Abstract
Introduction
Dorsally displaced fractures of the distal radius fractures are one of the commonest in day-to-day practice. There is still no consensus among surgeons regarding the suitability of using volar or the dorsal cortex as basis for internal fixation for dorsally displaced fractures.
Background
We report an anatomical study, which compares the thickness of the volar and dorsal cortices of cadaveric adult radii using digital photography.
Results
Results of this study show that the volar cortex was statistically, significantly thicker than the dorsal cortex. We believe that the volar cortex may behave as the calcar of the distal radius and hence internal fixation devices applied to the volar cortex may provide a more stable internal fixation compared to those based on the dorsal cortex.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the distal radius are among the most common of all skeletal injuries [5]. The distal end of the radius is the anatomic foundation of the wrist joint [6]. The distal end of the radius was only recently named Crinis radii (Crinis = tail of a comet or rays of the sun) [11]. Although, high resolution MRI and digital X-ray has been used to assess the bone density of the distal radius, as far as we are aware, no anatomical study has been done to look at the bony architecture of the distal radius [1, 12]. Debate still continues among surgeons regarding the suitability of the volar or the distal cortices regarding the application of implants [2, 4, 9, 10]. The aim of the study is to compare the thickness of the volar and distal cortices at 0, 5 and 10 mm from the articular surface. We suggest the possible reasons for the difference noted in the study. We make suggestions which might provide the mechanical basis for internal fixation of the distal radius.
Materials and methods
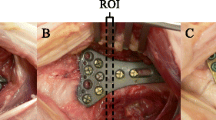
Ten adult distal radii were obtained from preserved anatomic specimens. Three specimens had to be discarded due to the presence of previous fractures. The remaining specimens were stripped off all soft tissues and were sectioned at 0, 5 and 10 mm from the articular surface using a 0.5 mm thick band saw (Fig. 1). This gave three sections each with a proximal and distal surface. Each of the surfaces of these cross-sections were digitally photographed and images analysed using Adobe Photo Shoppe™ (accuracy 0.05 mm). To measure the thickness of volar and dorsal cortices, three points were identified on the dorsal and volar cortices of each surface of the two sections (Fig. 2). Forty-two paired points were marked on the dorsal and the volar cortices of both surfaces of each specimen (Fig. 3). Four paired points were marked on the medial and the lateral cortices of both the surfaces of each specimen. An average value of the thickness each cortex was calculated and was used to represent the thickness of each cortex. A two-tailed t test was used to statistically interpret the results.
Results
Table 1 details the findings of this study. The results indicate that the volar cortex is statistically, significantly thicker than the dorsal cortex at the level of 0, 5 and 10 mm from the articular surface (P < 0.05). There was no statistical difference between the thickness of the lateral and the medial cortices in any of the specimens. By comparing the values we have eliminated the error which can occur due to magnification or downsizing of the thickness of the cortices.
Discussion
Structural anatomy of the distal radius has been a subject of previous studies using MRI relaxometry [1] and computer-assisted analysis of digital plain x-rays [12]. The latter technique is still deemed to be experimental [12]. Dual energy absorptiometry is a commonly used method to evaluate skeletal status in clinical practice but it cannot distinguish between trabecular and cortical bone [1]. High resolution MR scan can give information of the trabecular bone structure in vivo and in vitro but has it not yet been used to measure the thickness of the various cortices of the distal radius [1].
Our study shows that the volar cortex was statistically significantly (P < 0.001) thicker than the dorsal at 0, 5 and 10 mm from the articular surface. By comparing the values rather than using the absolute values, we have eliminated the error which can occur due to magnification or downsizing of the thickness of the cortices.
We believe that the significantly thick volar cortex may be due to more compressive force being transmitted via the volar cortex than the dorsal cortex (Hunter’s law). We were unable to find any statistically significant difference in the thickness of the volar cortex at the radial and ulnar borders of any of the cross-sections. A previous cadaveric study has suggested that dorsal plating cannot totally restore the axial, loading transmission pattern [13].
Although our study has looked at only the thickness of the volar cortex, the authors are aware that other factors like the blood supply to the distal fragment and the use of locking/non-locking plates also influence the decision regarding the location of the plate on the distal radius. The volar approach to the wrist has also been shown to preserve the vascular supply and the dorsal periosteum of the dorsal metaphyseal fragments [9]. In the volar approach, the pronator quadratus protects the flexor tendons by forming a barrier between the implant and the flexor tendons [9]. Previous studies have shown that unicortical volar plates used to fix comminuted dorsally displaced fractures are subjected to significant axial and bending loads leading to failure of fragment fixation and recurrence of the deformity [8]. Other biomechanical studies have since confirmed the superiority of the bicortical fixation devices applied on the volar cortex of the distal radius [3]. Liporace et al. [7] compared the biomechanical stability of standard dorsal non-locked T plate to a volar non-locked plate in a simulated model of a dorsally unstable distal radius fracture. They demonstrated that a fixed angle volar locked plate has significantly greater stiffness than dorsally applied standard T plates [7].
We believe that the volar cortex behaves as the Calcar of the radius, and that restoration of its continuity and anatomy may be crucial in maintaining the reduction of the distal radii fracture. The significant thickness of the volar cortex compared to the dorsal cortex may allow fixation devices to have a good hold.
References
Brismar TB, Budinsky L, Majumdar S (2001) Evaluation of trabecular bone orientation in wrists of young volunteers using MR relaxometry and high resolution MRI. Adv Exp Med Biol.496:1–7
Campbell DA (2000) Open reduction and internal fixation of intraarticular and unstable fractures of the distal radius using the AO distal radius plate. J Hand Surg Br 25(6):528–534
Drobetz H, Kutscha-Lissberg E (2003) Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop 27(1):1–6
Herron M, Faraj A, Craigen MAC (2003) Dorsal plating for displaced intra-articular fractures of the distal radius. Injury 34:497–502
Jupiter JB (1991) Current concepts review fractures of the distal end of the radius. J Bone Joint Surg Am 73-A:461–469
Jupiter JB (1997) Complex articular fractures of the distal radius classification and management. J Am Acad Orthop Surg 5(3):119–129
Liporace FA, Gupta S, Jeong GK, Stracher M, Kummer F, Egol KA, Koval KJ (2005) A biomechanical comparison of a dorsal 3.5-mm T-plate and a volar fixed-angle plate in a model of dorsally unstable distal radius fractures. J Orthop Trauma 19(3):187–191
Orbay JL (2000) The treatment of unstable distal radius fractures with volar fixation. Hand Surg 5(2):103–112
Orbay JL, Fernandez DL (2002) volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg 27A(2):205–215
Osada D, Viegas SF, Shah MA, Morris RP et al (2003) Comparison of different distal radius dorsal and volar fixation plates: a biomechanical study. J Hand Surg 28A(1):94–104
Riet RV, Glabbeek FV, Bortier H (2002) Crinis radii. A name for the distal radius. Clin Anat 15:375–376
Trippi D, Chimenti M, Bozzi R (1993) A computer assisted method for the study of the trabecular bone of the distal radius on conventional radiographs. J Digit Imaging 6(2):140–147
Zhu L, Ho H, Lu W, Leung F, Chow SP (2002) A cadaveric model for biomechanical study of fixation methods for AO type C2 fractures of the distal radius: design and testing with dorsal plating fixation. Hand Surg 7(2):279–283
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dhillon, S.S., Kumar, A.J.S., Sadaiyyappan, V. et al. Anatomical study comparing the thickness of the volar and dorsal cortex of cadaveric adult distal radii using digital photography. Arch Orthop Trauma Surg 127, 975–977 (2007). https://doi.org/10.1007/s00402-007-0394-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0394-8