Abstract
Malignant transformation of fibrous dysplasia is very rare. The frequency is increased in polyostotic forms, in McCune–Albright and Mazabraud’s syndromes and previously irradiated cases. Pain, which is rapidly becoming worse over a short period unrelated to trauma is the most alarming symptom. Early radiological features of sarcomatous transformation are moth-eaten or cystic areas of osteolysis, cortical destruction and gradual formation of a soft tissue mass. The prognosis is unfavorable as most of the cases are in an advanced stage in the time of diagnosis. We present an unusual case of unsuspected secondary osteosarcoma arising in a previously unirradiated, monostotic fibrous dysplasia. A 46-year-old woman was admitted with hip pain, which worsened after a minor trauma occurred 1 year ago. Plain graphies of left femur showed a well-delineated lesion with endosteal scalloping and areas having a ground-glass appearance. The MRI revealed minimal contrast enhancement but no heterogenous signal intensity, cortical destruction, periost reaction or accompanying soft tissue component was noted. The lesion was initially curetted. But being diagnosed as osteosarcoma histologically, classical osteosarcoma protocol pre and postoperative chemotherapy was applied. Resected femur showed areas of fibrous dysplasia admixed with osteosarcoma having fibroblastic, chondroblastic and osteoblastic areas that were focally invading the soft tissue. Tumor viability was estimated as 95%. The clinical course worsened rapidly after the operation. She did not respond to postoperative chemotherapy and lost with pulmonary metastases less than a years’ time after the operation. The case is presented to increase awareness on the possibility of malignant transformation in an otherwise unsuspected fibrous dysplasia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibrous dysplasia (FD) is a benign medullary fibro-osseous lesion, which may present in either monostotic or polyostotic forms [5]. The prognosis of patients with FD is very good but malignant transformation occurs, although rarely. The frequency of malignant change is increased in polyostotic forms, especially in patients with concomitant McCune–Albright [1] (endocrine abnormalities and skin pigmentation) and Mazabraud’s syndromes (polyostotic fibrous dysplasia and soft tissue myxomas) [10]. It is estimated to be 4% for McCune–Albright syndrome while it is just 0.5% for monostotic forms [14]. Osteosarcoma is the most common type of tumor, followed by fibrosarcoma and chondrosarcoma [12]. Patients are usually in the third or fourth decades of life. The most frequent anatomic sites are the craniofacial bones, the femur, and the tibia, which generally received radiation therapy before the sarcoma developed [12]. We present a case of secondary osteosarcoma of femur arising in a previously nonirradiated monostotic FD, which was clinically and radiologically unsuspected.
Case presentation
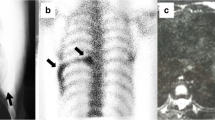
A 46-year-old woman was admitted with hip pain which was worsened after a minor trauma occurred 1 year ago. She had experienced a major trauma and fracture in her left femur 30 years ago and she had been suffering from mild hip pain since then. She laid a history of being diagnosed as having a “benign-natured disease” 15 years ago. She visited several outpatient clinics when she had pain and went on painkillers since then but refused surgical treatment. Her previous plain graphies and magnetic resonance images (MRI) were reviewed when she was referred to our hospital (Fig. 1). In the MRI performed 2 years prior to admission, collodiaphyseal angle was changed related to pathologic fracture of collum femoris, and a lesion could be identified located in metaphysio-diaphyseal location of left femur. It had a completely homogeneous morphology and displayed isointensity with body fluids. The lesion was consistant with “fibrous dysplasia” and remained unchanged in MRI performed in the following year. There was no cortical destruction, periost reaction, or accompanying soft tissue component. The lesion showed minimal contrast enhancement but no heterogenous signal intensity was noted. Plain X-ray graphies showed endosteal scalloping and well-delineated areas with a ground-glass appearance, which was also consistent with FD. There was a coxa-vara deformity in consistency with MRIs. The overall radiologic appearance, and stable nature of the lesion suggested an ordinary FD, complicated by a healed fracture. The lesion was monostotic and the case did not show cutaneous pigmentation, endocrine disturbances or soft tissue lesions as can be seen with McCune–Albright and Mazabraud’s syndromes. She had a 4-mm pulmonary opacity reminiscence of tuberculosis sequel in plain pulmonary graphy where the thorax computerized tomography revealed a second nodule having the same size and lesion characteristics. She was treated with curettage and bone cementing.
Imaging characteristics of the lesion. a Plain radiography of the femur shows a well-defined, lytic lesion with endosteal scalloping (arrow) and a pathologic fracture at collum femoris (arrowhead). The collo-diaphyseal angle is destroyed and a coxa-vara deformity can be observed. There is ground glass appearance in the central part of lesion (asterisk). No cortical destruction or periosteal reaction is present. b T1-W coronal plane MRI shows hypointense bone lesion compared to muscles at the proximal meta-diaphyseal region of left femur. c Contrast enhanced T1-W coronal plane MRI shows slightly enhancement of lesion. No heterogenously enhanced component is present. d STIR coronal plane MRI shows a well-defined, homogenously hyperintense lesion (equal to body fluids). No cortical destruction or soft tissue component is present
Curettage material (Fig. 2) displayed areas resembling aneurysmal bone cyst/telengiectatic osteosarcoma with hemorrhage and fibrin formation with numerous giant cells intermingled as well as foamy cells forming areas reminiscent of nonossifying fibroma. Solid areas showed widespread osteoid production. Osteoid producing cells were round or spindle shaped having either large vesicular nuclei or dense hyperchromatic nuclei. The tumor was noted to be densely cellular with a high mitotic rate including atypical figures. Thorough examination showed areas consistent with FD, showing an abnormal fibrous and immature osseous tissue. There were irregularly shaped, curved bone trabeculae, without a peripheral osteoblastic rimming. Thus the case was diagnosed as secondary osteosarcoma arising in preexisting FD. Therapeutic options were discussed in musculoskeletal tumor council and chemotherapy was given before tumor bed excision was performed. Following three courses of chemotherapy including Cisplatin and doxorubucin, rest tumor surgery and replacement of tumor resection prosthesis was done. In the total femur resection specimen (Fig. 3), tumor showed a mixed pattern of conventional osteosarcoma having fibroblastic, chondroblastic and osteoblastic areas that were focally invading the soft tissue and viability was estimated as 95%. In addition to area of FD in the vicinity of previously curetted segment, three more foci were observed in the distal metaphyseal region. They were measuring 5, 2, and 1.5 cm respectively in their largest diameters. And there were two minute “one trabecule-sized” microscopic foci. According to our strategy for conventional high-grade bone sarcomas three cycles of adjuvant chemotherapy was applied postoperatively. During her postoperative follow up she developed tumoral nodules around the femur prosthesis and several pulmonary nodules consistent with metastasis. She also suffered from local infection and acute femoral artery occlusion, which was cured by an inevitable left hip desarticulation. Additional satellite soft tissue nodules were observed in amputation material. She died of extensive pulmonary metastasis 11 months after the initial diagnosis (Fig. 4).
a Low power view of curetted specimen. Note the aneurysmal bone cyst/telengiectatic osteosarcoma-like areas filled with blood and fibrin (hematoxylen and eosin, ×4). b The walls of these cystic areas are rich in giant cells and they are lined by tumoral osteoid (hematoxylen and eosin, ×20). c Trichrome stains reveal the “lace-like” nature of lining osteoid (Masson’s trichrome stain, ×20). d Fibrous dysplasia areas and sarcomatous areas (asterisk) (hematoxylen and eosin, ×2)
a Postcurettage X-ray: Endosteal scalloping can be seen at the mid-diaphysis of femur. Implanted orthopedic material is also visible. b Femur resection performed after chemotherapy. Soft tissue extension of tumor is very prominent. Tumor also partially destroys the implanted chips. Note the other foci of fibrous dysplasia (arrows). The smallest focus is quite indistinguishable as admixed with fatty marrow (short arrow)
Resection specimen a Low power view of transition zone between fibrous dysplasia (left) and sarcomatous areas (right) (hematoxylen and eosin, ×2). b Soft tissue extention of osteosarcoma. Note the invasion through muscle bundles (hematoxylen and eosin, ×20). c Areas of fibrous dysplasia. Note the fibroblastic stroma and irregulary shaped, curved bone trabeculae, without a peripheral osteoblastic rimming (hematoxylen and eosin, ×10). d Other foci of fibrous dysplasia in distal metapyseal region marked with short arrow in Fig. 3 (hematoxylen and eosin, ×2)
Discussion
Experience on secondary osteosarcoma arising in FD is very limited since most cases have been published as single case reports due to the rarity of the entity. According to the largest series, malignant changes seem more likely to occur in polyostotic than in monostotic FD [7, 14]. Most of the cases that arose in monostotic disease have followed a previous radiation therapy [12, 16]. Unfortunately in most of these cases, sarcoma was in an advanced stage in time of diagnosis [7, 12] and did not respond to conventional chemotherapy as in classical osteosarcoma [6]. However there are experiences suggesting that secondary osteosarcomas may have a prognosis that approaches that of otherwise comparable primary osteosarcoma with combined therapy in case the local tumor control is achieved [3]. Thus it is important to recognize malignant transformation as early as possible, although it may not be easy as in our case. Hoshi et al. [8] reported four cases in which the FD was diagnosed only in one of them prior to sarcoma. The other three cases were diagnosed as sarcoma and FD at the same time. Suspecting from malignant transformation can be extremely difficult especially in cases with monostotic disease having either subtle symptoms or none. In the reported cases up to date, the specific symptoms of the malignant change were mainly pain, swelling and late appearance of a bony mass [8, 15]. But given the fact that the pain is a nonspecific finding and is the most common complaint followed by pathological fracture in FD [13], great care should be taken when evaluating this symptom. Pain which is rapidly becoming worse over a relatively short period without trauma should be considered alarming [8]. History of radiation therapy to the diseased area should also raise clinical suspicion. It must be kept in mind that sarcomatous changes in previously irradiated areas are late complications, thus the past history should be questioned in detail [2]. In cases of a typical osteosarcoma, radiographic features clearly illustrate the aggressive bone-forming nature of the lesion but secondary osteosarcomas, such as those arising from infarcts or fibrous dysplasia, may produce a confusing radiologic picture [11]. Presence of areas with ground-glass appearance is consistent with FD. Early radiological features of sarcomatous transformation in FD are moth-eaten or cystic areas of osteolysis, cortical destruction and gradual formation of a soft tissue mass [15]. Lesions generally have a poorly delineated margin within and/or near the area with a glassy appearance, prominent or slight periosteal reaction can also be found [8]. MRI shows an abundance of vascularity within the lesion and some lesions present slightly more contrast enhancement than FD areas [8]. Ring-like and spotty calcification in the tumor matrix generally indicates chondrosarcoma while the fibrosarcoma usually shows simple osteolytic destruction [15]. The presented case surprisingly had a completely homogeneous morphology, with a classical “ground glass appearence” and “Sheppard’s crook deformity” on plain graphy. It neither showed cortical destruction nor accompanying soft tissue component and remained unchanged until the first curettage. The tumor gradually showed an aggresive behavior after the currettage. It showed soft tissue extention in the resected specimen despite neoadjuvant chemotherapy cycles while “satellite” soft tissue nodules were observed in the subsequent desarticulation specimen. The case also developed concominant metastatic pulmonary nodules and unfortunately the prognosis did not approach to that of otherwise comparable primary osteosarcoma. One may speculate that the local control could not be achieved [3] since the tumor was curetted initially as malignancy was unsuspected. But very poor response to chemotherapy raises suspicions about tumor biology reserving the effect of the “contaminated” nature of the initial surgery.
The timing and etiology of malignant transformation are big questions, the answers of which are awaiting for further studies and case observations. Even in syndromic cases with McCune-Albright syndrome or Mazabraud’s syndrome, the specific molecular alterations that could account for an increased incidence of osseous sarcomas have not been completely elucidated [10]. Jhala et al. [9] presented a secondary osteosarcoma arising in a case of McCune–Albright syndrome and Mazabraud’s syndrome in which the osteosarcomatous portion exhibited trisomy of chromosomes 5 and 7 on karyotypic analysis, by comparative genomic hybridization and FISH. Complementary to this observation, Dal Cin et al. [4] reported a series of abnormalities including trisomy 2, rearrangement in chromosome 12 and a t(6;11)(q15;p15) translocation in cases of fibrous dysplasia and osteosarcoma, suggesting that FD is a neoplastic lesion rather than a dysplastic process. Thus it can be speculated that FD, is a neoplasm of very low malignant potential that can be transformed to a high-grade neoplasia someday because of an unknown stimulus. But probably a more acceptable approach would be supposing the cause of malignant transformation in most of the cases as a permanent mechanical trauma, destruction and regeneration of the bone.
Information concerning the management of these cases is also limited. Whether they respond to conventional osteosarcoma therapy is controversial [3, 6]. But distant metastasis and death was inevitable even in cases that received pre- and/or postoperative chemotherapy and widely resected subsequently [8]. Mortality rates are reported to be almost 54% [12] but these reports are not detailed in respect to adequacy of surgical treatment and chemotherapy protocols. Combination chemotherapies can alter prognosis but further accumulation of data is absolutely necessary. So far, no definitive statement regarding the efficacy of chemotherapy for this disease entity can be made. We followed our routine scheme for high-grade bone sarcomas but considering the poor response, postoperative chemotherapy was also added. Unfortunately the outcome was not promising for she was lost with pulmonary metastases less than a years’ time after the operation. And overall picture fit to the observations on secondary osteosarcomas that they did not respond to conventional chemotherapy as in classical osteosarcomas [6].
In conclusion, we presented an unusual case of secondary osteosarcoma arising in a long-standing, previously unirradiated monostotic fibrous dysplasia, which followed an aggressive and fatal course. According to the previously described, clinical and radiological findings, patients of sarcomatous transformation can be detected in earlier stages more promising for a disease free survival. In this respect, our case deserves attention since none of alarming findings were observed radiologically. Pain was the most serious symptom of the patient but it was dull in nature and was present for many years. And in contrast to the previous reports, the worsening period was long as almost a year and preceeded by a trauma. Nevertheless we conclude that all symptoms should be regarded as alarming for sarcomatous transformation thus we suggest prior histopathologic confirmation especially in cases with long standing disease.
References
Albright F, Butter AM, Smith P (1937) Syndrome characterized by posterities fibrosa disseminate, areas of pigmentation and endocrine dysfunction, with precocious puberty in females: report of five cases. N Engl J Med 216:727–746
Altay M, Bayrakci K, Yildiz Y, Sağlik Y (2004) The development of osteosarcoma following radiotherapy for fibrous dysplasia. Acta Orthop Traumatol Turc 38:353–356
Bielack SS, Kempf-Bielack B, Heise U, Schwenzer D, Winkler K (1999) Combined modality treatment for osteosarcoma occurring as a second malignant disease. Cooperative German–Austrian–Swiss Osteosarcoma Study Group. J Clin Oncol 17:1164
Dal Cin P, Sciot R, Brys P, De Wever I, Dorfman H, Fletcher CD, Jonsson K, Mandahl N, Mertens F, Mitelman F, Rosai J, Rydholm A, Samson I, Tallini G, Van den Berghe H, Vanni R, Willen H (2000) Recurrent chromosome aberrations in fibrous dysplasia of the bone: a report of the CHAMP study group. Chromosomes and morphology. Cancer Genet Cytogenet 122:30–32
Fletcher CDM, Unni KK, Mertens F (2002) Pathology and genetics of tumours of soft tissue and bone. IARC Press, Lyon
Healey JH, Buss D (1991) Radiation and pagetic osteogenic sarcomas. Clin Orthop 270:128–134
Horvai A, Unni KK (2006) Premalignant conditions of bone. J Orthop Sci 11:412–423
Hoshi M, Matsumoto S, Manabe J, Tanizawa T, Shigemitsu T, Izawa N, Takeuchi K, Kawaguchi N (2006) Malignant change secondary to fibrous dysplasia. Int J Clin Oncol 11:229–235
Jhala DN, Eltoum I, Carroll AJ, Lopez-Ben R, Lopez-Terrada D, Rao PH, Pettenati MJ, Siegal GP (2003) Osteosarcoma in a patient with McCune-Albright syndrome and Mazabraud’s syndrome: a case report emphasizing the cytological and cytogenetic findings. Hum Pathol 34:1354–1357
Lopez-Ben R, Pitt MJ, Jaffe KA, Siegal GP (1999) Osteosarcoma in a patient with McCune-Albright syndrome and Mazabraud’s syndrome. Skeletal Radiol 28:522–526
Rosenberg ZS, Lev S, Schmahmann S, Steiner GC, Beltran J, Present D (1995) Osteosarcoma: subtle, rare, and misleading plain film features. AJR Am J Roentgenol 165:1209–1214
Ruggieri P, Sim FH, Bond JR, Unni KK (1994) Malignancies in fibrous dysplasia. Cancer 73:1411–1424
Saglik Y, Atalar H, Yildiz Y, Basarir K, Erekul S (2007) Management of fibrous dysplasia. A report on 36 cases. Acta Orthop Belg 73:96–101
Schwartz DT, Alpert M (1964) The malignant transformation of fibrous dysplasia. Am J Med Sci 247:1–20
Xu D, Luan H, Zhan A, Feng W, Sun X, Meng F (1996) Spontaneous malignant transformation of fibrous dysplasia. Chin Med J (Engl) 109:941–945
Yabut SM, Kenan S, Sissons HA, Lewis MM (1988) Malignant transformation of fibrous dysplasia. A case report and review of the literature. Clin Orthop 228:281–289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doganavsargil, B., Argin, M., Kececi, B. et al. Secondary osteosarcoma arising in fibrous dysplasia, case report. Arch Orthop Trauma Surg 129, 439–444 (2009). https://doi.org/10.1007/s00402-008-0669-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-008-0669-8