Abstract
Introduction
Osteochondral transplantations, albeit technically challenging, appear promising not only in knee joint lesions, but also in the treatment of talus lesions. We hypothesized that in patients suffering osteochondral lesions of the talus, favorable outcomes are obtained in patients undergoing primary mosaicplasty as compared to patients undergoing secondary mosaicplasty.
Materials and methods
Over a 3-year period (1998–2001), 14 patients (six male, eight female, median age 22 years) were treated with an autologous osteochondral transplantation of the talus. Eight patients were previously untreated (group I). Six patients had previous ankle procedures, such as microfracturing (group II). The median follow-up was 24 months and 100% complete at 12 months. The functional outcome was evaluated at least at 6 weeks, 12 weeks, and 1 year after surgery using pain on a visual analog scale (VAS) and sports activity was recorded at 1 year after surgery. In ten patients, magnetic resonance imaging (MRI) of the ankle was performed at 1 year after surgery (group I/II: 7/3).
Results
Overall ankle pain was decreased from 6.9 ± 2.1 to 4.0 ± 2.8 postoperatively. The mean knee pain for the donor knee was 2.6 ± 2.4. We found no significant difference between the primary mosaicplasty group and the secondary mosaicplasty group with regard to pain. MRI scans of ten patients showed a complete incorporation of the osteochondral cylinders at 1 year after surgery.
Conclusion
Favorable outcomes were obtained in patients undergoing primary mosaicplasty as compared to patients undergoing secondary mosaicplasty. We found no significant difference among patients with previous ankle surgery in contrast to those without, with a median 24-months follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ankle sprains are common sport-associated injuries with an incidence of one diagnosis per day per 10,000 citizens. Approximately 5% of these sprains result in osteochondral lesions to the talus [10]. Osteochondral lesions of the talus are a relatively common cause of ankle pain and disability [9]. Due to the lack of intrinsic repair mechanisms, the restoration of damaged cartilage in adult humans remains challenging. Different operative and non-operative treatment options for these lesions have been described [2].
Size dependent repair is discussed in the literature [3]. Tissue response techniques (e.g. microfracturing) are recommended for smaller defects. OCT (osteochondral transplantation, e.g. diamond bone cut system or other mosaicplasty devices like OATS) are intended for defects larger than 2 cm2 but these are limited in size by the donor site. The modern procedures like ACT (autologous chondrocyte transplantation following a two step protocol with in vitro multiplication) or MACT (matrix associated ACT) are suitable for the largest defects [3]. Several studies showed good results using mosaicplasty in talar defects, but there is only one study with more than 40 cases [6].
The aim of therapy should be the restoration of joint function and decrease of pain. The surgical repair of osteochondral talus lesions should follow a step-wise protocol:
Reconstruction or stimulation of biological regeneration of the joint surface formed by cartilage is the superior task.
We hypothesized that, among patients with osteochondral lesions of the talus, favorable functional outcomes may be obtained in patients undergoing primary mosaicplasty as compared to secondary mosaicplasty.
Materials and methods
Between April 1998 and March 2001, 14 patients (m/w = 6/8) were treated with an autologous osteochondral transplantation of the talus (r/l = 6/8). The study design was a retrospective cohort study with a level of evidence of IV. The patients’ median age at the time of surgery was 22 years (16–38 years, Table 1). The indications were osteochondrosis dissecans Herde grade III and IV (n = 11) and posttraumatic osteochondral talus lesions (n = 3). The defects were located on the medial aspect of the talus in 11 cases and on the lateral aspect in three cases. The mean defect size was 68.9 ± 32.2 mm2. The defects were measured with an OATS sizer with heads of 5–10 mm diameter. In ten patients, an osteotomy of the medial malleolus was performed to access the cartilage defect. One patient required an osteotomy of the lateral malleolus. During the procedure, six patients were treated with one cylinder, seven with two, and one patient with five.
Donor cylinders were harvested from one of the condyles of the ipsilateral knee joint. Donor cylinders were taken from the medial condyle in 13 patients and from the lateral condyle in one patient.
Operative technique
After initial arthroscopic assessment of the osteochondral talus lesion, a mini arthrotomy of the knee joint was performed. The osteochondral grafts were harvested from the non weight-bearing zone of the medial or lateral femoral condyle using a special drilling chisel (OATS; Arthrex; Naples, FL, USA). The osteochondral talus lesions were debrided and prepared for the grafts. The donor cylinders were implanted using a press fit technique. In most patients, an osteotomy of the medial (n = 10) or lateral (n = 1) malleolus was necessary for appropriate exposure of the talus lesion. For osteotomy of the medial ankle, two drill holes were made. The oblique osteotomy was performed at the transition between the pilon and the medial malleolar joint surface. After the osteochondral transplantation, the medial ankle was fixed with two 3.5 mm screws.
Postoperatively, the patients remained partial weight bearing with full range of motion for 12 weeks.
The mean follow-up was 24 months (12 to 43 months), and 100% complete. At 6 weeks, 12 weeks, and 12 months following surgery, conventional radiographs of the ankle were obtained in two planes. In ten patients, a magnetic resonance imaging (MRI) of the ankle joint was performed 1 year after surgery to evaluate joint congruity, incorporation, and position of the graft. We evaluated clinical parameters such as patient confidence, sports activity, and pain on a visual analog scale (VAS) ranging from 0 to 10 on the follow-ups.
We compared the outcomes between previously operated patients (group II, n = 6) versus primary mosaicplasty (group I, n = 8). The patient characteristics are displayed in Tables 1 and 2.
Group I: previously untreated patients
Group I consisted of three male and five female patients with a mean age of 22 ± 5 years. All were diagnosed with osteochondrosis dissecans tali (ODT). Mean defect size was 69 ± 38 mm2 and we used an average of 1.75 osteochondral cylinders to fill the osteochondral defect.
Group II: previously treated patients
Group II consisted of three male and three female patients with a mean age of 27 ± 8 years. Three patients had posttraumatic (posttr.) osteochondral talus lesions and three patients had ODT. The mean defect size in this group was 55 ± 32 mm2 and we used an average of two osteochondral cylinders to fill the osteochondral defect. The patients had between one and two previous arthroscopies with a cartilage debridement (Table 1).
We compared the VAS pre- and postoperatively using the Mann–Whitney U test, the t test, and the Wilcoxon test.
Results
Pain level
The average preoperative VAS of the ankle was 6.8 ± 2.5 in group I versus 7.5 ± 1.9 in group II (P = 0.228). Postoperatively, the average VAS of the ankle was 4.8 ± 1.8 in group I versus 2.9 ± 2.4 in group II (P = 0.218). The postoperative knee pain was graded higher in group I (3.4 ± 1.7 vs. 1.5 ± 2.8, P = 0.15).
No significant differences were recorded between the two groups for the VAS. A sample size of 40 in each group would have 80% power to detect a probability of 0.681 that a postoperatively VAS in group I was less than in group II using a Wilcoxon (Mann–Whitney) rank-sum test with a P level <0.05.
The mean overall pain score on the VAS was 3.6 ± 2.8 at 1 year after surgery versus 6.9 ± 2.1 (Table 2, Fig. 1, 2). Three patients located their primary pain in the knee joint. The average pain score for the donor knees was 2.6 ± 2.4 in all patients. The average pain score for the ankle was 4.0 ± 2.8 in all patients. No patient included in this series reported regular use of pain medication. Ten patients included in this series reported functional improvement after the surgery and nine patients reported improved participation in sports activities.
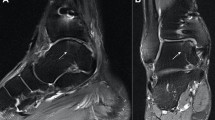
Sample case 3: 16-year-old female. Diagnosis of an osteochondrosis dissecans 1 year prior to the procedure. Radiographs and MRI scans showed, preoperatively (upper scans), the lesion on the medial talus and, postoperatively (scans below), a good incorporation of the transferred cylinder. She improved postoperatively, but still complained of pain and had to stop sports activities
Radiographs
Radiographs of the ankle at 6 weeks, 12 weeks, and 12 months after surgery showed no signs of graft dislocation and good joint congruity in all patients. No radiographic signs of graft necrosis were appreciated. The cylinders were identifiable 1 year postoperatively by X-ray. MRI scans of ten patients showed a complete incorporation, appropriate congruity of the joint surface, and viable transplants.
Adverse effects
No infection, no bleeding, and no re-operations were evident among all included patients during the mean study period of 24 months.
Sports activity
With two exceptions in group I, the sports level was equal in both groups. Only two cases (1 and 4) performed soccer and gymnastic on a competitive level prior to their clinical symptoms.
For group I, four patients (50%) returned to an equal level, two (25%) returned to sport at a lower level and two (25%) had to stop sports. In group II, two (33%) patients returned to the same sports level as before, two (33%) on a lower level, and two (33%) patients had to stop sports.
Discussion
We found no significant differences among patients with previous ankle surgeries in contrast to patients without ankle surgery suffering osteochondral lesions of the talus necessitating mosaicplasty. Clinical outcomes of mosaicplasty appear satisfactory in both previously treated and previously untreated patients.
Osteochondral lesions of the ankle joint remain challenging, as cartilage lesions of the ankle joint are common injuries. Different treatment options have been described in the literature. Mosaicplasty of the talus appears to be a promising treatment option and recent publications suggested promising results, albeit it is a technically demanding procedure [1, 4, 6–8]. Autologous osteochondral grafts have some advantages over allografts, including no threat of disease transmission, high survival rate of the grafted chondrocytes, and reliability of bone union. Accepted disadvantages are limited supply of autologous tissue, morbidity or adverse effect on joint function of graft harvest, fixed age of the donor, and the difficulty of matching topology of graft to recipient site. The latter problem may be circumvented by using multiple small plugs, implanted like tiles that can contour to the desired surface curve more easily than one large graft.
The results in other studies of osteochondral autograft transplant for lesions of the talus demonstrate good to excellent postoperative ankle scores including improvement of pain and function with minimal knee donor site morbidity. However, this technique has disadvantages regarding efficiency in surface reconstruction with the harvested grafts. But histological and clinical outcome seems to be superior to the other treatment choices [6].
Our 14 patients were divided into two groups to compare mosaicplasty of the talus in previously treated and untreated chondral lesions. Both groups improved due to the procedure. By comparing the VAS of both groups with previously operated patients (group I), we were unable to demonstrate a significant difference caused by the small case number and high standard deviation. Series with more than 40 patients have been only published by Hangody [5].
We can confirm the promising results of the larger series with long-term experience of Hangody and Fules [6]. We agree with other previously published results that primary treatment of osteochondral lesions of the talus should be arthroscopic and the described procedure is reserve for failed previous surgery [9]. It was not possible to demonstrate an advantage in one of the two relatively small patient groups; therefore, we found that previous ankle surgery is not per se a deteriorating factor in mosaicplasty.
A size dependent indication algorithm needs to be reviewed carefully. Defects can only be seen in relation to the total body as joints of people with the same BMI and different heights might have very different joint surface sizes in absolute numbers. There are many techniques that have been attempted to repair osteochondral lesions as the ones described in the “Introduction”. However, all results have demonstrated tissue regeneration below articular cartilage quality.
Our favorable early results and those of other authors using similar techniques may validate osteochondral transplantation as a viable, alternative secondary procedure for treating unstable osteochondral defects in the talus that are refractive to more commonly used surgical techniques. Larger prospective, randomized studies with long-term follow-up providing a higher level of evidence are pending currently. These can usually not be provided for surgical procedures. Multicenter studies could improve the small amount of patients undergoing mosaicplasty in a single institution.
The majority of our patients had to return to sports on a lower level or even to stop sports. Although, the previously untreated patients did slightly better, the overall outcome demonstrated that the results of the procedure are not that satisfying and should be only a secondary option. The limitations of our study were the small sample size and no control group.
The success of the procedure depends largely on the adherence to proper indication and attention to technical details. Mosaicplasty of the talus appears to be a promising treatment option with promising results. A larger series is necessary to develop a proper treatment algorithm prior to recommending a stepwise surgical treatment pathway, with mosaicplasty as a reserve procedure. This study could contribute some preliminary results in focusing on such a standard.
We found no significant difference among patients with previous ankle surgery in contrast to those without undergoing OATS procedure for osteochondrosis dissecans with a median 24-months follow-up.
References
Baltzer AW, Arnold JP (2005) Bone-cartilage transplantation from the ipsilateral knee for chondral lesions of the talus. Arthroscopy 21:159–166
Evans CH (2005) Novel biological approaches to the intra-articular treatment of osteosarthritis. Biodrugs 19:355–362
Giannini S, Vannini F (2004) Operative treatment of osteochondral lesions of the talar dome: current concepts review. Foot Ankle Int 25:168–175
Giannini S, Vannini F, Buda R (2002) Osteoarticular grafts in the treatment of OCD of the talus: mosaicplasty versus autologous chondrocyte transplantation. Foot Ankle Clin 7:621–633
Hangody L (2003) The mosaicplasty technique for osteochondral lesions of the talus. Foot Ankle Clin 8:259–273
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85-A(Suppl 2):25–32
Kish G, Modis L, Hangody L (1999) Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete. Rationale, indications, techniques, and results. Clin Sports Med 18:45–66, vi
Kolker D, Murray M, Wilson M (2004) Osteochondral defects of the talus treated with autologous bone grafting. J Bone Joint Surg Br 86:521–526
Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Henle P, Niemeyer P (2006) Mosaicplasty with autogenous talar autograft for osteochondral lesions of the talus after failed primary arthroscopic management: a prospective study with a 4-year follow-up. Am J Sports Med 34:55–63
Seil R, Kohn D (2001) Osteochondral lesions of the talus––a rarity? Orthopade 30:1–2
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haasper, C., Zelle, B.A., Knobloch, K. et al. No mid-term difference in mosaicplasty in previously treated versus previously untreated patients with osteochondral lesions of the talus. Arch Orthop Trauma Surg 128, 499–504 (2008). https://doi.org/10.1007/s00402-007-0513-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0513-6