Abstract
Introduction
As the average age of society increases, so does the number of cases of fragility fractures of the pelvis (FFP). Magnetic resonance imaging (MRI) can visualise associated oedema and is thus the gold standard for diagnosing such fractures. MRI, however, is costly, not always available, and involves certain exclusion criteria. Dual-energy computed tomography (DECT) appears to be a promising alternative. It is unclear, however, whether it could be used for diagnosing FFP with similar sensitivity/specificity. The aim of our study was thus to compare conventional CT and DECT with MRI in cases of suspected FFP.
Materials and methods
A total of 46 patients with suspected FFP underwent MRI, CT and DECT scans. There were three comparison groups for each of these patients: conventional CT image analysis without dual-energy modification (Arm 1), DECT analysis (Arm 2) and MRI as the gold standard (Arm 3). Diagnosis and FFP classification were performed by a radiologist in random order and without clinical information. The sensitivity and specificity of conventional CT and DECT were calculated in comparison with MRI as the reference standard.
Results
With 100% sensitivity and specificity, DECT is on par with MRI when it comes to diagnosing fragility fractures of the pelvis and is superior to conventional CT (90.3% sensitivity, 100% specificity). In terms of classification as well, there were no differences between DECT and MRI. On conventional CT, on the other hand, 16 patients were classified differently than they were on MRI.
Conclusions
Our study shows DECT to be reliable and superior to conventional CT in terms of oedema detection and specific fracture classification in FFP. DECT thus combines the advantages of conventional CT (good visualisation of bone matter) and MRI (medullary cavity and visualisation of occult fractures).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The increasing relevance of fragility fractures of the pelvis in an ageing society
Fragility fractures or insufficiency fractures are defined by the World Health Organisation (WHO) as fractures caused by injury that would be insufficient to fracture normal bone [1]. Bone density gradually decreases throughout life. This is a physiological process that is accelerated especially by osteoporosis [1,2,3]. With demographic change and an ageing population, we can thus expect an increase in the incidence of fragility fractures [1, 4,5,6,7]. Apart from fragility fractures of the pelvis (FFP), pelvic injuries are primarily seen in connection with high-energy trauma (e.g., road accidents) in young patients. These differ in many respects from pelvic fractures caused by low-energy trauma, such as fragility fractures [1, 3, 6]. With age, however, bone strength decreases and the ligaments are eventually more stable than the cancellous bone. In contrast to pelvic ring fractures that are the result of high-energy trauma in young patients, pelvic fragility fractures in the elderly often leave the ligaments intact while the bone is unable to withstand the strain and breaks [3, 7, 8]. This also explains why bilateral sacral fractures occur relatively often in the geriatric patient collective, while in young patients they indicate a very severe injury mechanism [6].
Classification of pelvic ring fractures
The system used by the Orthopaedic Trauma Association (OTA) to classify pelvic fractures covers fracture types A, B and C and is based on the Tile classification method [9]. However, because of the particularities in geriatric patients, this classification does not provide a true picture of the severity of injury. Realising the need for a classification system specifically for fragility fractures of the pelvis, P. M. Rommens and A. Hofmann developed a new system [3, 4]. This established classification system distinguishes between four main groups (I–IV) based on specific anatomical features and increasing degree of instability.
Diagnosing insufficiency fractures
Patients with geriatric pelvic ring fractures usually complain of pain that is exacerbated by movement [1, 3, 8]. In many cases, the patient’s history of falls or trauma is not very instructive or the patient cannot remember it (result of minor trauma, dementia). Accurate diagnosis may be delayed as a result. There have even been cases where operations to treat back pain (e.g., lumbar decompression surgery) have been performed unnecessarily, with a sacral fracture later being identified as the primary source of the pain [10].
Conventional CT and MRI are the main established methods used to diagnose fragility fractures of the pelvis. While bony structures and, most importantly, cortical fracture lines can be clearly imaged with CT, MRI has the great advantage that it can clearly visualise the medullary cavity (bone marrow alterations like oedema/ bone bruise). A further advantage of MRI is that it does not expose the patient to radiation. MRI currently has the highest sensitivity when it comes to visualising bone marrow oedema in fluid-sensitive sequences. Fracture lines as a sign of cancellous fractures are easy to detect in native T1 sequences [5]. MRI has repeatedly been proven to have greater sensitivity (100%) than CT (65–75%) when it comes to visualising occult bone marrow alterations of the pelvis [11,12,13,14]. Nevertheless, for economic reasons (MRI takes longer and patients are often unable to lie still, limited availability/capacity, and higher cost), CT scans are usually performed first and MRI is only ordered if symptoms persist when an attempt is made to mobilise the patient and the results of the CT scan are normal. In routine clinical practice, however, the decision to order MRI depends very much on the treatment concept, and opinions on the use of MRI in cases of fragility fractures of the pelvis vary [5].
Conventional X-ray examinations today do not play an important role in diagnosing fragility fractures of the pelvis as significant dislocations, which would be visible on X-ray, are not common in this type of fracture [8, 15].
In the past, bone scintigraphy was described in some publications as a possible technique for diagnosing fragility structures of the pelvic ring [16]. Despite the high sensitivity of bone scintigraphy, however, the consensus today is that MRI is preferable [5, 9, 17].
We believe that dual-energy CT represents another diagnostic method for visualising bone marrow oedema as effectively as with MRI. Dual-energy CT is currently used, for example, to identify gouty tophi, to analyse urinary stones, and for metal artefact reduction [5].
The dual-energy CT method
With the Somatom Force CT scanner (Siemens, Erlangen, Germany), a modern DECT system approved for routine diagnostic procedures, we can visualise oedema with two tubes and rows of detectors that are offset at approximately 90° from each other. That way, two different energy spectra (e.g., 80 and 150 kV) can be acquired in one scan. How these two datasets are created varies depending on the equipment manufacturer. Owing to different degrees of X-ray attenuation of the different elements, the materials of the examined tissue can be decomposed and thus individual substances distinguished. With the virtual non-calcium (VNCa) technique, calcium is identified and then removed from cortical and cancellous bone in the image, making it possible to assess bone marrow oedema. Radiation exposure from DECT and scan duration are not higher with the new equipment than with conventional CT [5, 18].
Problem
It is unclear whether DECT could be used for diagnosing FFP (bone marrow alterations) with a sensitivity/specificity similar to that of MRI, and whether it is superior to established conventional CT. The aim of our retrospective clinical study was to compare, for the first time, DECT and conventional CT with MRI in terms of oedema detection and classification in patients with suspected FFP.
Material and methods
Study collective and inclusion/exclusion criteria
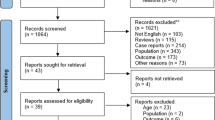
This retrospective pilot study included 46 patients (40 female, 6 male, 79.7 ± 9.2 years) who had presented in our clinic between 1 December 2015 and 1 June 2018 with a suspected fragility fracture of the pelvic ring. All patients underwent diagnostic DECT and MRI of the pelvis, the routine diagnostic method used in our clinic in the event of suspected insufficiency fracture of the pelvis. Inclusion and exclusion criteria are summarised in Table 1.
Study arms and evaluation of results
We generated three comparison groups for each patient. Arm 1 constituted CT images without computerised dual-energy modification, i.e., conventional CT examination. Additional CT scans and associated radiation exposure could thus be avoided. In Arm 2, the images from the DECT examination were modified with the virtual non-calcium (VNCa) technique to show bone marrow oedema. Arm 3 constituted MRI as the current gold standard for detecting oedema.
The images were evaluated using a set procedure. After the CT and MRI data sets had been acquired, they were assessed by a radiologist specialised in musculoskeletal injuries, in randomised order, blinded and without clinical information. The sensitivity and specificity of conventional CT and DECT were calculated by comparing results with those of MRI as the reference standard, using fourfold tables. In all three series, the FFP classification was used whenever a bone marrow alteration was detected to also examine differences in fracture classification: FFP Type I are isolated anterior pelvic ring fractures. FFP Type II lesions are non-displaced dorsal pelvic ring injuries, while FFP Type III are displaced unilateral and FFP IV are displaced bilateral dorsal pelvic ring injuries. The remaining degree of stability therefore decreases from I to IV. Each fracture type also has a sub-classification.
Three different MRI scanners were used for diagnostics in our clinic during the study period: the Magnetom Aera 1.5 T (Siemens, Erlangen, Germany), the Magnetom Harmony 1.0 T (Siemens, Erlangen, Germany), and the Achieva 3 T TX (Philips, Hamburg, Germany). The extent of oedema was examined with fluid-sensitive fat-saturated sequences (STIR/TIRM, PDw fatsat) and sometimes with additional T1w and T2w sequences.
Study registration and statistics
The study was approved by the Ethics Committee of Ulm (application no. 343/16) and registered in the German Clinical Trials Register (Trial ID: DRKS00010552). The calculations were made with Excel (Microsoft Office 2016) and QuickCalc (Graphpad Software). Sensitivity and specificity were calculated as the percentage of patients identified by each technique based on the standard of reference (MRI) with a confidence interval (CI) of 95%. For statistical comparisons of diagnostic ability between DECT and conventional CT, the sensitivity and specificity were compared using a paired proportion test (the McNemar test). A CI of 5% was used here.
Results
Comparison of conventional and dual-energy CT with MRI in terms of detection of FFP
In 31 of the 46 (67.4%) patients, at least one bone marrow alteration or fracture of the pelvis was found on MRI. Accordingly, no pelvic alteration was found in 15 patients (32.6%). In the 31 patients with a pathology, a total of 77 bone marrow alteration sites were identified on MRI. These were distributed as follows: 45.5% (35) were alterations of the sacrum, 27.3% (21) were alterations of the superior pubic ramus, and 27.3% (21) were alterations of the inferior pubic ramus.
In the DECT scan too, at least one alteration was found in 31 patients and no alteration was found in 15 patients. The results were also the same in terms of the total number of bone marrow alteration sites and their distribution, with exactly the same number of pathologies identified in the dorsal pelvic ring, in the superior pubic ramus and in the inferior pubic ramus as on MRI. This means that a total of 77 pathologies were diagnosed both on MRI and on DECT.
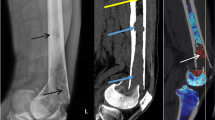
On conventional CT, at least one pelvic pathology was found in 28 patients (60.9%), and no alteration was found in 18 of the 46 patients (39.1%). A total of 59 bone marrow alterations were identified with this examination method. Of these, 28.8% (n = 17) were in the dorsal pelvic ring, 35.6% (n = 21) in the superior pubic ramus, and 35.6% (n = 21) in the inferior pubic ramus (Figs. 1 and 2).
Using fourfold tables, for the dual-energy CT scans we calculated a sensitivity of 100% (CI 89.0–100%), because all 31 patients with a pathology were identified as such. There were no false-positive diagnoses (100% specificity, CI 79.6–100%).
Conventional CT achieved a sensitivity of 90.3% (CI 75.1–96.7%) when compared with MRI, as no pathology was identified in three patients who had been diagnosed with one on MRI. Conventional CT achieved a specificity of 100% (CI 82.4–100%).The p value for the McNemar test was 0.2482, showing that DECT had no significantly enhanced sensitivity for finding pathologies compared with CT.
The results of both conventional CT and DECT were the same as those of MRI when it came to detecting ventral pelvic ring alterations (100% sensitivity and specificity in the “ventral pelvic ring fractures” subgroup).
In diagnosing dorsal pelvic ring injuries, conventional CT had a sensitivity of 68.0% (CI 48.4–82.8%). Eight out of 25 diagnoses were false negatives (32%), i.e., pathologies were not detected. Specificity remained unchanged at 100% (CI 84.5–100%).
Evaluation of DECT data also showed 100% sensitivity (CI 86.7–100%) when it came to detecting dorsal pelvic ring alterations. All 25 patients diagnosed with dorsal pelvic ring pathology on MRI were also diagnosed with these alteration on DECT. DECT also achieved the same specificity of 100% as MRI in this subgroup (CI 84.5–100%). The p value for the McNemar test was 0.0133, showing that DECT had significantly enhanced sensitivity when it came to dorsal pelvic ring alterations compared with CT.
Comparison of conventional and dual-energy CT with MRI in terms of correct classification of FFP
Classification of the bone marrow alterations detected on MRI revealed the following distribution pattern: There were six unilateral ventral pelvic ring pathologies (Type Ia) in our series (19.4%). No bilateral ventral pelvic ring alteration (Type Ib) was found. Type IIa, an isolated dorsal injury, was detected two times in our study (6.5%). A compression injury of the ventral lateral mass of the sacrum and accompanying instability of the ventral pelvic ring (Type IIb) occurred six times (19.4%). A non-displaced total fracture of the sacrum or ilium or a sacroiliac injury with accompanying instability of the ventral pelvic ring is classified as Type IIc and was diagnosed four times in our series (12.9%). Non-displaced lesions of the dorsal pelvic ring (Type II) were thus the most common pathologies in this study (12/31 = 38.7%). FFP Types IIIa (displaced ilium fracture) and IIIb (displaced unilateral sacroiliac disruption) were not observed in our series. Type IIIc (displaced unilateral sacral fracture) was diagnosed only three times in this group (9.7%). Displaced bilateral dorsal pelvic ring injuries (Type IV) were diagnosed a total of ten times in this series (10/31 = 32.2%). There were no bilateral iliac fractures or sacroiliac disruptions (FFP type IVa). Type IVb, a spinopelvic dissociation containing a bilateral vertical injury of the lateral mass of the sacrum with a horizontal component that connects them (H-shaped fracture), was diagnosed eight times (25.8%). A combination of different dislocated instabilities in the dorsal pelvic ring is classified as Type IVc and was diagnosed two times in our series (6.5%).
The results of the comparison of conventional CT with MRI as the gold standard in terms of classification are shown in Fig. 3. A total of 16 patients (34.8%) were classified differently based on conventional CT than they were based on MRI. Fracture classification based on DECT, on the other hand, was identical to the results of MRI (Fig. 4).
Comparison of FFP classification after magnetic resonance imaging (MRI) grey columns with that after conventional computed tomography (CT). Patients whose classification after CT was the same as after MRI are shown in green. Those who were classified differently on conventional CT are shown in the corresponding colours (see arrow as an example: the three patients marked in striped turquoise were classified as IIb on MRI, but as Ia on CT)
Discussion
The aim of our retrospective clinical study was to examine dual-energy CT as a potential new method for diagnosing fragility fractures of the pelvic ring. To this end, we compared dual-energy CT with MRI as the gold standard in terms of detecting bone marrow oedema. To examine possible advantages of DECT over conventional CT, the latter was also compared with MRI.
We were able to show that DECT (100% sensitivity when examining the dorsal pelvic ring) is superior to conventional CT (68% sensitivity when examining the dorsal pelvic ring) when it comes to detecting sacral pathologies in geriatric patients. The p value for the McNemar test was 0.0133, showing that DECT had significantly enhanced sensitivity for finding sacral pathologies compared with CT.
According to our findings, dual-energy CT (100% sensitivity, 100% specificity) achieves a result that is same to that of MRI (current gold standard) when it comes to diagnosing pathologies (ventral and dorsal) of the pelvis.
The methods commonly used in everyday clinical practice to diagnose fragility fractures of the pelvis are conventional CT and if the results of that are still ambiguous MRI, the latter being an effective method to detect oedema in FFP. While CT can clearly visualise bony structures and, most importantly, cortical fracture lines, MRI has the major advantage that it can be used to assess the medullary cavity [5].
Since ventral pelvic ring injuries are often accompanied by a cortical disruption, such injuries are likely to be clearly visible on conventional CT. Our study confirms this. Sensitivity and specificity were both 100% when it came to pathologies of the ventral pelvic ring. Assessing the dorsal pelvic ring with conventional CT has its limits, however, as fragility fractures of the sacrum often remain occult because they are characterised not so much by cortical disruption but rather by compression lines or bone oedema [17, 18]. This explains the lower sensitivity of conventional CT (68%) in our study when it came to assessing dorsal pathologies of the pelvic ring, which other studies have confirmed [11,12,13,14]. Cabarrus et al. found out, that in 98% of their patients insufficiency fractures of the pelvis or proximal femur could be detected with MRI, whereas with the CT this was possible in 53% of the patients [11].
This is where the strength of MRI currently lies, as it can visualise such occult fractures by visualising oedema [5, 6, 8]. Therefore some colleagues perform MRI examinations without CT when FFP was suspected. In some hospitals, however, MRI is not the standard for this indication because availability is limited, cost is relatively high, the exam itself takes a long time and geriatric patients who are in pain struggle to lie still for such long periods, and relative and absolute contraindications (e.g., pacemaker) prohibit the examination. Our working group has previously described the importance of MRI on the basis of a recent survey of the German expert group on pelvic surgery, the “AG Becken III” of the German Trauma Society as well as the advantages and disadvantages of established imaging methods in relation to FFP [5, 18].
But what is the meaning of a bone bruise detected on MRI without a cortical disruption on CT? The bone bruise represents a hemorrhagic zone in the bone. The histopathological correlate of this are microfractures of the spongy bone as well as oedema and bleeding in the fatty marrow [19, 20]. So bone bruise is a pathological situation. If the regeneration processes of the bone stay overwhelmed, it takes a few weeks until periosteal reactions or cortical interruption become visible in CT. If there is no cure, the fracture becomes radiologically visible after 2–3 weeks [21]. However, it is possible that a bone bruise heals without cortical interruption if the underlying pathological factors (overload, pathological bone metabolism) are corrected [22].
Oedema in the bone is generally associated with pain [23]. The painfulness under physical stress usually increases. In our opinion, it is necessary to exclude a non-displaced fracture or bone oedema as a potential precursor of a fracture, even if there is no fracture diagnosed on conventional CT. Spiegl et al. came to the same conclusion in their overview study about fragility fractures of the os sacrum [22]. Although the two papers cited outlined the potential of DECT (established areas of application include the identification of gouty tophi, analysis of urinary stones and metal artefact reduction) for diagnosing FFP, there has been no clinical comparative study to compare conventional CT, DECT, and MRI [5, 18].
In our study, we were able to show for the first time that DECT is a very suitable method for detecting bone marrow oedemas of the pelvis. With a sensitivity and specificity of 100%, a DECT scan on its own is enough to diagnose pathologies of the pelvic ring. It combines the advantages of both MRI and CT with radiation exposure that is no greater than that of conventional CT—with the same scan duration. DECT is superior to the latter in particular in terms of assessing the biomechanically relevant dorsal pelvic ring (Fig. 5 a, b, c).
a A fracture of the left lateral mass is visible on conventional computed tomography (CT). b On dual-energy computed tomography (DECT), bone marrow oedema (green) is now visible in the right and left lateral mass, with a transverse component (H sign). c On magnetic resonance imaging (MRI), the bone marrow oedema in the right and left lateral mass is visible, too
One disadvantage of DECT worth noting, however, is the fact that it does not differentiate between oedematous bone marrow and haematopoietic bone marrow. In the “blood-rich” marrow of a young patient collective in particular, this can lead to false positives on DECT. The patient collective should thus be carefully selected to achieve conclusive results. The ideal conditions for DECT are inherent in the osteoporotic bone of an elderly person with extensive bone marrow adiposity and as such are usually present in fragility fractures [5]. This is why we decided to choose a patient collective with a minimum age of 55 and cannot recommend using the method in young people. This limitation of dual-energy CT is not clinically relevant, however, because pelvic fractures in young patients are mainly the result of high-speed trauma, in which case both dorsal and ventral pelvic ring fractures appear as cortical step-off with accompanying tissue damage and can therefore be detected with conventional CT.
We believe it is remarkable that DECT not only is effective in detecting fractures but also has significant advantages over conventional CT when it comes to correct fracture classification. After all, classification based on DECT assessment was identical to MRI classification results.
On conventional CT, on the other hand, the pathologies of 16 patients were classified differently than they were on MRI (34.8%), primarily in the area of the dorsal pelvic ring, as previously discussed. Bilateral sacral abnormities in particular were either diagnosed as a unilateral fracture (6/8 = 75%) or not at all (2/8 = 25%). With isolated unilateral dorsal pelvic fractures (Type IIa) as well, 0 of 2 fractures were identified correctly on conventional CT. These observations are especially significant because geriatric patients in particular sustain bilateral dorsal pelvic ring injuries more frequently than young people. There is also the risk of incorrect treatment decisions being made as a result of incorrect classification [24].
Regarding the difference between bone bruise/ oedema and fractures another limitation of our retrospective and non-prospective study is that Rommens and Hofmann did not use MRI but conventional CT to establish the FFP classification [3, 4]. In our study, however, we decided to use MRI as a standard of comparison as it is proven to have a higher sensitivity than conventional CT [11,12,13,14]. What is more, the distribution pattern of the fracture types is comparable to that found by Rommens and Hofmann. Thus, we can assume that our patient collective is representative of the expected FFP distribution pattern.
As a consequence, DECT signal alterations in this study led to changes in the FFP classification, which, however, is based on CT and which describes fractures, which are visible in conventional CT scans, only. From our point of view, it is therefore much more important to mention that in FFP injuries, bone marrow alterations may be detected with same accuracy by both DECT and MRI, which may correspond to an occult fracture or oedema, which is possible to develop into a more unstable fracture type.
In summary, DECT appears to be a promising diagnostic method for assessing FFP. This retrospective analysis confirms the positive experience in our hospital, where DECT has since replaced the combination of conventional CD and additional MRI scans where required. For our working group, the major advantages are that we can now diagnose an FFP with a single scan instead of possibly two, with the same availability and level of radiation exposure as conventional CT yet the same 100% sensitivity and specificity of MRI, even outside of regular MRI operating hours. The next step should be a prospective study to verify our results.
References
Oberkircher L, Ruchholtz S, Rommens PM, Hofmann A, Bücking B, Krüger A (2018) Osteoporotic pelvic fractures. Dtsch Arztebl Int 115:70–80
Fuchs T, Rottbeck U, Hofbauer V, Raschke M, Stange R (2011) Pelvic ring fractures in the elderly. Underestimated osteoporotic fracture Der Unfallchirurg 114:663–670
Rommens PM, Wagner D, Hofmann A (2012) Osteoporotic fractures of the pelvic ring. Zeitschrift für Orthopädie und Unfallchirurgie 150:107–120
Rommens PM, Hofmann A (2013) Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Inj Int J Care Inj 44:1733–1744
Hackenbroch C, Riesner HJ, Lang P, Stuby F, Danz B, Friemert B, Palm HG, AG Becken III der Deutschen Gesellschaft für Unfallchirurgie (2016) Dual energy CT: a novel technique for diagnostic testing of fragility fractures of the pelvis. Zeitschrift für Orthopädie und Unfallchirurgie 155:27–34
Ruchholtz S, Bücking B, Schulz R-J (2016) Becken. Alterstraumatologie, 1st edn. Thieme Verlagsgruppe, Stuttgart, pp 296–318
Lourie H (1986) Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA 248:715–717
Stuby FM, Schaffler A, Haas T, Konig B, Stockle U, Freude T (2013) Insufficiency fractures of the pelvic ring. Der Unfallchirurg 116:351–366
Tile M (1988) Pelvic ring fractures: should they be fixed? J Bone Jt Surg 70:1–12
Imhof H, Halpern B, Herneth A (2006) Pareto-Reihe Radiologie Wirbelsäule. Thieme Verlagsgruppe, Stuttgart
Cabarrus MC, Ambekar A, Lu Y, Link TM (2008) MRI and CT of insufficiency fractures of the pelvis and the proximal femur. Am J Roentgenol 191:995–1001
Soles GL, Ferguson TA (2012) Fragility fractures of the pelvis. Curr Rev Musculoskel Med 5:222–228
Henes FO, Nuchtern JV, Groth M, Habermann CR, Regier M, Rueger JM, Adam G, Grossterlinden LG (2012) Comparison of diagnostic accuracy of magnetic resonance imaging and multidetector computed tomography in the detection of pelvic fractures. Eur J Radiol 81:2337–2342
Grangier C, Garcia J, Howarth NR, May M, Rossier P (1997) Role of MRI in the diagnosis of insufficiency fractures of the sacrum and acetabular roof. Skelet Radiol 26:517–524
Peh WC, Khong PL, Yin Y, Ho WY, Evans NS, Gilula LA, Yeung HW, Davies AM (1996) Imaging of pelvic insufficiency fractures. Radiographics 16:35–48
Kaup M, Wichmann J, Scholtz J, Beeres M, Kromen W, Albrecht MH, Lehnert T, Boettcher M, Vogl TJ, Bauer R (2016) Dual-energy CT-based display of bone marrow edema in osteoporotic vertebral compression fractures: impact on diagnostic accuracy of radiologists with varying levels of experience in correlation to mr imaging. Radiology 29:150472
Wagner D, Ossendorf C, Gruszka D, Hofmann A, Rommens PM (2015) Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg 41:349–362
Hackenbroch C, Riesner HJ, Lang P, Stuby F, Beer M, Friemert B, Palm HG, Becken AG III (2017) Die dual-energy-computertomographie in der muskuloskeletalen radiologie mit fokus auf Insuffizienzfrakturen des beckens. Z Orthop Unfall 155:708–715
Thiryayi WA, Thiryayi SA, Freemont AJ, Klestil T, Kreczy A (2008) Histopathological perspective on bone marrow oedema, reactive bone change and haemorrhage. Eur J Radiol 67:62–67
Rangger C, Kathrein A, Freund MC, Klestil T, Kreczy A (1998) Bone bruise of the knee: histology and cryosections in 5 cases. Acta Orthop Scand 69:291–294
Tins BJ, Garton M, Cassar-Pullicino VN, Tyrrell PN, Lalam R, Singh J (2015) Stress fracture of the pelvis and lower limbs including atypical femoral fractures-a review. Insights Imaging 6:97–110
Ishibashi Y, Okamura Y, Otsuka H, Nishizawa K, Sasaki T, Toh S (2002) Comparison of scintigraphy and magnetic resonance imaging for stress injuries of bone. Clin J Sport Med 12:79–84
Spiegl U, Schnake K, Osterhoff G, Scheyerer M, Ullrich B, Bula P, Siekmann H (2018) Radiologische diagnostik von stress- und insuffizienzfrakturen des sakrums. Orthopädie und Unfallchirurgie. https://doi.org/10.1055/a-0640-8933
Schmitz P, Baumann F, Grechenig S, Gaensslen A, Nerlich M, Müller M (2015) The cement-augmented transiliacal internal fixator (caTIFI): an innovative surgical technique for stabilization of fragility fractures of the pelvis. Injury 46:114–120
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Palm, HG., Lang, P., Hackenbroch, C. et al. Dual-energy CT as an innovative method for diagnosing fragility fractures of the pelvic ring: a retrospective comparison with MRI as the gold standard. Arch Orthop Trauma Surg 140, 473–480 (2020). https://doi.org/10.1007/s00402-019-03283-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03283-8