Abstract
Background
Progressive oxidation of highly cross-linked ultra-high molecular weight (UHMPWE-X) liners is considered to be a risk factor for material failure in THA. Antioxidants such as vitamin E (alpha-tocopherol) (UHMWPE-XE) were supplemented into the latest generation of polyethylene liners. To prevent inhomogenous vitamin E distribution within the polymer, blending was established as an alternative manufacturing process to diffusion. The purpose of the present study was to investigate the in vivo wear behavior of UHMWPE-XE in comparison with conventional UHMWPE-X liners using virtual CAD-based radiographs.
Methods
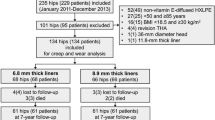
Until now, 94 patients from a prospective, randomized, controlled, multicenter study were reviewed at 5-year follow-up. Of these, 51 (54%) received UHMWPE-XE and 43 (46%) UHMWPE-X liners. Anteroposterior pelvic radiographs were made immediately after surgery and at 1 and 5 years postoperatively. The radiographs were analyzed using the observer-independent analysis software RayMatch® (Raylytic GmbH, Leipzig, Germany).
Results
The mean wear rate was measured to be 23.6 μm/year (SD 13.7; range 0.7–71.8 μm). There were no significant differences between the two cohorts (UHMWPE-X: 23.2 μm/year vs. UHMWPE-XE: 24.0 μm/year, p = 0.73). Cup anteversion significantly changed within the 1st year after implantation independent from the type of polyethylene liner [UHMWPE-X: 18.2–23.9° (p = 0.0001); UHMWPE-XE: 21.0–25.5° (p = 0.002)]. No further significant changes of cup anteversion in both groups were found between year 1 and 5 after implantation [UHMWPE-X (p = 0.46); UHMWPE-XE (p = 0.56)].
Conclusion
The present study demonstrates that the addition of vitamin E does not adversely affect the midterm wear behavior of UHMWPE-X. The antioxidative benefit of vitamin E is expected to become evident in long-term follow-up. Cup anteversion increment by 5° within the 1st year is likely a result of the released hip flexion contracture resulting in an enhanced posterior pelvic tilt. Therefore, a reassessment of target values in acetabular cup placement might be considered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultra-high molecular weight polyethylene (UHMWPE) was considered to be the gold standard for acetabular liners in total hip arthroplasty for a long time [1,2,3]. However, polyethylene wear debris-induced periprosthetic osteolysis remains one of the main causes for aseptic loosening in THA [2, 3]. The introduction of radiation cross-linking of polyethylene liners resulted in enhanced wear resistance (UHMWPE-X) [4,5,6]. Progressive oxidation of UHMPWE-X was considered to be another risk factor for material failure in THA [7]. In vitro studies demonstrated that stabilization of UHMWPE-X with antioxidants such as vitamin E (alpha-tocopherol) (UHMWPE-XE) increases resistance to oxidative stress [8]. However, vitamin E addition reduces cross-linking capacity of polyethylene [9,10,11] and particularly concentrations above 0.3 wt% (mass fraction) in the irradiated surface are considered to impair wear characteristics [12]. On the other hand, a defined amount of vitamin E (ranging between 0.1 and 1.0 wt%) in the unirradiated bulk extends the oxidative stability of UHMWPE-XE blends [13]. For clinical application, two different manufacturing processes were used to integrate vitamin E into UHMWPE:
The first method rests upon the diffusion of vitamin E into UHMWPE after radiation cross-linking. Cross-linking is not warped due to absence of vitamin E during consolidation. However, inhomogeneity of vitamin E content in the polyethylene liner due to diffusion process requires post-irradiation thermal treatment [10, 14, 15].
The alternative method is based on blending of vitamin E with UHMWPE resin powder prior to consolidation resulting in homogenous distribution of vitamin E in the polyethylene liner [16,17,18]. It is not yet proven whether these features have a positive effect on in vivo wear behavior and long-term implant survival.
A reliable and accurate measurement of low wear rates using conventional radiographs remains challenging [19]. Although the radiostereometric analysis (RSA) is widely accepted as the gold standard to measure the micromotions of implant components [20], traditional RSA requires the insertion of tantalum beads into the bone [21]. In 2012, a report about two new RSA methods which supersede marker beads using phantom devices was published. Both new RSA methods [scanned models (MB-RSA) and computer-generated geometrical shape models (EGS-RSA)] were validated as accurate and precise as the former gold standard for evaluation of polyethylene wear [22, 23]. Another well-established technique to assess wear and implant position is EBRA (Einzel-Bild-Roentgen-Analyse) [24, 25], a semiautomatic, graphical-based method evaluating standard anteroposterior radiographs without requiring additional means at exposure (e.g. markers) [26]. However, all graphical-based methods such as EBRA, ROMAN (Roentgen monogrammetric analysis) and HAS (hip analysis suite) do not reach the level of precision like RSA [27]. A recently developed innovative wear analysis system was used in this study. It is based on virtual computer-aided design (CAD)-based radiographic images without the need for a reference sphere. This method was validated for analysis of in vivo polyethylene wear [28].
In this prospective multicenter study, the 5-year in vivo wear behavior of UHMWPE-XE versus UHMWPE-X was evaluated by virtual CAD-based X-rays [29].
Materials and methods
In 2011, the VITAS (Vitelene® against Standard UHMWPE-X) study was established (PI second author) as a prospective, randomized, multicenter study to compare vitamin E-blended UHMWPE-XE (Vitelene®, sponsor: Aesculap AG, Tuttlingen, Germany) with UHMWPE-X. Six different orthopaedic departments in Germany participated and recruited 400 patients between 2011 and 2015. The follow-up period is scheduled up to 15 years. Patients of both genders with the indication for a primary cementless total hip arthroplasty due to hip osteoarthritis were recruited for this trial. Exclusion criteria were significant increased anesthetic risk (ASA IV), tumors, drug or alcohol abuse as well as immunosuppressive therapy, infections, fractures, previous surgeries at the affected hip, poor bone quality and relevant deformities (leg length differences > 30 mm, offset reductions > 30 mm). Informed written consent according to the Declaration of Helsinki was obtained from every patient prior to surgery. The study was approved by the local ethics committee (#11-4845-BO) and registered on Clinicaltrials.gov (#NCT01713062).
Implants and intervention
Vitelene® is a vitamin E-blended highly cross-linked polyethylene liner. It is produced by compression molding technique from a compound of 0.1% vitamin E and polyethylene polymers. Subjects were randomly assigned to obtain either a Vitelene® liner or a conventional UHMWPE-X (remelted, cross-linking by γ-irradiation [75 kGy], sterilization: ethylene oxide) liner. The acetabular component was a cementless fixed Plasmacup DC® (Aesculap). It is a hemispheric cup with a microporous titanium coating (Plasmapore®). The type of femoral stem and the surgical approach was defined by the orthopaedic surgeon, but limited to four different stem types (Metha®, Excia®, Bicontact®, TRJ®, all Aesculap). To evade effects of different head materials, Al2O3 ceramic heads (Biolox® Ceramtec, Plochingen, Germany) with 32 or 36 mm diameter were regularly used. Postoperatively, all patients received physiotherapy and were mobilized 1 day after surgery. The further postoperative treatment schedule was left over to the study centers. The amount of weight bearing was dependent on individual decision of each surgeon and varied from full weight bearing immediately after surgery down to 20 kg weight bearing for 6 weeks.
Wear analysis
The 5-year wear analysis of 94 patients of the multicenter study (VITAS) was performed using the innovative software RayMatch® (Raylytic, Leipzig, Germany). The software enables to measure highly precise radiographic parameters and femoral head penetration. For this analysis, CAD data of the prosthetic components are crucial and were provided by the manufacturer of the prosthetic components (Aesculap AG, Tuttlingen, Germany). For method validation, virtual pelvis X-rays of 21 patients from 2 study centers (Vitelene® cohort with vitamin E: 12 patients, UHMWPE-X cohort without vitamin E: 9 patients) were made 1 and 5 years after surgery [27]. The radiographic images were analyzed to determine polyethylene wear, cup inclination and cup anteversion. The software works completely automatically and is independent from any other factors (e.g. investigators experiences, X-ray technique, type of implant, etc.). It is based on the creation of virtual images of the prosthetic components via computer simulation. In a first step, voxels with an isotropic edge length of 0.15 mm are discretized. Attenuation coefficients are assigned to the voxels depending on the prosthetic material. The simulation model consists of a projection surface (simulating the detector), an X-ray emitter (simulating the X-ray tube) and the prosthetic component. Emanating from an X-ray source, vectors are calculated reaching the pixels on the projection surface. The next step is to determine the resulting intensity of the radiation along the vectors using the Lambert–Beer law. The calculated intensity per virtual pixels constitutes grey values creating a realistic simulated image of the prosthesis. In the next step, the simulated image (“digitally reconstructed radiograph”, DRR) is compared with the real image by creating gradient-based difference images. Subsequently, the accordance of DRR and real images is determined utilizing a cross-correlation. The position and the alignment of the implant components is adjusted iteratively in all six directions aiming at a maximum accordance with the real image. The data processing was performed by powerful hardware (PC with Intel® Core™ i5-4570 CPU and graphic card Nvidia® GTX1080). The mean absolute error of 4.0 μm with a standard deviation of 7.1 μm was attributed to different positions in space. Summing up, the RayMatch® method is equal to the most accurate method (RSA) without the disadvantage of the insertion of tantalum beads compared to the traditional RSA [27, 28] (Figs. 1, 2).
Creation of virtual images of the prosthetic components via computer simulation. The simulation model consists of a projection surface (simulating the detector), an X-ray emitter (simulating the X-ray tube) and the prosthetic component. Emanating from an X-ray source, vectors are calculated reaching the pixels on the projection surface
The cup inclination (CupInc) was measured as the angle between the cup surface and a horizontal reference line using a 2D–3D registration between the patient-specific cup CAD model and the X-ray. The cup anteversion (CupAnt) was measured as the angle between the cup surface against the cup symmetry axis in the frontal plane using a 2D–3D registration between the patient-specific cup CAD model and the X-ray. The hip implant wear (HIW) was measured between the hip cup and the hip head at the specified follow-up time point using a 2D–3D registration between the patient-specific cup and head CAD model and the X-ray. The parameter is determined in micrometers and expressed as the average wear rate per year.
Statistical analysis
For descriptive statistics of the data, means and standard deviations (SD) are provided. The Shapiro–Wilk test was used to test for normality of the sample. The Student’s t test was used for comparison of paired samples with a normal distribution of pre- and postoperative means. In cases of not normally distributed means, the Wilcoxon signed-rank test was used. p values < 0.05 were considered significant. The software SPSS®19 (SPSS Inc. Headquarters, Chicago, Illinois, USA) was used to carry out statistical analysis.
Results
From 400 included probands, 84 left the study. In ten patients (2.5%), revision surgery was necessary, of which seven occurred in UHMWPE-X group. The reasons for revision were postoperative hemorrhage (n = 3), stem loosening (2), periprosthetic fracture (2), aseptic cup loosening (1), periprosthetic infection (1) or dislocation (1). At a minimum follow-up of 5 years, reasonable X-rays for wear analysis (postoperative, 1- and 5-year follow-up X-rays) were available from 94 patients. Among the 94 patients, no significant differences in any demographic characteristics between the UHMWPE-X (n = 43) and UHMWPE-XE groups (n = 51) were noted. In the UHMWPE-X group, gender ratio was 22–28 (male to female) and 31–37 in the UHMWPE-XE group, respectively. The mean age at the time of surgery was 62.3 years (range 34–75 years) and did not differ between the groups (p = 0.22) as it was for the BMI (mean 28.5, range 18–41, p = 0.26 between groups). In all patients, the diameter of the femoral modular head was 32 mm. Due to poor X-ray quality in one of the study centers, the HIW could not be analyzed in 12 images (UHMWPE-XE n = 8; UHMWPE-X n = 4). Therefore, the images of 82 patients were evaluated for femoral head penetration. In 35 (UHMWPE-X: n = 17; UHMWPE-XE: n = 18) of these patients, a Metha® short stem was applied. In 42 patients (UHMWPW-X: n = 21; UHMWPE-XE: n = 21), a Bicontact® straight stem was used. Four patients (UHMWPE-X: n = 2; UHMWPE-XE: n = 2) received a Excia® T stem system and in one case (UHMWPE-X) a trochanter preserving TRJ® stem was used. In total, mean femoral head penetration was similar between both cohorts (UHMWPE-X = 116 μm; UHMWPE-XE = 120 μm; p = 0.73). The mean femoral head penetration was 23.2 μm/year (range 0.7–71.8 μm) in the UHMWPE-X group and 24.0 μm/year (range 0.7–67.8 μm) in the UHMWPE-XE group at 5-year follow-up. In the 1st year, no femoral head penetration was detected in both groups. Using four different stem types, there were no significant differences in wear rates between the cohorts [Metha® 24.6 µm/year (0.7–71.8); TRJ® 32.3 µm/year; Bicontact® 22.2 µm/year (0.7–61.9) and Excia® 25.8 µm/year (13.1–38.2)]. Within the two major subgroups, no significant difference could be identified using the two inlay types [Metha®: UHMWPE-X vs. UHMWPE-XE: 24.1 µm/year (0.7–71.8) vs. 25.4 (8.1–67.8) (p = 0.81); Bicontact®: UHMWPE-X versus UHMWPE-XE: 23.3 µm/year (6.2–61.5) vs. 21.5 µm/year (0.7–41.8) (p = 0.65)] (Tables 1, 2).
From surgery to 5-year follow-up, the cup inclination changed from 40.9° (range 29.9–52.7°) to 41.2° (range 29.1–54.1°) in the UHMWPE-X group (p = 0.82) and from 39.5° (range 28.9°–52.2°) to 39.8° (range 28.4°–53.3°) in the UHMWPE-XE group (p = 0.77) (Tables 3, 4).
The postoperatively measured cup anteversion significantly increased within the 1st year after implantation independent from the type of polyethylene liner, from 18.2° (range 7.3°–33.2°) to 23.9° (range 10.3°–44.2°) in the UHMWPE-X group (p = 0.0001) and from 21.0° (range 6.0°–37.4°) to 25.5° (range 10.9°–46.1°) in the UHMWPE-XE group (p = 0.002), respectively. From year 1 to year 5 after implantation, no further significant changes of cup anteversion in both groups were found (UHMWPE-X, p = 0.46; UHMWPE-XE, p = 0.56) (Tables 5, 6).
Discussion
Strong efforts have been made to improve material properties and to reduce wear of polyethylene in THA [2, 8, 9, 35]. Cross-linking of conventional polyethylene was a milestone to improve wear characteristics in THA. Since then, a precise measurement of low wear rates became challenging in conventional radiographs making it difficult for comparative studies. Especially in short and midterm follow-up, semiautomatic methods such as EBRA, ROMAS and HAS [27] have specific disadvantages and are inferior to RSA [28]. We used a novel, non-invasive and investigator independent wear analysis technique. In our study, the two cohorts (UHMWPE-X vs. UHMWPE-XE) showed no significant differences in wear rates within 5-year follow-up. The stem design had no significant impact on the wear behavior of the polyethylene inlay. In both groups, the polyethylene wear was substantially below the threshold for osteolysis induction of 100 μm/year [30]. This fits with most reports in the literature about vitamin E-supplemented polyethylene liners. Apart from Scemama et al. [31], no author described significant differences between vitamin E-supplemented and conventional polyethylene liners [31,32,33,34,35,36]. In Table 7, there is an overview about the current data in the literature.
Interestingly, the anteversion of the acetabular cup increased within the 1st year after implantation independent from the material of the acetabular liner (+ 5.7° UHMWPE-X vs. + 5.1° UHMWPE-XE; p = 0.42). It is known that permanent and stable osseointegration of titanium cups occurs during the early postoperative period [37, 38]. Therefore, a migration of the cup towards flexion must be taken into consideration in the analysis of our results. Yet, there is no gold standard for measuring the acetabular anteversion [39]. Due to automated measurement, the RayMatch® technique has the advantage to be non-dependent on investigators’ experience [28]. However, the RayMatch® technique does not take differences in the pelvic tilt into account. In conventional two-dimensional radiographs, the variation of pelvic tilt may lead to an incorrect measurement of the acetabular orientation [40]. For inclination, the error is vanishingly small [41], but anteversion is highly susceptible to changes in pelvic tilt [42].
A major strength of our study is the design as a prospective, randomized multicenter trial. To our knowledge, this is the second report on in vivo wear behavior of vitamin E-blended polyethylene in total hip arthroplasty. The application of the recently validated, virtual computer-aided design (CAD)-based analysis tool ensures a reliable, observer-independent measurement of radiographic parameters. However, our study has several limitations. Of the 400 patients included, 84 patients have withdrawn their consent to participate in the study. Furthermore, among the 94 patients who were examined at 5-year follow-up, 12 cases could not be analyzed regarding HIW due to inadequate image quality.
In summary, there was no significant difference in midterm wear behavior between UHMWPE-X and UHMWPE-XE.
Conclusion
The addition of vitamin E does not significantly affect wear behavior of UHMWPE-X at 5-year follow-up. At 10-year follow-up, we expect superior wear behavior of UHMWPE-XE due to reduced oxidative embrittlement. Interestingly, cup anteversion increased by nearly 5° within the 1st year after implantation and is expected to be functional. Therefore, a reassessment of target values in acetabular cup placement might be considered.
Availability of data and materials
All patient-related data were collected by file research from the archives of the participating centers.
References
Beaulé PE, Campbell P, Mirra J, Hooper JC, Schmalzried TP (2001) Osteolysis in a cementless, second generation metal-on-metal hip replacement. Clin Orthop Relat Res 386:159–165
Muratoglu OK, Kurtz S (2002) Alternate bearing surfaces in hip replacement. In: Sinha R (ed) Hip replacement. Current trends and controversies. CRC Press, New York, pp 1–46
Oral E, Wannomae KK, Rowell SL, Muratoglu OK (2007) Diffusion of vitamin E in ultra-high molecular weight polyethylene. Biomaterials 28(35):5225–5237 (Epub 2007 Sep 19)
Kawakage NOS, Ogihara T (1997) Poly (vinyl alcohol)-clay and poly (ethylene oxide)-clay blends prepared using water as solvent. J Appl Polym Sci 66:573–581
Digas G, Karrholm J, Thanner J, Malchau H, Herberts P (2004) Highly cross-linked polyethylene in total hip arthroplasty: randomized evaluation of penetration rate in cemented and uncemented sockets using radiostereometric analysis. Clin Orthop. 429:16
Nivbrant B, Roerhl S, Hewitt B, Li M. In vivo wear and migration of high cross linked poly cups: a RSA study. In: 49th Annual Orthopaedic Research Society; 2003; New Orleans; 2003. p. 358
MacDonald D, Sakona A, Ianuzzi A et al (2011) Do first-generation highly crosslinked polyethylenes oxidize in vivo? Clin Orthop Relat Res 469:2278–2285
Oral E, Christensen S, Malhi A, Wannomae K, Muratoglu O (2006) Wear resistance and mechanical properties of highly crosslinked UHMWPE doped with vitamin E. J Arthroplasty 21(4):580–591
Bracco P, Oral E (2011) Vitamin E-stabilized UHMWPE for total joint implants: a review. Clin Orthop Relat Res 469:2286–2293
Oral E, Wannomae KK, Hawkins N, Harris WH, Muratoglu OK (2004) Tocopheroldoped irradiated UHMWPE for high fatigue resistance and low wear. Biomaterials 25:5515–5522
Grupp TM, Holderied M, Mulliez MA, Streller R, Jäger M, Blömer W, Utzschneider S (2014) Biotribology of a vitamin E-stabilized polyethylene for hip arthroplasty—influence of artificial ageing and third-body particles on wear. Acta Biomater 10(7):3068–3078. https://doi.org/10.1016/j.actbio.2014.02.052(Epub 2014 Mar 12)
Oral E, Godleski Beckos C, Malhi AS, Muratoglu OK (2008) The effects of high dose irradiation on the cross-linking of vitamin E-blended ultrahigh molecular weight polyethylene. Biomaterials 29(26):3557–3560. https://doi.org/10.1016/j.biomaterials.2008.05.004(Epub 2008 Jun 2)
Xu JZ, Wannomae KK, Muratoglu OK, Oral E (2018) Increased oxidative protection by high active vitamin E content and partial radiation crosslinking of UHMWPE. J Orthop Res 36(7):1860–1867. https://doi.org/10.1002/jor.23835(Epub 2018 Jan 3)
Oral E, Ghali BW, Rowell SL, Micheli BR, Lozynsky AJ, Muratoglu OK (2010) A surface crosslinked UHMWPE stabilized by vitamin E with low wear and high fatigue strength. Biomaterials 31(27):7051–7060. https://doi.org/10.1016/j.biomaterials.2010.05.041(Epub 2010 Jun 25)
Oral E, Muratoglu OK (2011) Vitamin E diffused, highly crosslinked UHMWPE: a review. Int Orthop 35(2):215–223. https://doi.org/10.1007/s00264-010-1161-y(Epub 2010 Dec 1)
Parth M, Aust N, Lederer K (2002) Studies on the effect of electron beam radiation on the molecular structure of ultra-high molecular weight polyethylene under the influence of alpha-tocopherol with respect to its application in medical implants. J Mater Sci Mater Med 13(10):917–921
Oral E, Greenbaum E, Malhi A, Muratoglu O (2005) Characterization of blends of α-Tocopherol with UHMWPE. Biomaterials 26:6657–6663
Oral E, Neils AL, Rowell SL, Lozynsky AJ, Muratoglu OK (2013) Increasing irradiation temperature maximizes vitamin E grafting and wear resistance of ultrahigh molecular weight polyethylene. J Biomed Mater Res B Appl Biomater 101(3):436–440. https://doi.org/10.1002/jbm.b.32807(Epub 2012 Oct 31)
Ayers DC, Greene M, Snyder B et al (2015) Radiostereometric analysis study of tantalum compared with titanium acetabular cups and highly cross-linked compared with conventional liners in young patients undergoing total hip replacement. J Bone Joint Surg Am 97:627–634
Selvik G (1989) Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand 232:1–51
Bottner F, Su E, Nestor B, Azzis B, Sculco TP, Bostrom M (2005) Radiostereometric analysis: the hip. HSS J. 1(1):94–99. https://doi.org/10.1007/s11420-005-0114-2
Stilling M, Kold S, de Raedt S, Andersen NT, Rahbek O, Søballe K (2012) Superior accuracy of model-based radiostereometric analysis for measurement of polyethylene wear: a phantom study. Bone Joint Res. 1(8):180–191. https://doi.org/10.1302/2046-3758.18.2000041(Print 2012 Aug)
Troelsen A, Greene ME, Ayers DC, Bragdon CR, Malchau H (2015) A Novel method for assessment of polyethylene liner wear in radiopaque tantalum acetabular cups: clinical validation in patients enrolled in a randomized controlled trial. J Arthroplasty 30(12):2354–2359. https://doi.org/10.1016/j.arth.2015.06.050(Epub 2015 Jul 2)
Langton DJ, Sprowson AP, Mahadeva D, Bhatnagar S, Holland JP, Nargol AV (2010) Cup anteversion in hip resurfacing: validation of EBRA and the presentation of a simple clinical grading system. J Arthroplasty 25(4):607–613. https://doi.org/10.1016/j.arth.2009.08.020(Epub 2009 Dec 21)
Biedermann R, Krismer M, Stöckl B, Mayrhofer P, Ornstein E, Franzén H (1999) Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement. Einzel-Bild-Röntgen-Analyse-femoral component analysis. J Bone Joint Surg Br. 81(2):266–272
Krismer M, Bauer R, Tschupik J, Mayrhofer P (1995) EBRA: a method to measure migration of acetabular components. J Biomech 28(10):1225–1236
Callary SA, Solomon LB, Holubowycz OT et al (2017) Accuracy of methods to measure femoral head penetration within metal-backed acetabular components. J Orthop Res 35:988–996
Haversath M, Klebingat S, die VITAS-Gruppe, Jäger M (2018) Endoprosthetic wear analysis using virtual CAD-based radiographs. Orthopade. 47(10):811–819. https://doi.org/10.1007/s00132-018-3602-z(Article in German)
Jäger M, Van Wasen A, Warwas S et al (2014) A multicenter approach evaluating the impact of vitamin e-blended polyethylene in cementless total hip replacement. Orthop Rev (Pavia) 6:5285
Dowd JE, Sychterz CJ, Young AM, Engh CA (2000) Characterization of long-term femoral-head-penetration rates. Association with and prediction of osteolysis. J Bone Joint Surg Am. 82(8):1102–1107
Scemama C, Anract P, Dumaine V, Babinet A, Courpied JP, Hamadouche M (2017) Does vitamin E-blended polyethylene reduce wear in primary total hip arthroplasty: a blinded randomised clinical trial. Int Orthop 41(6):1113–1118. https://doi.org/10.1007/s00264-016-3320-2(Epub 2016 Nov 4)
Salemyr M, Muren O, Ahl T, Bodén H, Chammout G, Stark A, Sköldenberg O (2015) Vitamin-E diffused highly cross-linked polyethylene liner compared to standard liners in total hip arthroplasty. A randomized, controlled trial. Int Orthop. 39(8):1499–1505. https://doi.org/10.1007/s00264-015-2680-3(Epub 2015 Jan 29)
Nebergall AK, Greene ME, Laursen MB, Nielsen PT, Malchau H, Troelsen A (2017) Vitamin E diffused highly cross-linked polyethylene in total hip arthroplasty at five years: a randomised controlled trial using radiostereometric analysis. Bone Joint J. 99(5):577–584. https://doi.org/10.1302/0301-620x.99b5.37521
Galea VP, Connelly JW, Shareghi B, Kärrholm J, Sköldenberg O, Salemyr M, Laursen MB, Muratoglu O, Bragdon C, Malchau H (2018) Evaluation of in vivo wear of vitamin E-diffused highly crosslinked polyethylene at five years: a multicentre radiostereometric analysis study. Bone Joint J. 100(12):1592–1599. https://doi.org/10.1302/0301-620x.100b12.bjj-2018-0371.r1
Shareghi B, Johanson PE, Kärrholm J (2017) Wear of vitamin E-infused highly cross-linked polyethylene at five years. J Bone Joint Surg Am 99(17):1447–1452. https://doi.org/10.2106/JBJS.16.00691
Sillesen NH, Greene ME, Nebergall AK, Huddleston JI, Emerson R, Gebuhr P, Troelsen A, Malchau H (2016) 3-year follow-up of a long-term registry-based multicentre study on vitamin E diffused polyethylene in total hip replacement. Hip Int. 26(1):97–103. https://doi.org/10.5301/hipint.5000297(Epub 2015 Dec 11)
Beckmann NA, Jaeger S, Janoszka MB, Klotz MC, Bruckner T, Bitsch RG (2018) Comparison of the primary stability of a porous coated acetabular revision cup with a standard cup. J Arthroplasty 33(2):580–585. https://doi.org/10.1016/j.arth.2017.09.023(Epub 2017 Sep 20)
O’Rourke D, Al-Dirini RM, Taylor M (2018) Primary stability of a cementless acetabular cup in a cohort of patient-specific finite element models. J Orthop Res 36(3):1012–1023. https://doi.org/10.1002/jor.23709(Epub 2017 Sep 12)
Saka G, Altun G, Burc H, Aydogan M (2019) A new radiographic acetabular cup anteversion measurement method in total hip arthroplasty: a clinical study. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-019-02384-9(Epub ahead of print)
Muir JM, Vincent J, Schipper J, Govindarajan M, Paprosky WG (2018) Evaluation of tilt-correction of anteversion on anteroposterior pelvic radiographs in total hip arthroplasty. Cureus 10(5):e2647. https://doi.org/10.7759/cureus.2647
Tiberi JV III, Antoci V, Malchau H, Rubash HE, Freiberg AA, Kwon YM (2015) What is the fate of total hip arthroplasty (THA) acetabular component orientation when evaluated in the standing position? J Arthroplasty 30:1555–1560
Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D (1995) Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty 10:369–372
Sillesen NH, Greene ME, Nebergall AK, Nielsen PT, Laursen MB, Troelsen A, Malchau H (2015) Three year RSA evaluation of vitamin E diffused highly cross-linked polyethylene liners and cup stability. J Arthroplasty 30:1260–1264
Funding
The study is financially supported by B. Braun-Aesculap AG, Germany; Trial registration: NCT01713062. This study was supported by B. Braun Melsungen (AAG-G-H-1113).
Author information
Authors and Affiliations
Consortia
Contributions
All authors ensured that they had furnished a substantial contribution to the article and that they are in agreement with form and contents of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethics committee (11-4845-BO). The study was registered on Clinicaltrials.gov. The trial registration number is NCT01713062.
Consent to publish
All patients consented to publish personal data in an anonymised form.
Conflict of interest
The authors declare they have no conflict of interest.
Patient confidentiality
Data were protected according to the U.S. Health Insurance Portability and Accountability Act (HIPAA).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Busch, A., Jäger, M., Klebingat, S. et al. Vitamin E-blended highly cross-linked polyethylene liners in total hip arthroplasty: a randomized, multicenter trial using virtual CAD-based wear analysis at 5-year follow-up. Arch Orthop Trauma Surg 140, 1859–1866 (2020). https://doi.org/10.1007/s00402-020-03358-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03358-x