Abstract
Introduction: Single buttress plating laterally was sometimes performed by a few orthopedists to treat complex tibial plateau fractures with medial compartment involvement. However, we might encounter cases with medial compartment collapse due to such treatment. The causes of failure, the technique of the revision surgery, and the methods of prevention were investigated retrospectively. The purpose of this study was to report our clinical results of a retrospectively followed series of patients treated with blade plate fixation for proximal tibial metaphyseal nonunions and malunions which were treated with unilateral plating. Materials and methods: Twenty-eight patients with failed treatment of complex tibial plateau fractures due to single buttress plating laterally underwent the revision surgeries. Removal of the buttress plate, proximal tibial corrective osteotomy, and insertion of an angled blade plate medially were performed. Postoperatively, exercise of the range of motion of the knee was encouraged as early as possible. Results: Twenty-five patients were followed-up for a median of 4.8 years (range, 1.2–6.8), and all fractures healed at a median of 4.0 months (range, 3.0–6.0). The proximal medial tibial angle (PMTA) was corrected to the acceptable range (80–99°) in all 25 patients (P<0.001) and knee function improved in 22 out of 25 patients (P<0.001). Conclusion: For clinical and biomechanical considerations, single buttress plating laterally was unsuitable for complex tibial plateau fractures with medial compartment involvement due to relatively huge compressive loads on the medial compartment. The stability provided by a few screws of the buttress plate laterally was normally insufficient. An angled blade plate could be a useful armament in the management of metaphyseal nonunion and malunions of the proximal tibia. Its better stabilization could normally provide a high success rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tibial plateau fractures are not uncommon, which may be caused by either high or low energy injuries. Because of poor regenerative ability of injured articular cartilage, the principal treatment method for tibial plateau fractures normally focuses on maintaining normal knee alignment, reconstructing articular bony congruity, and providing sufficient stability [3, 11, 18]. Early exercise of the range of motion (ROM) for the knee is believed to have the best functional outcome.
Tibial plateau fractures are divided by Schatzker into six types [14, 18]. Displaced fracture fragments may be reduced by various open or arthroscopic techniques and then stabilized by various internal or external fixators [18]. Although plating treatment has achieved much support, operative complications are common, especially deep infection [1, 17, 20]. Minimizing soft tissue dissection and reducing numbers of inserted plates were recommended in the literature [18]. Moreover, single plating laterally had achieved some support [6, 11]. However, under such a situation fragment stability may be vulnerable. In the author’s outpatient department (OPD), patients sometimes encounter medial compartment collapse due to single buttress plating laterally. A revision surgery had to be performed to resume the normal knee alignment and regain the normal walking ability. Recently, single less invasive stabilization system (LISS) plate with lateral placement had been reported with a great success [3, 6, 11, 15]. After all, its use was still not wide due to expensiveness [13]. On the other hand, supplement with buttress plating medially may further damage the skin vitality [1, 20].
The purpose of this study was to report our clinical results of a retrospectively followed series of patients treated with blade plate fixation for proximal tibial metaphyseal nonunions and malunions which were treated with unilateral plating. A more integrated principle to treat such complex fractures might then be established.
Patients and methods
From May 1995 to April 2001, 28 consecutive adult patients (>15 years) with failed treatment of tibial plateau fractures due to single buttress plating laterally were treated with revision surgery at our institution. Patients’ median age was 32 years (range, 19–56), with a male to female ratio of 5:2. All fractures were caused by motorcycle or car accidents and were finally treated with single buttress plating laterally at various hospitals. The period from the injury to our revision surgery was a median of 12 months (range, 6–24). The fractures were operated for 1–3 times but all failed. Twenty-two patients required the use of a cane or crutches for ambulation. Three fractures had a history of deep infection but subsided after debridement and antibiotic treatment. Patients whose fractures were treated conservatively or by other techniques were excluded.
At the OPD, the operative wound at the knee was carefully inspected and no deep infection was noted at that time. The ROM for the knee was a median of 120° (range, 80–140). All knees revealed various degrees of varus deformity and were unstable during the physical examination. The plain radiographs of anteroposterior and lateral views of the knee were checked. All 28 fractures revealed various degrees of varus angulation at the proximal tibia and 14 fractures had healed.
At admission for revision surgery, complete blood cell (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) were routinely checked. Cases with latent infection would be treated with external fixation and excluded from this study. In this study, the data of all 28 cases were within normal range.
Surgical technique
Under spinal anesthesia, patients were placed on the operating table in the supine position. A pneumatic tourniquet was routinely used.
A midshaft fibulotomy was first performed. A midline longitudinal skin incision over the anterior knee and the upper tibia was performed. The prior plate at the proximal tibia was removed. A transverse tibial osteotomy just distal to the tibial tubercle was performed with a power saw. Then, the lower extremity axis was realigned to maintain the medial edge of the knee and the medial malleolus at the midline. After the contour of the medial aspect of the tibia was trimmed with a power saw, a 95° angled blade plate (Synthes, Bettlach, Switzerland) was inserted at the medial aspect of the tibia. The orientation of the blade was toward the upper margin of the fibular head. At least four cortical screws need to be inserted for the distal fragment. Massive cancellous bone graft procured from the lateral aspect of the proximal tibia was packed in the fracture gaps.
The stability was checked and the wound was closed with absorbable sutures. Postoperatively, a long leg splint was applied for 3 weeks in cases with suspicious stability. All patients were permitted to ambulate with protected weight bearing as early as possible. Exercise of the ROM for the knee was encouraged.
Patients were followed up at the OPD in 4–6 week intervals. The clinical and radiographic fracture healing processes and complications were recorded. Crutches could be discontinued only after the fracture had healed. After the fracture healed, patients were advised to follow-up annually and whenever necessary.
In this study, fracture union was defined: clinically, there was no pain and tenderness, and patients could walk without support; radiographically, the trabeculae had bridged both fragments [5]. Nonunion was defined: the fracture was still ununited after 1 year treatment.
For the convenience of comparison, Fisher’s exact test or paired Student’s t test was used. Statistical significance was set at P<0.05. Knee function was evaluated with Mize’s criteria and divided into four grades. A satisfactory outcome included an excellent or good grade [9].
Correction of varus deformity of the knee was evaluated with the proximal medial tibial angle (PMTA) [12]. It was the intersecting angle between the tibial articular surface and the axis of the distal fragment. Normally, it was 87°±2°. Malunion was defined: the fracture healed with the PMTA of less than 80° or more than 99°. In this study, 14 cases were malunion and other 14 cases were nonunion preoperatively.
Results
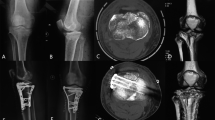
Twenty-five patients were followed up for a median of 4.8 years (range, 1.2–6.8) and three patients were lost to regular follow-up despite our best efforts to contact them. All 25 fractures healed at a median of 4.0 months (range, 3.0–6.0; Figs. 1, 2, 3). One of the three patients lost to follow-up had fracture union at 4.0 months but no follow-up continued. The other two patients were immediately lost postoperatively.
Case 1. A 42-year-old man sustained a left bicondylar tibial plateau fracture and was treated with single buttress plating laterally. Malunion and medial compartment collapse with the proximal medial tibial angle (PMTA) of 70° occurred for 12 months. Revision surgery with the PMTA of 90° was performed. At 6.8 years follow-up, the PMTA was 88° and knee function was excellent
Case 2. A 56-year-old man sustained a left bicondylar tibial plateau fracture and was treated with single buttress plating laterally. Nonunion and medial compartment collapse with the PMTA of 68° occurred for 8 months. Revision surgery with the PMTA of 88° was performed. At 6.5 years follow-up, the PMTA was 85° and knee function was excellent
Case 5. A 48-year-old man sustained a right bicondylar tibial plateau fracture and was treated with single buttress plating laterally. Malunion and medial compartment collapse with the PMTA of 74° occurred for 15 months. Revision surgery with the PMTA of 88° was performed. At 5.8 years follow-up, the PMTA was 86° and knee function was good
Before the revision surgery, the PMTA in 25 patients was a median of 72° (range, 65–82). Postoperatively, the PMTA improved to a median of 90° (range, 86–93; P<0.001). At the latest follow-up, the PMTA became a median of 88° (range, 84–92; P<0.001; Table 1).
Before the revision surgery, knee function in 25 patients was unsatisfactory. At the latest follow-up, 22 patients became satisfactory (P<0.001). Three patients were with unsatisfactory outcomes due to irregular various degrees of knee pain and less than 90° of knee flexion. Therefore, knee arthroplasty was suggested whenever necessary. There were no nonunion, wound infection, skin slough, and malunion.
Discussion
During the stance of a gait cycle, the human knee will sustain loads of at least three times the body weight [10]. In addition, 60–75% loads will cross the medial tibial plateau [4, 8, 16]. Therefore, the medial compartment normally sustains relatively huge compressive loads during the daily activity. Although traditionally a plate is placed on the lateral side to fit for the tension band principle [19], the medial compartment stability provided by a few screws inserted from the lateral side is vulnerable. Clinically, collapse of the medial tibial compartment is not uncommon. In this study, the normal range of valgus knee was broadened according to the same consideration. Ten degrees of valgus knee was still accepted but only 5° was permitted for varus knee (80°–99° of the PMTA was considered normal) [7].
Once the medial tibial compartment collapses, open reduction may make fragments more comminuted. Osteotomy with realignment of the proximal tibia should be a better choice. In the present series, insertion of an angled blade plate at the medial aspect of the tibia had provided sufficient stability until the fracture healed [2]. Local cancellous bone graft could vanish the fracture gap and promoted the fracture healing process.
In the literature, dual plating on both the medial and the lateral aspect of the tibia had been supported for complex tibial plateau fractures with bicondylar involvement [1, 18]. However, the relatively more extensive soft tissue dissection might induce a high infection rate [1, 20]. Therefore, a single plate was advocated by some orthopedists [6, 11]. In addition, they supported the plate that was inserted on the lateral aspect of the tibia to avoid endangering the skin vitality medially. If a LISS plate was used, the result was considered excellent [3, 15]. However, if a LISS plate is unavailable, from the biomechanical viewpoint, a buttress plate should be inserted from the medial side. Thus, the medial compartment can achieve a better stability due to the support of the plate and screws. Because the lateral tibial plateau only sustains 25–40% loads, supports by screws inserted from the medial side might be sufficient. In other words, a single buttress plate medially for complex tibial plateau fractures may be sufficient. Therefore, the buttress plate should be inserted from the medial side if the medial compartment is involved and not from the lateral side. The greatest disadvantage of plating medially is the skin problems associated with acute fractures. If insertion of buttress plates medially is prohibited, reinforcing devices, such as external fixation, may be supplemented to augment buttress plating laterally.
In the present series, an angled blade plate was used for the revision surgery (Figs. 1, 2, 3). Normally, the bone stock after failed plate treatment was so osteoporotic, comminuted, and deficient as to cancellous screws may not provide the sufficient stability. Under this situation, a blade is better than screws to provide the better stability [2]. Insertion of 95° angled blade plate on the medial aspect of the proximal tibia is not difficult technically. First the tibial alignment is well maintained. With the blade placed toward the fibular head, the angled blade plate is inserted parallel to the medial cortex of the tibia. Normally, the proximal fragment can only be stabilized with the blade and one or two cancellous screws. The distal fragment is stabilized by four cortical screws. Usually, the stability is sufficient until the fracture is healed. Should severe osteoporosis be noted, short-term splint immobilization can be supplemented. The outcomes are generally satisfactory.
In conclusion, for the clinical and biomechanical considerations, single buttress plating laterally is unsuitable for complex tibial plateau fractures with medial compartment involvement. A single buttress plate should be inserted on the medial aspect of the tibia and the success rate may increase. If plating medially cannot be performed due to the skin condition, reinforcing devices should be supplemented for a certain time. For cases with failed plate treatment laterally, an angled blade plate (where a LISS plate is unavailable) inserted from the medial side after corrective osteotomy of the proximal tibia is performed which can achieve a high success rate.
References
Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK (2004) Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 18:649–657
Carpenter CA, Jupiter JB (1996) Blade plate reconstruction of metaphyseal nonunion of the tibia. Clin Orthop 332:23–28
Cole PA, Zlowodzki M, Kregor PJ (2004) Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma 18:528–535
Coventry MB (1988) Proximal tibial osteotomy. Orthop Rev 17:456–458
DeLee JC, Heckman JD, Lewis AG (1981) Partial fibulectomy for ununited fractures of the tibia. J Bone Joint Surg Am 63:1390–1395
Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ (2004) Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma 57:340–346
Freeman EL, Johnson EE (1995) Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop 315:25–33
Hsu RW, Himeno S, Coventry MB, Chao EY (1990) Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop 255:215–227
Mize RD, Bucholz RW, Grogan DP (1982) Surgical treatment of displaced, comminuted fractures of the distal end of the femur: an extensile approach. J Bone Joint Surg Am 64:871–879
Mow VC, Proctor CS, Kelly MA (1989) Biomechanics of articular cartilage. In: Nordin M, Frankel (eds) Basic biomechanics of the musculoskeletal system. Lea & Febiger, Philadelphia, pp 31–58
Mueller KL, Karunakar MA, Frankenburg EP, Scott DS (2003) Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop 412:189–195
Paley D, Maar DC, Herzenberg JE (1994) New concepts in high tibial osteotomy for medial compartment osteoarthritis. Orthop Clin North Am 25:483–498
Ricci WM, Rudzki JR, Borrelli J Jr (2004) Treatment of complex proximal tibia fractures with the less invasive skeletal stabilization system. J Orthop Trauma 18:521–527
Schatzker J, McBroom R, Bruce D (1979) Tibial plateau fractures: the Toronto experience 1968–1975. Clin Orthop 138:94–104
Stannard JP, Wilson TC, Volgas DA, Alonso JE (2004) The less invasive stabilization system in the treatment of complex fractures of the tibial plateau: short-term results. J Orthop Trauma 18:552–558
Tew M, Waugh W (1985) Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg Br 67:551–556
Tscherene H, Lobenhoffer P (1993) Tibial plateau fractures: management and expected results. Clin Orthop 292:87–100
Whittle AP, Wood GW II (2003) Fractures of lower extremity. In: Canale ST (ed) Campbell’s operative orthopedics. CV Mosby, Philadelphia, pp 2725–2872
Wood GW II (2003) General principles of fracture treatment. In: Canale ST (ed) Campbell’s operative orthopedics. CV Mosby, Philadelphia, pp 2669–2723
Young MJ, Barrack RL (1994) Complications of internal fixation of tibial plateau fractures. Orthop Rev 23:149–154
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, CC. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch Orthop Trauma Surg 126, 82–87 (2006). https://doi.org/10.1007/s00402-006-0106-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-006-0106-9