Abstract
Objective
The aim of this observational study was to investigate the postoperative alignment change with Oxford unicompartmental knee arthroplasties (UKA), and clarify whether femoro-tibial facet angle (FTFA) is useful for evaluating alignment correctability with UKA.
Methods
This study evaluated 79 knees consecutive minimally invasive Oxford phase 3 UKAs performed between 2013 and 2014. Full-length weight-bearing radiographs of the lower limbs were obtained pre- and postoperatively to assess varus angle. Preoperative valgus stress radiography in the supine position was also performed. FTFA was measured on weight-bearing anteroposterior radiography and valgus stress radiography.
Results
The preoperative varus angle of 4.6° ± 3.1° reduced to 1.7° ± 2.6° postoperatively. Preoperative varus angle and postoperative varus angle change strongly correlated with the FTFA value and its change on the valgus stress radiographs, respectively (p < 0.01). Based on preoperative FTFA under valgus stress radiography, intra-articular varus corrected group (37 knees) with preoperative varus angle 2.9° ± 2.4° was corrected to − 0.3° ± 2.0° after UKA. However, intra-articular varus uncorrected group (42 knees) with preoperative varus angle 6.0° ± 3.0° was only corrected to 3.5° ± 1.7°. Thirteen knees (16.5%) were overcorrected to valgus after UKA, with a mean FTFA of − 1.2° ± 0.4° under valgus stress force, which related with a postoperative valgus angle 0.8° ± 1.2°.
Conclusion
FTFA change under valgus stress force was useful for evaluating the correctability of UKA. It could reflect intra-articular varus deformity. Intra-articular varus deformity not corrected under valgus stress would result in varus after UKA. However, intra-articular deformity which could be overcorrected under valgus stress would have a tendency to valgus after Oxford UKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the aging of the population in the world, the incidence of knee osteoarthritis is increasing. Unicompartmental knee arthroplasty (UKA) is a minimal invasive option for anteromedial osteoarthritis with many advantages, such as smaller incision, less soft tissue injury, minimal bone resection, preservation of normal knee kinematics, and rapid recovery [1,2,3,4].
As postoperative lower extremity alignment is crucial to the outcome of knee arthroplasty, the varus deformity correction is an important consideration before UKA. Valgus overcorrection or varus undercorrection may result in a poor result [5,6,7]. Overcorrection could cause contralateral compartmental overload and failure in arthritis progression [7,8,9]. However, undercorrection could increase the load to the medial compartment, which may accelerate polyethylene wear [9, 10].
However, to our knowledge, few studies have been reported of useful references for surgeon to predict alignment correctability with minimally invasive Oxford UKA. Tashiro et al. found coronal alignment could be predicted with full-length valgus stress radiography [11]. However, the evaluation parameter was weight-bearing ratio which was not an immediate factor for intra-articular deformity evaluation. Besides, it was about the fixed-bearing system which was designed quite different with the mobile-bearing system. The mobile Oxford UKA was designed to restore the natural knee with no attempt to assess the lower limb alignment intraoperatively, and no soft tissue release was performed. Therefore, a preoperative reference able to predict postoperative alignment may be useful. Femoro-tibial facet angle (FTFA) is the angle between femoral facet and tibial facet, which could reflect the intra-articular deformity. Therefore, the aim of this observational study was to investigate the postoperative alignment change with intra-articular deformity correction using minimally invasive Oxford phase 3 mobile-bearing UKA, and clarify whether the FTFA change under valgus stress force radiography is useful for evaluating alignment correctability with UKA.
The hypothesis of this study was that FTFA on preoperative anteroposterior (AP) radiographs under valgus stress would be correlated well with the postoperative alignment and be useful for predicting the alignment correctability with minimally invasive mobile-bearing UKA.
Patients and methods
Approval for the present study from the institutional review board was obtained. From September 2013 to December 2014, 79 knees consecutive knees of 68 patients were included. At baseline, the mean age was 69.0 ± 8.8 years, with a mean body mass index (BMI) of 24.6 ± 3.6 kg/m2. A total of 38 UKAs were performed on the right knee and 41 on the left knee; 24 knees were male (30.4%) and 55 were female (69.6%). The indications for UKA were severe knee pain of medial compartment and considerable difficulty in walking and performing daily activities. Radiograph can demonstrate loss of articular cartilage medially by showing that the medial joint width became narrow. The other indications were an intact anterior cruciate ligament (ACL), varus deformity < 15°, flexion contracture < 15°, intact lateral compartment [12]. The preoperative diagnosis was osteoarthritis in all patients. Informed consent was obtained from all individual participants included in the study.
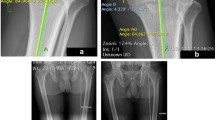
Weight-bearing, hip-to-ankle AP radiographs were taken at our institution both preoperatively and postoperatively. Care was taken to ensure that each patient stood with his/her patellae facing forward, to minimize rotational variation among the radiographs. Valgus stress radiographs were obtained without anesthesia in the supine position. The junior author manually applied a firm valgus force through the affected knee, paying attention to neutral rotation and keeping the tibia plateau parallel to the X-ray beam. On full-length weight-bearing radiographs, the hip–knee–ankle angle (HKAA) was defined as the angle between the femoral mechanical axis (center of hip to center of knee) and the tibial mechanical axis (center of knee to center of ankle) [13, 14]. Varus was defined as HKAA < 180°. The varus angle was defined HKAA subtracted from 180°. The femoro-tibial facet angle (FTFA) was defined as the angle between the best-fit line along the surface of the tibial plateau and the line connecting the most distal points of the medial and lateral femur condyles. The FTFA was measured on weight-bearing AP radiograph and valgus stress radiograph. According to the FTFA on valgus stress radiographs, the sample was divided into two groups. Group A, intra-articular varus corrected group, which valgus force could correct FTFA to 0° or more, was defined as correctable. Group B, intra-articular varus uncorrected group under valgus stress, which valgus force could not correct FTFA to 0°, was considered undercorrected. The measurements were performed on a picture archiving and communication system (PACS) using software packages in the hospital. Each measurement was performed twice by two independent observers (Fig. 1a–d).
a A case of a 73-year-old woman with varus knee OA was treated with UKA. Femoro-tibial facet angle on weight-bearing radiographs was 7.0°. The femoro-tibial facet angle (FTFA) was defined as the angle between the best-fit line along the surface of the tibial plateau and the line connecting the most distal points of the medial and lateral femur condyles. b Femoro-tibial facet angle (FTFA) under valgus stress force radiography was corrected to 3.7°. c Preoperative hip–knee–ankle angle (HKAA) on full-length weight-bearing radiograph was 172.5°, which meant that varus angle was 7.5°. The hip–knee–ankle angle (HKAA) was defined as the angle between the femoral mechanical axis (center of hip to center of knee) and the tibial mechanical axis (center of knee to center of ankle). d Postoperative hip–knee–ankle angle (HKAA) on full-length weight-bearing radiograph was 176.5°, which meant that varus angle was 3.5°
All UKA procedures were performed by the senior author using the same minimally invasive surgical technique with the mobile Oxford medial UKA (Oxford unicompartmental knee, Zimmer Biomet, Bridgend, UK). The knee joint was exposed through a small skin incision with quadriceps sparing and no patellar eversion. Medial release for ligament balancing or realignment was not performed. However, all medial osteophytes were completely removed with the osteotome. The ligament balance was determined according to 1 mm gap after the polyethylene bearing insert. Patients were followed up at months 3, 6, and 12, and yearly thereafter. The final assessment was recorded for analysis.
All data were analyzed using SPSS for windows 17.0 (SPSS, Chicago, IL, USA). The data was reported as the mean ± standard deviation. The χ2 test and t test were used to determine statistically significant differences between the groups. The relationships between varus angle and FTFA were evaluated using Pearson’s correlation coefficient to assess whether each parameter could be used to predict the alignment correctability. A p value < 0.05 was considered statistically significant [15].
Results
The mean follow-up was 18.3 ± 4.5 months with no lost. In all patients, passive full flexion of the knee and painless active full flexion was possible within 7 postoperative days and 3 postoperative months, respectively. The mean preoperative range of motion (ROM) was 120.8° ± 9.7°, which was improved to a mean of 124.8° ± 6.4° at the final follow-up, although this difference was not statistically significant (p = 0.349). The mean hospital for special surgery (HSS) knee score increased from 58.7 ± 8.4 to 92.2 ± 4.9 at the time of final follow-up (p = 0.000). The mean preoperative FTFA on weight-bearing radiographs was 3.2° ± 1.8°, which reduced to 0.3° ± 1.0° on the preoperative valgus stress radiographs with valgus stress force (p < 0.01). The mean mechanical preoperative varus angle of 4.6° ± 3.1° reduced to 1.7° ± 2.6° after UKA (p = 0.000, < 0.01).
The varus angle on full-length weight-bearing radiography was 4.6° ± 3.1°, which was strongly correlated with the FTFA value on weight-bearing radiography (r = 0.658, p < 0.01). The formula was shown as following: Y (°) = 0.993 (°) + 1.126X (°) (Y: varus angle value; X: FTFA value). Correspondently, postoperative varus angle change showed a strong positive correlation with the preoperative FTFA change on valgus stress radiography (r = 0.603, p < 0.01). Y (°) = 0.223 (°) + 0.913X (°) (Y: varus angle change value; X: FTFA change value) (Figs. 2, 3).
According to preoperative FTFA under valgus stress radiography, the sample was divided into two groups. Group A, intra-articular varus corrected group under valgus stress, 37 knees, preoperative varus angle of 2.9° ± 2.4° reduced to − 0.3° ± 2.0° postoperatively. Group B, intra-articular varus uncorrected group under valgus stress, 42 knees, preoperative varus angle of 6.0° ± 3.0° was corrected to 3.5° ± 1.7° postoperatively. The two groups were comparable in terms of age, gender distribution, and BMI. There were no differences in the mean postoperative HSS score and ROM between the groups. Though the difference in amount of correction achieved after surgery in two groups was not statistically significant (2.5° ± 2.9°, 3.2° ± 1.7°, p > 0.05), the pre-and post-operative varus angle between the two groups with and without intra-articular varus correction under valgus stress were significantly different. In Group B, the varus deformity was more severe than that of Group A (preoperative varus angle: Group A: 2.9° ± 2.4°, Group B: 6.0° ± 3.0°, p < 0.001). Under the valgus stress force, intra-articular deformity could not be corrected in Group B. Therefore, more postoperative varus deformity was remained in Group B after UKA (postoperative varus angle: Group A: − 0.3° ± 2.0°, Group B: 3.5° ± 1.7°, p < 0.001) (Table 1).
After UKA, there were 13 knees (16.5%) whose alignment was overcorrected to postoperative valgus, with a mean age of 71.0 ± 8.7 years. Before UKA, the intra-articular varus deformity was also overcorrected to valgus under valgus stress radiograph with the mean FTFA − 1.2° ± 0.4° (− 2.0 to − 1.0°), which was related to a mean postoperative valgus angle 0.8° ± 1.2° (1.0° to − 3.0°) after UKA (Table 2).
Discussion
The most important finding of the present study was that the postoperative varus angle change was significantly strong correlated with the preoperative FTFA change on the valgus stress radiographs. FTFA could reflect intra-articular varus deformity correctability. FTFA would increase as the varus deformity worsen, especially when bone on bone in medial compartment. FTFA change on valgus stress radiographs can be used to evaluate the correctability of varus deformity preoperatively and predict the postoperative alignment correctability after minimally invasive Oxford medial UKA.
The varus deformity is the frontal malalignment in osteoarthritis, which is crucial to the result of knee arthroplasty. The varus deformity included the intra-articular and extra-articular deformity [16, 17]. HKAA is usually used to assess the total malalignment deformity, which is determined by the mechanical axis of both the femur and the tibia. FTFA is the angle between femoral facet and tibial facet, which could reflect the deformity of intra-articular knee. Furthermore, it is not influenced by the extra articular deformity. The intra-articular varus deformity may due to the medial wear with or without medial ligament crispation, which is generally reducible in UKA. The indication of UKA is anteromedial osteoarthritis, whose varus deformity is from cartilage erosion in medial compartment. The angle of varus depends on the amount of cartilage loss in medial compartment. Each millimeter cartilage wear increase by 1° varus. To expose bone on both surfaces, the total thickness of cartilage wear is about 5 mm, causing about 5° varus [18,19,20,21]. The mean preoperative varus angle on weight-bearing radiographs in the case series was 4.6 ± 3.1°, which reflected the varus might result from cartilage wear. This formula Y (°) = 0.993 (°) + 1.126X (°) (Y: varus angle value; X: FTFA value) can be used to reflect the relationship between varus angle and FTFA. As the varus angle on full-length weight-bearing radiography was strong correlated with the FTFA value on weight-bearing radiography, the FTFA measurement on weight-bearing radiography was useful for evaluation of intra-articular varus deformity.
Oxford unicompartmental knee has a mobile-bearing with full congruency, minimizing polyethylene wear and restoring the natural knee motion [22]. The principle of the procedure was to keep knee stability by ligament tension. Soft tissue tension must be adequate to prevent the joint from subluxation or dislocation. Over high tension may cause excessive wear of polyethylene or even limit movement. On the other hand, lessening tension may cause instability and bearing dislocation. If we keep the natural tension with no soft tissue release, the size of bearing which inserted into the knee is related to bone cut and the correctability of articular deformity. More bone cut, thicker bearing size. Smaller bone cut, thinner bearing size. If we use larger size bearing, overcorrection tends to incur. On the contrary, if we use smaller bearing, undercorrection and dislocation of bearing would incur. Therefore, the alignment correctability of Oxford UKA mostly depends on the correctability of intra-articular deformity which is related to the cartilage wear correction and restored ligament tension. The valgus stress radiography can reflect the correctability of intra-articular varus deformity from cartilage wear when the medial soft tissue is not released. It follows that FTFA change on valgus stress radiographs can be used to evaluate the correctability of varus deformity preoperatively and predict the postoperative alignment after medial UKA.
The other finding of the study was that intra-articular deformity which could be overcorrected under valgus stress radiographs would tend to valgus after UKA. However, the preoperative varus not corrected under valgus stress radiographs would result in excessive varus after UKA. This formula Y (°) = 0.223 (°) + 0.913X (°) also can be used to reflect the peculiarity in the alignment correctability of Oxford UKA. Though the alignment could be to some extent corrected, limbs with more severe preoperative varus deformity tended to remain in excessive varus. Mullaji investigated 122 consecutive minimally invasive Oxford phase 3 medial unicompartmental knee arthroplasties in 109 patients for postoperative alignment. In 75% of the knees, the HKAA was restored to within an acceptable alignment of 177° ± 3°, 14% of the limbs were in excessive varus (< 174°), and 11% were in valgus (> 180°) [23]. Although most of the limbs had acceptable alignment after UKA, some patients would have excessive varus or valgus. The reason might be that limbs with more severe preoperative varus deformity had a contracted ligament. It followed that FTFA under valgus stress radiographs cannot be corrected to 0°, in other words, intra-articular varus deformity was not correctable before operation. However, no ligament was not allowed to release in UKA procedure and the contracted ligament was not corrected to acceptable length. Consequently, it remained in excessive varus after mobile-bearing UKA. In contrast, limbs with FTFA overcorrected had a tendency to result in valgus after UKA. The reason might be that limbs overcorrected under valgus force do not have a contracted ligament and serious cartilage wear. It follows that intra-articular varus was less and FTFA could easily be overcorrected to 0°or more under valgus stress. Besides, some patients may have a small physiological habitual valgus before developing medial compartmental OA due to medial wear. According to UKA procedure, soft tissue tension must be adequate to prevent the joint from subluxation or dislocation. Thus, surgeon usually preferred a thicker bearing to keep the joint gap 1 mm. As a result, the postoperative alignment tended to be valgus after mobile-bearing insertion.
With respect to patient selection in practice, intra-articular varus deformity correctable is proper indication for medial UKA, especially the mild-to-moderate varus corrected group under valgus stress. As overcorrection could cause contralateral compartmental overload and failure in arthritis progression, it might be better to select patient without FTFA overcorrected under valgus stress radiographs. Otherwise, limbs with FTFA overcorrected under valgus stress have a tendency to valgus after UKA. Similarly, limbs with more severe preoperative varus deformity tend to remain in excessive varus. The serious intra-articular varus deformity that could not be corrected to acceptable angle under valgus stress is not indicated for UKA, especially those varus not just from cartilage wear. Therefore, varus deformity is not allowed to be larger than 15° for UKA indication criteria. Total knee arthroplasty should be the best choice for serious varus deformity, which could correct deformity more amount because of bone cut and ligament release [24, 25].
Nevertheless, there were still a few potential weaknesses in the study. First, the evaluation of the ligamentous balance was not quantified. The gap was 1 mm, which was a subjective indicator. However, all procedures were performed by the senior author, and the surgical criteria of soft tissue and bone preservation were uniform throughout the study. Second, the valgus stress force was not applied using a measurable tensor device. Therefore, the distraction force may not always have been the same as the one applied during stress radiography. However, the same valgus force may not be appropriate for different patient to correct the varus deformity in practice. Third, as the aim of this study was to investigate usefulness of FTFA under valgus stress for evaluating correctability of varus deformity, many other factors such as excising osteophytes were not analyzed in the study, which might influence the correctability [26]. Further study is still needed to elaborate the result.
In conclusion, femoro-tibial facet angle (FTFA) can reflect intra-articular deformity from varus knee. FTFA change under valgus stress force radiography is useful for evaluating the correctability of intra-articular varus deformity. Intra-articular deformity varus not corrected under valgus stress radiographs will result in varus after UKA. However, intra-articular deformity which can be overcorrected under valgus stress radiographs will tend to valgus after Oxford UKA.
References
Berger RA, Della VC (2010) Unicompartmental knee arthroplasty: indications, techniques, and results. Instr Course Lect 59:47–56
Lisowski LA, van den Bekerom MP, Pilot P, van Dijk CN, Lisowski AE (2011) Oxford Phase 3 unicompartmental knee arthroplasty: medium-term results of a minimally invasive surgical procedure. Knee Surg Sports Traumatol Arthrosc 19:277–284
Price AJ, Dodd CA, Svard UG, Murray DW (2005) Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br 87:1488–1492
Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83:191–194
Aleto TJ, Berend ME, Ritter MA, Faris PM, Meneghini RM (2008) Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty 23:159–163
Zhang Q, Zhang Q, Guo W, Liu Z, Cheng L, Yue D, Zhang N (2014) The learning curve for minimally invasive Oxford phase 3 unicompartmental knee arthroplasty: cumulative summation test for learning curve (LC-CUSUM). J Orthop Surg Res 9:81
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res (423):161–165
Kim KT, Lee S, Kim TW, Lee JS, Boo KH (2012) The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res 24:85–90
Kim SJ, Bae JH, Lim HC (2012) Factors affecting the postoperative limb alignment and clinical outcome after Oxford unicompartmental knee arthroplasty. J Arthroplasty 27:1210–1215
Bruni D, Iacono F, Russo A, Zaffagnini S, Marcheggiani MG, Bignozzi S, Bragonzoni L et al (2010) Minimally invasive unicompartmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients. Knee Surg Sports Traumatol Arthrosc 18:710–717
Tashiro Y, Matsuda S, Okazaki K, Mizu-Uchi H, Kuwashima U, Iwamoto Y (2014) The coronal alignment after medial unicompartmental knee arthroplasty can be predicted: usefulness of full-length valgus stress radiography for evaluating correctability. Knee Surg Sports Traumatol Arthrosc 22:3142–3149
Murray DW (2005) Mobile bearing unicompartmental knee replacement. Orthopedics 28:985–987
Marx RG, Grimm P, Lillemoe KA, Robertson CM, Ayeni OR, Lyman S, Bogner EA et al (2011) Reliability of lower extremity alignment measurement using radiographs and PACS. Knee Surg Sports Traumatol Arthrosc 19:1693–1698
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Nayak BK, Hazra A (2011) How to choose the right statistical test? Indian J Ophthalmol 59:85–86
Thienpont E, Parvizi J (2016) A New Classification for the Varus Knee. J Arthroplasty 31:2156–2160
Maderbacher G, Baier C, Springorum HR, Zeman F, Grifka J, Keshmiri A (2016) Lower limb anatomy and alignment affect natural tibiofemoral knee kinematics: a cadaveric investigation. J Arthroplasty 31:2038–2042
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br 73:582–586
Ahlback S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) Suppl 277:7–72
Mullaji AB, Marawar SV, Luthra M (2008) Tibial articular cartilage wear in varus osteoarthritic knees: correlation with anterior cruciate ligament integrity and severity of deformity. J Arthroplasty 23:128–135
Moschella D, Blasi A, Leardini A, Ensini A, Catani F (2006) Wear patterns on tibial plateau from varus osteoarthritic knees. Clin Biomech (Bristol Avon) 21:152–158
Kendrick BJ, Simpson DJ, Kaptein BL, Valstar ER, Gill HS, Murray DW, Price AJ (2011) Polyethylene wear of mobile-bearing unicompartmental knee replacement at 20 years. J Bone Joint Surg Br 93:470–475
Mullaji AB, Shetty GM, Kanna R (2011) Postoperative limb alignment and its determinants after minimally invasive Oxford medial unicompartmental knee arthroplasty. J Arthroplasty 26:919–925
Wyss TF, Schuster AJ, Munger P, Pfluger D, Wehrli U (2006) Does total knee joint replacement with the soft tissue balancing surgical technique maintain the natural joint line? Arch Orthop Trauma Surg 126:480–486
Sim JA, Lee YS, Kwak JH, Yang SH, Kim KH, Lee BK (2013) Comparison of complete distal release of the medial collateral ligament and medial epicondylar osteotomy during ligament balancing in varus knee total knee arthroplasty. Clin Orthop Surg 5:287–291
Thienpont E, Schwab PE, Cornu O, Bellemans J, Victor J (2017) Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg 137(3):393–400
Funding
This study was funded by “the capital health research and development of special” (Grant number 2016-2-4062) and National Natural Science Foundation of China (grant number 81703896).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Zhang, Q., Yue, J., Wang, W. et al. FTFA change under valgus stress force radiography is useful for evaluating the correctability of intra-articular varus deformity in UKA. Arch Orthop Trauma Surg 138, 1003–1009 (2018). https://doi.org/10.1007/s00402-018-2945-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2945-6