Abstract
Introduction
Lipomas are associated with a variety of symptoms including neuropathies, local compression of the surrounding tissues, aesthetic complaints and may be graded as liposarcomas histologically. This study was performed to review our surgical management at the level of the hand.
Materials and methods
Between 2008 and 2013, 14 patients were referred to our department for suspected adipose tumour of the hand. Preoperative MRI was used to assess tumour and surrounding tissue to plan the surgical therapy. We reviewed the clinical history, MRI findings, surgical approach, and outcomes.
Results
Complaints leading to consultation were pain in 11 cases, compression neuropathy in 7 cases, aesthetic concern in 8 cases, and limited wrist range of motion in 2 cases. Magnetic resonance imaging was performed in 13 cases, confirming the diagnosis of adipose tumour in all but two cases. These two cases were diagnosed in one case as a ganglion and the other as an epithelioid sarcoma. An amputation of the fifth digit was performed regarding the latter case and the patient received additional radiotherapy. The mean follow-up period was 32 ± 20 months. There was no recurrence of lipoma or sarcoma.
Conclusion
MRI is useful for diagnosing and planning of the surgical intervention performed in the latter case adipose tumours. Rapidly evolving tumours with subfascial localization are absolute surgical indications. Incision biopsy is mandatory for entities of unknown dignity and for malignant tumours. Interdisciplinary tumour board meetings should discuss each patient before surgery is performed.
Level of evidence and study type
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lipomas arise from mesenchymal primordial fatty-tissue cells [1]. Their location in the hand is infrequent, where they represent 8 % of benign tumours [2, 3]. Their presence in the hand is associated with a variety of symptoms including neuropathies, local compression of surrounding tissues, pain and aesthetic complaints. Moreover, lipomas may present as liposarcomas [4].
Despite numerous cases reported in the literature [5–17], only a few studies have focused specifically on tumours concerning the hand and most of them are heterogeneous with differing preoperative management algorithms.
According to Halldorsdottir et al. [18] and our own experience, preoperative imaging and a curative approach are mandatory for adipose tumours of the hand due to the risk of malignant transformation.
This study evaluates the management of 14 patients with adipose tumours of the hand with special focus on MRI findings, risk of sarcomatous transformation and surgical management. We reviewed the histological data.
Materials and methods
Patients
This retrospective study was performed in accordance to the ethical guidelines of the University of Bordeaux. Criteria for inclusion were patients of all ages regardless of sex, with initial suspicion of adipose tumour of the hand. They were treated between January 2008 and December 2013. Fourteen patients, nine women and five men, met the study inclusion criteria. The mean age of patients was 56.5 (SD ±13.4 years; range 29–75 years) (Table 1).
Clinical examination
Symptoms were carefully reviewed. Careful observations were recorded with regard to pain, interference with hand function, compression neuropathy, trigger finger and aesthetic concerns. Lipomas presented as a slowly growing, soft, mobile and non-tender mass. Subcutaneous localization of the tumour was characterised by “doughy” resistance during palpation. Application of ice packs on the tumour to chill and harden the fat tissue was also used in diagnosis.
Preoperative MRI assessment
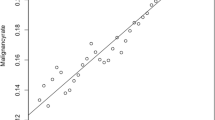
Preoperative 3.0-T MRI was performed to assess the suspected tumour and to plan surgery if (a) the tumour size was greater than 5 cm in diameter at palpation and if the latter (b) was situated subfascially, or (c) if its diameter increased rapidly over time. The patient was scanned supine, arms adducted and the dorsum of the hand parallel to the coronal plane of the magnetic field. To achieve high resolution, a small field of view (8–12 cm), with a matrix of 256 × 512 and slice thickness of 1.5–3 mm was used. MRI examination included coronal and sagittal T1- and T2-weighted sequences with axial short tau inversion recovery (STIR) and T1-weighed images. Intravenous gadolinium was applied to facilitate diagnosis for difficult entities.
Measured parameters
Clinical history, MRI findings, surgical approach, and outcomes were assessed diligently. Postoperative range of motion, grip strength, and pinch strength of the operated hand were compared to preoperative values. Grip strength and pinch strength were measured using the Jamar dynamometer.
All variables were analysed descriptively by tabulation of the measures of the empirical distributions. Possible differences between groups were tested using t test in case of continuous data. Significance level was set at p < 0.05.
Results
Clinical findings
Complaints leading to consultation were pain in 11 cases, compression neuropathy in 7 cases, aesthetic concerns in 8 cases, and limited wrist range of motion in 2 cases (Table 1). The compression neuropathy was localised at the level of the Guyon loge in 2 cases, at the level of the carpal tunnel in 1 case, and at the level of the interdigital or digital nerves in 4 cases.
MRI Assessment and Surgical Approach
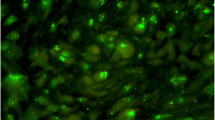
MRI was performed in all but one case. It confirmed the diagnosis of adipose tumours in all but two cases (Figs. 1, 2). In these two cases, the final diagnosis was a ganglion on the one hand and on the other hand an epithelioid sarcoma. The surgical approaches are presented in Table 1. In case of malignancy, a marginal excision was performed first and after reviewing the histological findings at the tumour board meeting, amputation of the fifth digit was done afterwards (Fig. 2). The patient received additional radiotherapy (80 Gy).
Histological findings and outcomes
Histological findings were lipoma in 7 cases, myxoid lipoma in 2 cases, and single angiolipoma, fusiform lipoma, lipofibromatous hamartoma, ganglion and epithelioid sarcoma. The mean follow-up period was 32.3 ± 19.6 months. There was no recurrence of lipoma and the patient with sarcoma is now considered in remission. Complete finger extension and grasp were reached in all cases. The postoperative wrist extension/flexion and wrist pro/supination reached 97.4 ± 4.8 % (p > 0.05), and 97.3 ± 3.5 % (p > 0.05) of the preoperative values, respectively. The postoperative grip strength and pinch strength reached 89.4 ± 9.4 % (p < 0.01), and 87.7 ± 13.5 % (p < 0.01) of the preoperative values, respectively.
Discussion
Lipomas were considered as rare entities of the upper extremity. Nowadays, these tumours are regarded common among soft tissue tumours of the hand representing 1–3.8 % of the benign tumours of the hand [2, 3]. In our own series, they represent 8.1 % of all patients operated for tumours of the hand between 2008 and 2013. Most often, adipose tumours come to clinical attention when they are of aesthetic concern for the patient or become large enough to create mechanical impairment [19]. In 1972, Leffert reported his experience of 141 lipomas of the upper extremity [20]. 109 tumours were asymptomatic and excised solely for aesthetic reasons. Of the 32 symptomatic lesions, 26 caused pain or tenderness, and 6 produced paraesthesias or sensory deficit secondary to nerve compression. Other presentations have been documented extensively in the literature: restricted range of motion and deformation of the wrist or digits [21, 22], decreased grip strength [23], muscle paralysis [24], polyarthritis [25], trigger finger [26, 27], dysaesthesias [28], muscle atrophy [29, 30], and nail plate dystrophy and thinning [31]. Another reason to perform excision is the subsequent risk of malignant transformation [4].
We regard an MRI assessment crucial in case of suspected adipose tumour. MRI assists in confirming diagnosis and specifying a surgical approach which avoids potential iatrogenic injuries [32]. Surgical excision is the gold standard for adipose tumour because of potential malignant appearance. It is strongly recommended (a) if the tumour size is greater than 5 cm in diameter (b) if the tumour is rapidly growing and (c) if the tumour is located beneath the muscle fascia. The criterion of the absolute tumour size is of minor relevance concerning the hand. The former should be heeded for more proximal localizations. The procedure can often be performed under local or plexus anaesthesia. Other approaches have been reported in the literature including liposuction or the use of injection of compounds that trigger lipolysis, such as steroids or phosphatidylcholine [33]. However, these techniques may fail to remove the entire tumour, which can promote recurrence. Moreover, the latter should be discarded since tissue samples for histological examination cannot be harvested. Indeed, the diagnosis of sarcoma cannot be ruled out before histological evaluation was done.
Despite a relative long follow-up period, methodological limitations remain. First, this study was undertaken at one department only. Second, the number of patients examined is quite small compared to the studies of Leffert [19]. However, this series was specifically focused on the hand and the retrospective analysis was sufficient, since patients’ data had been accurately archived using the clinic’s electronic database.
Conclusion
MRI is useful for diagnosing and planning of the surgical intervention regarding adipose tumours. Rapidly evolving tumours with subfascial localization are absolute surgical indications. Incision biopsy is mandatory for entities of unknown dignity and for malignant tumours. Interdisciplinary tumour board meetings are supposed to discuss each patient before surgery is performed.
References
Ceballos JI, Wylock P (2005) Hand palm and finger lipomas: four case reports and review of the literature. Eur J Plast Surg 28:243–246
Bogumill GP (1975) Tumours of the hand. Clin Orthop 108:214–222
Butler ED (1960) Tumours of the hand, a ten years survey and report of 437 cases. Am J Surg 100:293–302
Deshmukh SD, Gulati HK, Yadav P, Naik P (2013) Palmar well differentiated spindle cell liposarcoma: presentation of a rare tumor at a rare site. Hand Surg 18:115–120
Chatterton BD, Moores TS, Datta P, Smith KD (2013) An exceptionally large giant lipoma of the hand. BMJ Case Rep Epub Jul 8
Ramirez-Montaño L, Lopez RP, Ortiz NS (2013) Giant lipoma of the third finger of the hand. Springerplus 16:164
Bennani A, Saliou SS, Zizah S, Hamdi O, Almoubaker S, Lahrach K, Marzouki A, Boutayeb F (2013) An unusual location of juxtaosseous ossified lipoma. A case report. Chir Main 32:113–116
Kitagawa Y, Tamai K, Kim Y, Hayashi M, Makino A, Takai S (2012) Lipoma of the finger with bone erosion. J Nippon Med Sch 79:307–311
Jalan D, Garg B, Marimuthu K, Kotwal P (2011) Giant lipoma: an unusual cause of carpal tunnel syndrome. Pan Afr Med J 9:29
Pagonis T, Givissis P, Christodoulou A (2011) Complications arising from a misdiagnosed giant lipoma of the hand and palm: a case report. J Med Case Rep 15:552
Gupta A, Singal R, Mittal A, Goyal M (2011) Report of two cases of subcutaneous lipoma over the finger and review of literature: case series: benign tumour. Musculoskelet Surg 95:247–249
Abkari I, Abidi AE, Latifi M (2011) Giant lipoma of the third finger: a case report. Chir Main 30:152–154
Amar MF, Benjelloun H, Ammoumri O, Marzouki A, Mernissi FZ, Boutayeb F (2012) Anatomical snuffbox lipoma causing nervous compression. A case report. Ann Chir Plast Esthet 57:409–411
Chronopoulos E, Nikolaos P, Karanikas C, Kalliakmanis A, Plessas S, Neofytou I, Laspas F, Tzovara I, Chalazonitis A (2010) Patient presenting with lipoma of the index finger: a case report. Cases J 3:20
Fnini S, Hassoune J, Garche A, Rahmi M, Largab A (2010) Giant lipoma of the hand: case report and literature review. Chir Main 29:44–47
Grivas TB, Psarakis SA, Kaspiris A, Liapi G (2009) Giant lipoma of the thenar–case study and contemporary approach to its aetiopathogenicity. Hand (N Y) 4:173–176
Stuffer M (1995) Lipoma of the index digit—a very rare location. Arch Orthop Trauma Surg 114:239–240
Halldorsdottir A, Ekelund L (1982) CT diagnosis of lipomatous tumors of the soft tissues. Arch Orthop Trauma Surg 100:211–216
Dailiana ZH, Bougioukli S, Varitimidis S, Kontogeorgakos V, Togia E, Vlychou M, Malizos KN (2014) Tumors and tumor-like lesions mimicking carpal tunnel syndrome. Arch Orthop Trauma Surg 134:139–144
Leffert RD (1972) Lipomas of the upper extremity. J Bone Joint Surg Am 54:1262–1266
Oster LH, Blair WF, Steyers CM (1989) Large lipomas in the deep palmar space. J Hand Surg Am 14:700–704
Lee YH, Jung JM, Baek GH, Chung MS (2004) Intramuscular lipoma in thenar or hypothenar muscles. Hand Surg 9:49–54
Hoehn JG, Farber HF (1983) Massive lipoma of the palm. Ann Plast Surg 11:431–433
McFarland GB Jr, Hoffer MM (1971) Paralysis of the intrinsic muscles of the hand secondary to lipoma in Guyon’s tunnel. J Bone Joint Surg Am 53:375–376
Fernandez-Sueiro JL, Pinto JA, Blanco FJ et al (2006) Multiple parosteal lipoma associated to polyarthritis. Joint Bone Spine 73:202–204
Sonoda H, Takasita M, Taira H, Higashi T, Tsumura H (2002) Carpal tunnel syndrome and trigger wrist caused by a lipoma arising from flexor tenosynovium: a case report. J Hand Surg Am 27:1056–1058
Pampliega T, Arenas AJ (1997) An unusual trigger finger. Acta Orthop Belg 63:132–133
Bardazzi F, Savoia F, Fanti PA (2003) Subungual lipoma. Br J Dermatol 149:418
Posch JL (1956) Tumors of the hand. J Bone Joint Surg Am 38:517–539
Ingari JV, Faillace JJ (2004) Benign tumors of fibrous tissue and adipose tissue in the hand. Hand Clin 20:243–248
Flores LP, Carneiro JZ (2007) Peripheral nerve compression secondary to adjacent lipomas. Surg Neurol 67:258–262
Puhaindran ME, Pratt J, Manoso MW, Healey JH, Mintz DN, Athanasian EA (2010) Predictive value of magnetic resonance imaging in determining presence of residual disease after marginal excision of unsuspected soft tissue sarcomas of the hand. J Hand Surg Am 35:1479–1484
Pindur L, Sand M, Altmeyer P, Bechara FG (2011) Recurrent growth of lipomas after previous treatment with phosphatidylcholine and deoxycholate. J Cosmet Laser Ther 13:95–96
Acknowledgment
Thanks to Dr. Emma Hayton for review of the english manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leclère, F.M., Casoli, V., Pelissier, P. et al. Suspected adipose tumours of the hand and the potential risk for malignant transformation to sarcoma: a series of 14 patients. Arch Orthop Trauma Surg 135, 731–736 (2015). https://doi.org/10.1007/s00402-015-2170-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2170-5