Abstract
Introduction: The aim of this study is to evaluate the effectiveness of the Ponseti method in children presenting before 1 year of age with either untreated or complex (initially treated unsuccessfully by other conservative methods) idiopathic clubfeet. Patients and methods: The authors report 134 feet of 92 patients with Dimeglio grade 2, 3, or 4 deformities treated with the Ponseti method. Twenty-four percent of feet were of complex deformities at initial presentation to the authors’ clinics. Results: At a mean follow-up of 46 months (range 24–89) we avoided joint release surgery in 97% of feet. Sixty-seven percent required a percutaneous tenotomy of the Achilles tendon. Relapse rate was 31% (41 feet). We treated 2 relapses by restarting the use of orthosis, 17 with re-casting, 18 with anterior tibial tendon transfer following a second relapse, and 4 feet with extensive joint surgery. Compliance with the use of orthosis was identified as the most important risk factor (P<0.0001) for relapses. Previous unsuccessful treatment attempts by other conservative methods did not adversely affect the results unless the cases had iatrogenic deformities. Cases with iatrogenic deformities from previous treatment had a significantly increased risk of non-compliance and relapse. Experience of the treating surgeon and cast complications were also related to relapses. Conclusion: Our results show that the Ponseti technique is reproducible and effective in children at least up to 12 months of age. It can also produce good correction in children presenting with complex idiopathic deformities. Therefore, extensive joint releases should not be considered immediately in such cases. The treating surgeon should be meticulous in using the technique and ensure compliance to foot abduction brace in order to avoid recurrences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clubfoot is one of the most common foot deformities and may impede the child’s development when not treated successfully, causing much frustration to the family and the physician. Traditionally, joint releases [5, 27, 33, 36] are recommended for the treatment of congenital idiopathic clubfeet if correction of the foot using conservative methods within 3–6 months is not satisfactory [14, 26]. This approach clearly has the advantage of complete correction in one attempt with good early results. However, reports of more conspicuous anatomical changes, significant muscle weakness, and insufficient ankle range of motion led to a growing concern regarding the long-term outcome in patients treated with extensive surgical releases [9, 18, 21]. Functional results have been reported to be better if extensive surgery could be avoided [1, 2]. Other causes of concern in surgically treated patients are reoperations required in more than half of the patients, and the risk of serious complications which are sometimes more difficult to treat [1–4, 8, 12, 17, 26, 34].
On the other hand, inappropriate manipulations and castings as described in various conservative treatment methods cause incomplete correction and in some cases secondary damage to the foot skeleton. Hence, a generally achievable correction rate with conservative methods was believed to be low, and insistence with manipulations was discouraged [12, 27].
However, favorable long-term results were reported with the Ponseti technique [7, 23]. The Ponseti technique includes gentle manipulations followed by well-molded, weekly casts extending to the thigh. The cavus is corrected first by elevating the first metatarsal aligning the forefoot with the heel. Correction of varus and adduction is achieved by gradually abducting the foot in supination under the head of the talus. If there is a persistent equinus when 60–70° of foot abduction and correction of heel varus are achieved, a percutaneous Achilles tenotomy is performed. After the tenotomy, a final cast is applied for 3 weeks. To prevent relapses, a foot abduction brace is used full-time for the first 3 months and at nighttime until the child is 3–4 years of age.
Recent studies, from other centers, reported that the Ponseti technique was successful in avoiding extensive surgery in approximately 95% of virgin clubfeet [6, 16, 18, 24]. However, a certain number of clubfoot patients present to out-patient clinics with either late or so-called resistant deformities. Decision to treat these deformities with extensive surgery is empirical and based on limited success with conservative treatment methods other than the Ponseti. Encouraged by their early experiences, authors have started using the Ponseti method in all clubfoot patients presenting up to the age of 1 year. The purposes of this study are to evaluate the effectiveness of the Ponseti technique in correcting not only untreated but also complex clubfeet (initially treated unsuccessfully by other conservative methods), to examine the effect of the learning curve, and to identify the factors related to relapses for a successful result in the short-term.
Patients and method
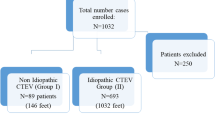
We treated 134 feet of 92 patients with idiopathic congenital clubfeet with the Ponseti method between January 1997 and September 2002. Criteria for inclusion in this study were the severity of the deformity (Grade 2, 3, or 4 according to Dimeglio classification) [10], patients under 1 year of age when the Ponseti treatment was started, with a minimum follow-up of 24 months after the completion of casting. Four feet of three patients were lost to follow-up and were excluded from this study. These patients were noted to have an excellent correction at 5–9 months follow-up. Therefore, the follow-up rate was 97%.
The mean age at the time of last follow-up was 50 months (range 26–94 months). Mean follow-up, defined as from removal of the last cast to the final evaluation, was 46 months (24–89 months).
The patients were grouped based on two criteria; previous treatment and experience of treating surgeon. Patients who had not received any treatment before were defined as untreated. Patients previously treated by conservative methods other than the Ponseti were defined as having complex clubfeet. Three groups were then identified according to previous treatment: Group A untreated clubfeet, Group B complex clubfeet without iatrogenic deformity, and Group C complex clubfeet with iatrogenic deformity. All complex deformities were considered “resistant” to non-operative treatment elsewhere and recommended extensive joint releases. Two other groups were identified to examine the effect of learning curve on the outcome: early experience group comprised the first 20 patients treated by each of the two treating surgeons (40 patients in total); later experience group comprised patients treated after the learning curve. Distribution of several patient characteristics and deformity grades within each group are shown in Table 1.
At presentation, each clubfoot was graded using the Dimeglio classification system. Only children with moderate (Grade 2), severe (Grade 3), and very severe (Grade 4) types of congenital idiopathic clubfeet were included in this study.
Treatment protocol
Manipulations were performed exactly as described by Ponseti [31] in untreated cases and complex cases without iatrogenic deformities. A different approach was used in complex cases with iatrogenic deformities. If the iatrogenic deformity was identified on removal of a cast done elsewhere and the condition of the foot looked inappropriate to continue with another cast (shortened and swollen foot, maceration, etc.), it was left out of cast for about 2 weeks. Manipulations were customized according to anatomical identification of the iatrogenic components of the deformity determined with a careful clinical examination of the foot. Afterwards, treatment continued as described. Either a semi-rigid synthetic cast (Soft Cast, 3M) or a plaster of Paris cast was used depending on the preference of the treating surgeon. The percutaneous Achilles tenotomy was performed under general anesthesia in some patients while in the others it was performed in the out-patient clinic using local anesthesia. Rarely, a cast change at 1 week was considered necessary to improve ankle dorsiflexion following the last cast after the tenotomy. We used a Denis Browne bar for the foot abduction brace. The foot-plates were removed and the shoes were attached directly to the bar in order to reduce the weight of the brace.
Compliance was assessed as reported by the parents, and non-compliance was defined as cessation of brace wear.
Relapses were defined as a Dimeglio score of equal to or more than five points, dorsiflexion less than 15°, or any apparent forefoot adduction or heel varus not reducible beyond neutral by gentle manipulation. Relapses were initially treated with re-casting. If a second relapse occurred and there was dynamic supination after any structural deformity had been corrected with casting, tibialis anterior tendon was transferred to the lateral cuneiform.
At follow-up, we evaluated the feet by both Dimeglio and Pirani scores. Triceps surae strength was clinically assessed by the children’s ability to stand or walk on toes, whichever is allowed by their cooperation.
Avoidance of extensive releases, and relapses were the main factors in the assessment of results. Successful treatment was defined as avoidance of extensive surgery (posterior, posteromedial, or complete subtalar releases). Data were further analyzed regarding possible causes of relapses.
Statistical analysis
Each foot was considered a case for statistical analysis. Fisher’s exact test (one-sided) was used to determine statistical differences between the treatment groups and the experience groups. We performed Kaplan–Meier survival analysis to relate the following variables to relapses: the severity of the deformity at presentation, number of Ponseti casts, need for Achilles tenotomy, previous treatment, age of patient at the start of treatment, and compliance with the use of orthosis. Log-rank test was used for comparing the equality of survival distributions.
Results
At a mean follow-up of 46 months, joint releases (posterior, postero-medial, and complete subtalar release) were avoided in 130 of 134 feet (97%) and in 88 of 92 (96%) patients treated using the Ponseti technique. Ninety clubfeet (67%) required a percutaneous tenotomy of the Achilles tendon.
Subsequently, the deformity relapsed in 41 feet (31%) of 27 patients. Two of these relapses were mild and responded to restarting the use of orthosis, whereas 35 had recasting for correction of first relapses. Five feet of four cases required repeat Achilles tenotomies. Eighteen feet (12 patients) had second relapses and required anterior tibial tendon transfer to the third cuneiform. Parents of two patients (two feet) refused recasting because of skin problems during initial castings. Four feet (3%) of four cases (4%) underwent joint releases.
Thirty-nine patients (57 feet) were not compliant with the use of foot abduction orthosis. The overall rate of compliance of patients was 58%. Rate of recurrence was 3% in cases compliant with the use of orthosis, whereas it was 68% in non-compliant cases.
There were cast complications in 12 feet (8.95%) of nine patients (9.78%). Intolerance to and frequent slippage of casts were seen in three feet of two patients. There was a pressure necrosis in one foot, and cast saw cuts in four feet (three patients). Oedema and skin problems interrupting with serial casting were observed in four feet (three patients).These complications were encountered in the early cases.
The results of groups were compared to each other and several statistically significant differences were noted (Table 2). Group B patients could be corrected with less number of casts as compared to the other treatment groups. Non-compliance and relapses were more frequent in both Group C and early experience group. Cases in these groups also required more number of casts. All patients who had joint releases were in the early experience group. This group also had more cast complications and worse Dimeglio scores. Cast complications were also associated with non-compliance with the foot abduction orthosis (Fisher’s exact test, P=0.003).
Statistical analysis of relapses, related to several variables (Table 3), identified compliance to foot abduction orthosis, cast complications interfering with serial casting, and experience of the treating surgeon as factors most significantly associated with relapses. Relapses occurred in only 3% of patients compliant with orthosis and 68% of patients non-compliant with orthosis.
At final follow-up, the ankle joint motions (mean ± standard error; range) were 23°±7.65° (10–40) of dorsiflexion and 49°±6.23° (30–60) of plantar flexion. The mean Dimeglio score was 2.68±0.16 (0–7) and the mean Pirani score was 0.37±0.05 (0–2.5).
Discussion
Using the Ponseti method, we have been successful in avoiding extensive surgery in 97% of congenital idiopathic clubfeet. This success rate is comparable to the other series reporting early results of the Ponseti method [6, 11, 16, 24].
Our results also show that the Ponseti method can be used for the treatment of both untreated and complex clubfeet in children at least up to the age of 12 months and still produce a high correction rate. From the institution where the Ponseti technique was developed and used for several decades, Morcuende et al. reported their results in a similar patient population [28]. At a mean age of 26 months (6 months to 8 years) at last follow-up, only 2.5% of cases required extensive surgery. They concluded that the Ponseti method could be used successfully in children up to approximately 2 years of age when no previous surgical treatment has been attempted. Our study from a different country with a different healthcare system demonstrates the reproducibility of the technique in this expanded patient population at a mean age of 50 months at last follow-up.
In our series, the indications for extensive surgery were parents refusing further casts for relapses in two patients and rigid relapses in two others. One of the rigid relapses occurred at 18 months of age and in the other the deformity recurred soon after a less than desirable correction in whom the surgeon chose to operate. All four feet were in the early experience group. The rate of extensive operative treatment was therefore 3% in our series. The authors think that with increasing experience this rate may be lower in patients with idiopathic clubfeet.
We identified compliance to foot abduction brace as the most important risk factor for recurrence. Other factors significantly related to relapses (Group C patients and learning curve patients) were also associated with a significantly high rate of non-compliance. This emphasizes the importance of brace compliance in preventing relapses in patients treated with the Ponseti method, as already recognized in previous studies [6, 11, 28]. Dobbs et al. also reported that the educational level of the parents was another significant risk factor for recurrence [11]. An additional risk factor identified in our study was problems with casting which interfered with serial casting. Furthermore, there was a statistically significant association of casting problems with later orthosis non-compliance suggesting that brace compliance is the key factor in preventing relapses.
We attribute the high rate of relapses in our series (31%) to the learning curve we had to go through because we had only few texts to guide us when we started the technique [7, 23, 31]. Our data clearly showed that learning curve patients had more problems with compliance and more relapses. They also required more casts and had numerous cast problems. Therefore, the authors recommend that the technique should be learned from experienced surgeons. Although it is easy to learn, casting is a motor skill to be learned and it should be done with precision. In our series, most of the problems associated with casting could have been avoided with better casting technique and also the number of casts required to correct the deformity were reduced with increasing experience.
Patients with iatrogenic deformities from previous non-Ponseti treatment were identified as a problematic group. Although, the deformities could be corrected with customized manipulations, they had significantly more casts, non-compliance, and relapses. Customized manipulations should not be regarded as modifications instead adaptations to the technique in a clubfoot with even more distorted anatomy. It is clear why these feet required more casts. However, why compliance were problematic and relapses were more frequent in this subgroup of patients remains to be elucidated.
For maintaining the correction, Ponseti emphasizes that the baby must wear a foot abduction brace [31]. The brace as described by Ponseti has been found to be very effective if it is properly constructed, the parents are accurately instructed, and the baby complies [7, 13]. However, in the bracing period, the quality and the fit of the brace and compliance can be problematic. This is reflected by a 43% rate of non-compliance in our cases.
We have evaluated brace compliance as reported by mothers. It is known that adolescents with idiopathic scoliosis tend to misreport their compliance of braces, and evaluation based on their reports are unreliable [35]. However, in this age group, the mother is the most reliable source of information and the authors had no reason to think otherwise in this situation.
We have performed tibialis anterior tendon transfers, along with Achilles tendon lengthening when necessary, in 12% of patients after second relapses had been corrected with recasting. The operation may be indicated in some other patients in the future. Ponseti reported that initially about one-third of cases required this procedure. However, it is reported to be required in considerably fewer patients (2.5%) when the importance of abduction splinting is appreciated [28].
Complete section of the Achilles tendon did not result in triceps surae weakness in any of the patients in our series and all cases were able to stand or walk on the toes at last follow-up. The authors are now confident that the tendon regenerates within weeks when the tenotomy is performed in infants, correlating with the relevant literature [7, 16]. The authors were able to Z-lengthen the previously cut and fully regenerated Achilles tendons in cases who had releases afterwards. It is also interesting to note that triceps surae weakness can be seen in patients who had open lengthening no matter how carefully it is done.
We have almost never used radiography for idiopathic clubfeet. It is known that radiographic abnormalities are common in clubfoot patients [19, 23, 29]. However, it is also reported by many authors that clinical outcome cannot be predicted from radiographs [7, 15, 19, 32]. Instead, maintenance of good movement is crucial to a successful outcome whether or not some deformity persists because movement has been shown to correlate with good functional results [12, 17, 25]. Good flexibility, as generally achieved in our cases, appears to be an important factor for future functional results.
Although imaging is not utilized during the treatment by the Ponseti method, repositioning and remodeling of cartilaginous anlages of bones, as suggested by Ponseti, has been demonstrated by serial MRI and ultrasound studies [22, 30]. Ippolito et al. reported better correction of the skeletal pathology in patients treated by the Ponseti manipulations as compared to patients treated by extensive releases [20].
The limitation of this study, as in all short-term studies, is that a mean follow-up of 46 months is too short to comment on long-term function and the appearance of the foot when the patient becomes an adult. However, most of the first relapses occurred within 24 months after casting (only two cases having relapses at 36 and 37 months) in this series. Also, Laaveg and Ponseti reported that their patients had first relapse at a mean age of 39 months [23]. Therefore, the authors thought a mean follow-up of 46 months, at a mean age of 50 months at last follow-up, would be reasonable for the purposes of evaluating the reproducibility of the technique’s effectiveness in obtaining and maintaining correction.
In conclusion, our study demonstrates that the Ponseti method is effective in all patients with idiopathic clubfeet at least up to the age of 12 months. In this age range, tendency to joint release surgery should be resisted even in late and complex deformities. Relapses do occur and they are predominantly related to non-compliance with the foot abduction orthosis. Learning the technique from an experienced surgeon will help avoid problems likely to be encountered in the early cases.
References
Aronson J, Puskarich CL (1990) Deformity and disability from treated clubfoot. J Pediatr Orthop 10:109–119
Asperheim MS, Moore C, Carroll NC, Dias L (1995) Evaluation of residual clubfoot deformities using gait analysis. J Pediatr Orthop B 4:49–54
Atar D, Lehman WB, Grant AD, Strongwater AM (1992) Revision surgery in clubfeet. Clin Orthop 283:223–230
Blakeslee TJ, DeValentine SJ (1995) Management of the resistant idiopathic clubfoot: the Kaiser experience from 1980–1990. J Foot Ankle Surg 34:167–176
Carroll NC, Gross RH (1990) Operative management of clubfoot. Orthopedics 13:1285–1296
Colburn M, Williams M (2003) Evaluation of the treatment of idiopathic clubfoot by using the Ponseti method. J Foot Ankle Surg 42:259–267 (DOI: 10.1053/S1067-2516(03)00312-0)
Cooper DM, Dietz FR (1995) Treatment of idiopathic clubfoot. A thirty-year follow-up note. J Bone Joint Surg Am 77:1477–1489
Crawford AH, Gupta AK (1996) Clubfoot controversies: complications and causes for failure. Instr Course Lect 45:339–346
Davies TC, Kiefer G, Zernicke RF (2001) Kinematics and kinetics of the hip, knee, and ankle of children with clubfoot after posteromedial release. J Pediatr Orthop 21:366–371
Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F (1995) Classification of clubfoot. J Pediatr Orthop B 4:129–136
Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA (2004) Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am 86:22–27
Green AD, Lloyd-Roberts GC (1985) The results of early posterior release in resistant clubfeet: a long-term review. J Bone Joint Surg Br 67:588–593
Hattori T, Ono Y, Kitakoji T, Iwata H (2003) Effect of the Denis Browne splint in conservative treatment of congenital club foot. J Pediatr Orthop B 12:59–62 (DOI: 10.1097/01.bpb.00000437222.21564.b5)
Heilig MR, Matern RV, Rosenzweig SD, Bennett JT (2003) Current management of idiopathic clubfoot questionnaire. A multicentric study. J Pediatr Orthop 23:780–787
Herbsthofer B, Eckardt A, Rompe JD, Kullmer K (1998) Significance of radiographic angle measurements in evaluation of congenital clubfoot. Arch Orthop Trauma Surg 117:324–329
Herzenberg JE, Radler C, Bor N (2002) Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop 22:517–521
Hutchins PM, Foster BK, Paterson DC, Cole EA (1985) Long-term results of early surgical release in clubfeet. J Bone Joint Surg Br 67:791–799
Ippolito E, Farsetti P, Caterini R, Tudisco C (2003) Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am 85:1286–1294
Ippolito E, Fraracci L, Caterini R, Di Mario M, Farsetti P (2003) A radiographic comparative study of two series of skeletally mature clubfeet treated by two different protocols. Skeletal Radiol 32:446–453 (DOI: 10.1007/s00256-003-0620-6)
Ippolito E, Fraracci L, Farsetti P, Di Mario M, Caterini R (2004) The influence of treatment on the pathology of club foot: CT study at maturity. J Bone Joint Surg Br 86:574–580 (DOI: 10.1302/0301-620X.86B4.14120)
Karol LA, Concha MC, Johnston CE II (1997) Gait analysis and muscle strength in children with surgically treated clubfeet. J Pediatr Orthop 17:790–795
Kuhns LR, Koujok K, Hall JM, Craig C (2003) Ultrasound of the navicular during the simulated Ponseti maneuver. J Pediatr Orthop 23:243–245
Laaveg SJ, Ponseti IV (1980) Long-term results of treatment of congenital club foot. J Bone Joint Surg Am 62:23–31
Lehman WB, Mohaideen A, Madan S, Scher DM, Van Bosse HJ, Iannacone M, Bazzi JS, Feldman DS (2003) A method for the early evaluation of the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B 12:133–140 (DOI: 10.1097/01.bpb.0000049579.53117.4a)
Macnicol MF, Nadeem RD, Forness M (2000) Functional results of surgical treatment in congenital talipes equinovarus (clubfoot): a comparison of outcome measurements. J Pediatr Orthop B 9:285–292
Macnicol MF (2003) The management of club foot: issues for debate. J Bone Joint Surg Br 85:167–170 (DOI: 10.1302/0301-620X.85B2.14067)
McKay DW (1983) New concept of and approach to clubfoot treatment: section II—correction of the clubfoot. J Pediatr Orthop 3:10–21
Morcuende JA, Dolan LA, Dietz FR, Ponseti IV (2004) Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics 113:376–380
Napiontek M (1996) Clinical and radiographic appearance of congenital talipes equinovarus after successful nonoperative treatment. J Pediatr Orthop 16:67–72
Pirani S, Zeznik L, Hodges D (2001) Magnetic resonance imaging study of the congenital clubfoot treated with the Ponseti method. J Pediatr Orthop 21:719–726
Ponseti IV (1996) Congenital clubfoot. Fundamentals of treatment. Oxford University Press, Oxford
Roye BD, Vitale MG, Gelijns AC, Roye DP Jr (2001) Patient-based outcomes after clubfoot surgery. J Pediatr Orthop 21:42–49
Simons GW (1985) Complete subtalar release in club feet. Part I—a preliminary report. J Bone Joint Surg Am 67:1044–1055
Sobel E, Giorgini RJ, Michel R, Cohen SI (2000) The natural history and longitudinal study of the surgically corrected clubfoot. J Foot Ankle Surg 39:305–320
Takemitsu M, Bowen JR, Rahman T, Glutting JJ, Scott CB (2004) Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine 29:2070–2074
Turco VJ (1979) Resistant congenital club foot—one-stage posteromedial release with internal fixation. A follow-up report of a fifteen-year experience. J Bone Joint Surg Am 61:805–814
Acknowledgments
The authors would like to thank Professor Rian Dişçi for his help in the statistical analysis of cases.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Göksan, S.B., Bursalı, A., Bilgili, F. et al. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Arch Orthop Trauma Surg 126, 15–21 (2006). https://doi.org/10.1007/s00402-005-0070-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-005-0070-9