Abstract
Introduction
This retrospective study presents clinical patient outcomes following meniscal repair using T-Fix devices and a modifiable, progressive rehabilitation program.
Materials and methods
Fifty-two patients (35 males and 17 females) with a mean age of 26.7 years (range 13–50 years) representing all of the patients who underwent arthroscopic meniscal repair (43 medial meniscus, 12 lateral meniscus) over a 3-year period by the same surgeon (D.C.) (55 menisci) participated in this study. Thirty-two of the patients (62%) had an associated ACL tear. All patients with an ACL tear underwent reconstruction (tibialis anterior allograft) at the time of meniscal repair. All meniscal tears were located in either the red-red zone (29) or the red-white zone (26). All patients who underwent meniscal repair participated in a modifiable (based on meniscal tear size, type, and location) progressive rehabilitation program. Operative notes and photographs were reviewed to identify the meniscal tear location, tear type, tear length, and the number of T-Fix devices used. Orthopedic clinic and physical therapy reports were also reviewed for postoperative range of motion, knee joint effusion, knee joint pain, McMurray test findings, and single-leg broad-jump test performance (90% bilateral equivalence goal). The average postoperative clinical follow-up period was 10.3 months (range 4–24 months).
Results
Most (22/23, 96%) patients who underwent meniscal repair alone displayed excellent results. All patients (32/32, 100%) who underwent combined ACL reconstruction-meniscal repair displayed excellent results. During an acute event such as a sudden directional change while running or contact with another player, 5 of these patients re-injured their meniscus at the repair site in conjunction with tearing the reconstructed ACL at 12±3 months following the index surgical procedure. Each of these 1–2 cm meniscal tears had been previously repaired with two T-Fix devices.
Conclusion
The T-Fix device used in combination with a modifiable progressive rehabilitation program produced excellent clinical patient outcomes among this patient group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
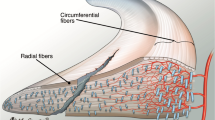
Nonimpaired meniscus function is essential to distribute knee joint reaction forces during weight-bearing, absorb impact shock, serve as a secondary source of noncontractile joint stabilization, provide nutrition to articular cartilage, and facilitate joint gliding and lubrication [11, 37, 43]. In a MRI study of 21 symptom-free adolescent soccer players, Wacker et al. [42] reported increased signals in the central medial meniscus among 38% of soccer players compared with 17% of control subjects. Additionally, the medial femoral condyle hyaline cartilage was on average 24.8% thicker for the young soccer players compared with control subjects. These findings support the sensitive balance between meniscal tissue functionality and femoral hyaline cartilage integrity.
Meniscal resection can contribute to the development of osteoarthritic changes at the knee joint [22]. To conserve this valuable tissue, meniscal repair rather than resection has become the preferred surgical management method whenever possible. Henning popularized arthroscopic meniscal repair [23]. Arthroscopic intervention for meniscal injury may include ‘inside-out’ [34, 35, 38, 39], ‘outside-in’ [28, 29, 44], and ‘all-inside’ [28] repair techniques. The posterior incision used during ‘inside-out’ meniscal repair techniques may contribute to neurovascular complications [9, 16]. Ultimately, meniscal repair success or failure can be influenced by various factors including knee joint capsuloligamentous status, location and type of meniscal tear, method of fixation, surgical timing, type of suture used, repair technique, and postoperative rehabilitation progression [5, 7, 15, 17, 21, 25, 40]. Presently, there is a lack of consensus regarding recommended postoperative rehabilitation progression and timetables following meniscal repair.
We observed a high percentage of knee joint capsule injury among our patients who had sustained anteroposterior longitudinal meniscal tears. Conceptually, anteroposterior longitudinal meniscal tears should be effectively repaired using a device such as the T-Fix (Smith Nephew Endoscopy, Andover, MA, USA) [2, 18, 19]. Barrett et al. reported that ‘all-inside’ meniscal repair using the T-Fix device enabled relatively easy device placement, did not require a posterior incision, and reduced complications associated with surgically induced neurovascular injury [9]. The purpose of this retrospective study is to discuss our clinical patient outcomes following meniscal repair using the T-Fix device in combination with a modifiable, progressive rehabilitation program based on meniscal injury size, type, and location.
Patients and methods
All of the patients who underwent arthroscopic meniscal repair over a 3-year period by the same surgeon (D.C.) using the T-Fix device were retrospectively evaluated via a comprehensive clinical examination. Fifty-two patients (55 menisci) who underwent T-Fix meniscal repair were identified. There were 35 males and 17 females with an average age of 26.7 years (range 13–50 years) in the study group. The average postoperative clinical follow-up period was 10.3 months (range 4–24 months). The operative notes and photographs taken during the index surgical procedure were reviewed to identify the meniscal tear location, tear type, tear length, and the number of T-Fix devices used. Orthopedic clinic and physical therapy reports were also reviewed for postoperative range of motion, knee joint effusion, knee joint pain, McMurray test findings, and single-leg broad-jump capability. A successful patient outcome was classified as an absence of knee pain and effusion, full active knee joint range of motion, a negative McMurray test, and 90% bilateral equivalence on a single-leg broad-jump. Additionally, all patients participated in a progressive rehabilitation program based on meniscal lesion size and type. If the anteroposterior longitudinal meniscal tear was <3 cm in length, knee flexion was restricted to 0–90° for 3 weeks and restricted to 0–125° flexion between postoperative weeks 3 and 6. If the meniscal tear was >3 cm in length. the knee was immobilized at 0° flexion with a locked long-leg hinged knee brace during full weight-bearing. Passive motion from 0 to 90° knee flexion in a continuous passive motion (CPM) device was encouraged over the initial 3 postoperative weeks. Between postoperative weeks 3 and 6, active knee flexion between 0 and 90° was allowed, and 0–125° passive knee flexion was allowed in the CPM device. Between 6 and 8 weeks following surgery, 0–125° active knee range-of-motion restrictions were terminated. All patients with anteroposterior longitudinal meniscal tears were allowed to return to sports that required regular cutting and jumping tasks by the 12th postoperative week. Patients who underwent repair of a complex or radial meniscal tear followed similar rehabilitation progressions, but with slightly greater delays in range of motion and weight-bearing progression (Table 1). As weight-bearing increased, all subjects participated in a progressive rehabilitation exercise regimen that emphasized weight-bearing, multiplanar, lower extremity function integrated with lumbopelvic control [31, 41]. By 6 weeks following surgery, all patients were allowed full weight-bearing as tolerated in the surgically treated lower extremity during gait.
Results
Of the 55 meniscal tears identified, 43 were medial meniscal tears, and 12 were lateral meniscal tears. All tears were classified as anteroposterior longitudinal meniscal tears, primarily at the posterior meniscal horn. All meniscal tears were located in either the red-red zone (29/55) or the red-white zone (26/55). Four of the tears were classified as bucket-handle tears. The majority of patients (32/55, 62%) had an associated ACL lesion that occurred concurrently with the meniscal injury. All patients who sustained an ACL lesion underwent reconstruction (tibialis anterior allograft) at the time of meniscal repair. The majority of meniscal tears were 1–2 cm in length (44/55, 80%) and were repaired using two T-Fix devices. Meniscal tears of 2–3 cm in length (9/55, 16.4%) were repaired using four T-Fix devices. Meniscal tears of 3–4 cm in length (2/55, 3.6%) were repaired using six T-Fix devices. All T-Fix devices were secured in pairs using a horizontal mattress suture configuration, and there were no intraoperative complications associated with T-Fix device insertion.
The majority (22/23, 96%) of patients who underwent meniscal repair alone displayed excellent results. A 50-year-old man, who underwent repair of a red-red zone posterior horn longitudinal tear of the medial meniscus using two T-Fix devices experienced continued knee pain and effusion at 6 months following the initial surgery. This patient had initiated aggressive active knee flexion range of motion earlier than recommended by our rehabilitation program. At 20 months following the index surgical procedure, a 22-year-old man experienced re-injury of a red-red zone, bucket-handle lateral meniscus tear from a sudden pivoting mechanism. The meniscal tear had been previously repaired using six T-Fix devices. Both of these patients were treated with arthroscopic meniscal resection at the site of the unhealed meniscus that was previously repaired.
All of the patients (32/32, 100%) who underwent combined ACL reconstruction-meniscal repair displayed excellent results. During a later acute event such as a sudden directional change while running or contact with another player, 5 of these patients re-injured their meniscus at the repair site in conjunction with tearing the reconstructed ACL at 12±3 months following the index surgical procedure. Each of these 1–2 cm meniscal tears had been repaired with two T-Fix devices. Patients who experienced a re-injury underwent revision ACL reconstruction and arthroscopic meniscal debridement.
Discussion
Proponents of both open and arthroscopic meniscal repair techniques have cited advantages related to technical ease, avoidance of complications, and overall efficacy compared with the alternative technique. Arthroscopic ‘inside-out’ techniques provide strong fixation, but their use is associated with a higher frequency of complications such as nerve injury [lateral peroneal (1%), medial-saphenous (7%); sterile effusion (2%), superficial infection (1%), and deep infection (1%)] [4]. Increased incidence of deep vein thrombosis, popliteal artery laceration, arthrofibrosis, and reflex sympathetic dystrophy has also been reported [24]. To avoid the complications associated with ‘inside-out’ meniscal repair techniques, the ‘outside-in’ and ‘all-inside’ techniques have been developed. Biomechanical studies have reported that the fixation strength using T-Fix devices is superior to that provided by almost all other methods of ‘all-inside’ meniscal repair [3, 10], and T-Fix implantation is markedly easier to perform than any ‘inside-out’ technique [9, 18]. Using a dog model, Arnoczky et al. [1] reported that meniscal healing is almost completed by 10 weeks following repair. Asik et al. [2] reported that complete meniscal healing takes approximately 12 weeks to occur. Based on these reports, patients who had been operated on less than 16 weeks previously were excluded from this study.
Although several reports have cited meniscal repair success rates approaching 90% using the T-Fix device [2, 8, 9], complications including synovitis and chondral lesions have been reported [9, 10]. Our experience suggests that appropriate T-Fix device use provides greater meniscal fixation and fewer complications than conventional ‘all-inside’ techniques. Second-look arthroscopic examination of our 2 patients who sustained either meniscal repair failure at 6 months after surgery or re-injury at 20 months following surgery revealed injury solely at the site of the previous meniscal lesion without evidence of synovitis or chondral lesions. Second-look arthroscopic examination of the 5 patients who sustained re-injury following meniscal repair in conjunction with ACL reconstruction likewise displayed meniscal re-injury solely at the site of previous repair, without evidence of degenerative meniscal changes, synovitis, or chondral lesions.
The chemotactic factor and growth hormone proliferation associated with the knee joint hemarthrosis that occurs from both the initial ACL injury and the ensuing reconstruction along with accumulated bony debris from tunnel creation and notchplasty are believed to facilitate meniscal healing [6]. Some surgeons believe that the meniscal healing rate is increased when repair is performed in conjunction with ACL reconstruction [6, 19, 28, 40]. Our results agree that these factors should enhance meniscal healing. However, our patients who sustained meniscal re-injury in combination with ACL graft injury displayed meniscal re-injury at the exact site of previous repair. This suggests that combined meniscal healing and T-Fix fixation were insufficient to protect the meniscus in the presence of ACL graft failure.
Several reports suggest the efficacy of immobilizing the knee in full extension early during rehabilitation [12, 29, 30]. However, others have recommended knee joint immobilization at variable flexion angles [19, 20, 34, 35, 38]. Several reports have suggested the need to restrict either early active or passive range of motion following meniscal repair [13, 14, 25, 40]. While several reports have recommended non-weight-bearing early during gait following meniscal repair [14, 34, 35, 38], early partial weight-bearing [13, 19, 20, 25, 40] and immediate full weight-bearing [28, 29] have also been proposed. Several reports have also suggested returning to cutting-type athletic maneuvers by 4 months post-meniscal repair [26, 28, 29].
Asik et al. [2] reported excellent (32/47, 68%), good (10/47, 21%), fair (2/47, 4%), and poor (3/47, 6%) clinical results using the T-Fix device and an aggressive rehabilitation program using immediate partial weight-bearing with the knee immobilized in full extension by a locking hinge knee brace over the initial 2 postoperative weeks. At 2 weeks following surgery 0–90° of active knee flexion was allowed, and after 6 weeks full active knee flexion was allowed. Full weight-bearing during gait was allowed 8 weeks following surgery [2]. On second-look arthroscopy at 6 months following the index surgical procedure, Asik et al. reported that all 6 patients who underwent meniscal repair in conjunction with ACL reconstruction displayed complete meniscal healing [2]. Barber [5] reported similar meniscal repair success rates among patients who participated in an accelerated rehabilitation program (full weight-bearing as tolerated during ambulation, unrestricted active knee flexion, and return to sports with a de-rotational brace at 3–4 months post-surgery) compared to patients who participated in a conventional rehabilitation progression (knee immobilization in brace locked at slight flexion for 6 weeks, non-weight-bearing for 12 weeks, and return to full sports participation at 6 months) post-meniscal repair. Mariani et al. [27] reported 77.3% (17/22 patients) good clinical results among patients who underwent meniscal repair and postoperative rehabilitation that included 0–90° passive knee flexion and full weight-bearing for 2 weeks. Over the initial 4 postoperative weeks, the surgical knee was immobilized at 0° flexion in a locked knee brace during ambulation. Brace use was discontinued when the patient achieved good quadriceps femoris muscle function and pain-free ambulation [27]. Progressive resistance exercises were initiated at 4 weeks post-meniscal repair. Noyes et al. [32] reported that accelerated rehabilitation among patients who underwent meniscal repair combined with ACL reconstruction might prevent knee joint arthrofibrosis. They suggested that immediate knee joint motion helped decrease the risk of knee joint contracture, stiffness, articular cartilage deterioration, and disuse-induced knee joint arthrosis. They also reported no statistically significant differences in hemarthrosis and soft-tissue swelling between immediate (accelerated rehabilitation program) and restricted (traditional rehabilitation program) knee joint motion. Tenuta and Arciero [40] reported similar satisfactory clinical results (85% success rates) using two different rehabilitation programs (conservative vs aggressive). The conservative rehabilitation progression included toe-touch weight-bearing, restricted knee range of motion (20–60°) over the initial 6 postoperative weeks followed by a 10–90° knee flexion allowance and partial weight-bearing using a single crutch between postoperative weeks 6 and 8, and full weight-bearing and unrestricted knee range of motion beginning during the 8th postoperative week. The aggressive rehabilitation program included early full range of motion and full weight-bearing. Although second-look arthroscopy revealed superior healing results among the patients who participated in the conservative rehabilitation program, the authors did not report which program patients with larger 3–4 cm tears who sustained repair failures had followed. Perhaps if these patients had modified their rehabilitation weight-bearing and range-of-motion progression, they would not have experienced repair failures.
Noyes and Barber-Westin [33] reported their results using a postoperative meniscal repair rehabilitation program that allowed early active knee flexion and full weight-bearing and return to cutting sports 6 months following surgery. Active knee flexion was restricted to 90° over the initial 3 weeks following surgery, restricted to 120° at 3–4 weeks post-surgery, with 135° allowed at 5–6 weeks post-surgery. Only partial weight-bearing was allowed over the initial 4 postoperative weeks. Following repair of horizontal, radial, or complex multiplanar meniscal tears, Noyes and Barber-Westin [33] recommended partial weight-bearing for 6 weeks. They reported good results (87%) for avascular zone meniscal tear repairs among patients who were 40 years of age or older. In our literature search, only Noyes and Barber-Westin [33] suggested the need to modify the use of accelerated rehabilitation programs depending upon the type of meniscal tear and suture technique used. Shelbourne et al. [36] suggested that all patients with unstable, peripheral, longitudinal, isolated meniscal tears could successfully participate in an accelerated postoperative rehabilitation program. Our rehabilitation program attempted to combine the progressiveness reported by Shelbourne et al. [36] with the case-by-case modifications based on the meniscal tear type and size as recommended by Noyes and Barber-Westin [33]. Additionally, we recommend consideration of the suture material that is used and the surgeon’s experience. Because of the fragile nature of bioabsorbable suture material, we believe that progressive rehabilitation following meniscal repair is more efficacious when non-bioabsorbable suture material is used.
All of the patients in this series participated in a progressive rehabilitation program that focused on early full weight-bearing, progressive active and passive knee range of motion, and eventual return to full sports participation. Based upon our clinical examination results, we agree with Barber and Click [6] that early physiological loading in conjunction with secure repair site fixation promotes meniscal healing while likely improving the functionality of the repaired tissue. However, depending upon the length and type of meniscal tear, the suture material used, the experience of the surgeon, and the type of fixation device used, we recommend rehabilitation program modification to provide additional repair site protection for larger anteroposterior longitudinal, radial, and complex meniscal tears (Table 1).
For anteroposterior longitudinal meniscal tears, weight-bearing actually helps stabilize the anteroposterior longitudinal meniscal tear repair site, but early aggressive active knee flexion with the larger tears (>3 cm) may tend to compromise the repair site, particularly if the tear is located in the posterior meniscal horn region. For our patients who present with a radial meniscal tear, we recommend non-weight-bearing for 6 weeks, partial weight-bearing with single crutch use, and full unrestricted knee range of motion at 8 weeks post-surgery, and return to full sports activity at 4–5 months. With these patients, immediate full weight-bearing may tend to displace the tear edges, thereby compromising the repair. Following surgical repair of complex meniscal tears, concern arises over the integrity of the suture fixation. Therefore, the time period for partial weight-bearing and restricted active range of motion are prolonged to protect the repair site during the early stages of the progressive rehabilitation program.
Although combined ACL reconstruction and meniscal repair surgery may enhance the meniscal healing process [6, 30], we have found that even at 12±3 months following the index combined surgical procedures, acute failure of the ACL graft will likely be associated with re-injury to the meniscus at the site of previous repair. We found this to be true even among smaller (1–2 cm), red-red zone tears that had been repaired using two T-Fix devices.
References
Arnoczky SP, Warren RF (1983) The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med 11:131–141
Asik M, Sen C, Erginsu M (2002) Arthroscopic meniscal repair using T-fix. Knee Surg Sports Traumatol Arthrosc 10:284–288
Asik M, Sener N (2002) Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc 10:25–29
Austin KS, Sherman OH (1993) Complications of arthroscopic meniscal repair. Am J Sports Med 21:864–868
Barber FA (1994) Accelerated rehabilitation for meniscus repairs. Arthroscopy 10:206–210
Barber FA, Click SD (1997) Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy 13:433–437
Barber FA, Herbert MA (2000) Meniscal repair devices. Arthroscopy 16:613–618
Barber FA, Herbert MA (1999) Suture anchors--update 1999. Arthroscopy 15:719–725
Barrett GR, Treacy SH, Ruff CG (1997) Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy 13:218–223
Becker R, Schroder M, Starke C, Urbach D, Nebelung W (2001) Biomechanical investigations of different meniscal repair implants in comparison with horizontal sutures on human meniscus. Arthroscopy 17:439–444
Bessette GC (1992) The meniscus. Orthopedics 15:35–42
Busenkell GL, Lee CS (1992) Arthroscopic meniscal repair: a posterior cannulated technique. Arthroscopy 8:247–253
Buseck MS, Noyes FR (1991) Arthroscopic evaluation of meniscal repairs after anterior cruciate ligament reconstruction and immediate motion. Am J Sports Med 19:489–494
Cannon WD Jr, Vittori JM (1992) The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 20:176–181
Cassidy RE, Shaffer AJ (1981) Repair of peripheral meniscus tears. A preliminary report. Am J Sports Med 9:209–214
Cetinkaya SM, Boynuk B, Taser O (1997) The comparison of the failure strength of meniscus arrows (absorbable fixation material) with different meniscal suturing techniques. Acta Orthop Traumatol Turc 31:453–455
Clark CR, Ogden JA (1983) Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am 65:538–547
Coen MJ, Caborn DN, Urban W, Nyland J, Johnson DL (1999) An anatomic evaluation of T-Fix suture device placement for arthroscopic all-inside meniscal repair. Arthroscopy 15:275–280
DeHaven KE, Black KP, Griffiths HJ (1989) Open meniscus repair. Technique and two to nine year results. Am J Sports Med 17:788–795
DeHaven KE, Lohrer WA, Lovelock JE (1995) Long-term results of open meniscal repair. Am J Sports Med 23:524–530
Doral MN Leblebicioglu G, Atay A (1999) Treatment of meniscal injuries in the anterior cruciate ligament injured knees. Acta Orthop Traumatol Turc 33:426–429
Fairbank TJ (1948) Knee joint changes after menisectomy. J Bone Joint Surg Br 30:664–670
Henning CE (1983) Arthroscopic repair of meniscus tears. Orthopedics 6:1130–1132
Henning CE, Clark JR, Lynch MA, Stallbaumer R, Yearout KM, Vequist SW (1988) Arthroscopic meniscus repair with a posterior incision. Instr Course Lect 37:209–223
Henning CE, Lynch MA, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA (1990) Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop 252:64–72
Jakob RP, Staubli HU, Zuber K, Esser M (1988) The arthroscopic meniscal repair. Techniques and clinical experience. Am J Sports Med 16:137–142
Mariani PP, Santori N, Adriani E, Mastantuono M (1996) Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy 12:680–686
Morgan CD (1991) The ‘all-inside’ meniscus repair. Arthroscopy 7:120–125
Morgan CD, Casscells SW (1986) Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy 2:3–12
Morgan CD, Wojtys EM, Casscells CD, Casscells SW (1991) Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 19:632–637
Murray R, Bohannon R, Tiberio D, Dewberry M, Zannotti C (2002) Pelvifemoral rhythm during unilateral hip flexion in standing. Clin Biomech 17:147–151
Noyes FR, Mangine RE, Barber S (1987) Early knee motion after open and arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med 15:149–160
Noyes FR, Barber-Westin SD (2000) Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy 16:822–829
Rosenberg TD, Scott SM, Coward DB, Dunbar WH, Ewing JW, Johnson CL, Paulos LE (1986) Arthroscopic meniscal repair evaluated with repeat arthroscopy. Arthroscopy 2:14–20
Ryu RK, Dunbar WH (1988) Arthroscopic meniscal repair with two-year follow-up: a clinical review. Arthroscopy 4:168–173
Shelbourne KD, Patel DV, Adsit WS, Porter DA (1996) Rehabilitation after meniscal repair. Clin Sports Med 15:595–612
Stone RG, Frewin PR, Gonzales S (1990) Long-term assessment of arthroscopic meniscus repair: a two- to six-year follow-up study. Arthroscopy 6:73–78
Stone RG, Miller GA (1985) A technique of arthroscopic suture of torn menisci. Arthroscopy 1:226–232
Stone RG, VanWinkle GN (1986) Arthroscopic review of meniscal repair: assessment of healing parameters. Arthroscopy 2:77–81
Tenuta JJ, Arciero RA (1994) Arthroscopic evaluation of meniscal repairs. Factors that effect healing. Am J Sports Med 22:797–802
Tiberio D (1994) Functional rehab in ankle injuries. Rehab Management: Interdisciplinary J Rehab 7:31–33, 131–132
Wacker F, Konig H, Felsenberg D, Wolf KJ (1994) MRT of the knee joint of juvenile footballers – are there early changes in the knee due to competitive sport? Fortschritte Geb Rontgenstr Neuen Bildgebenden Verfahren 160:149–153
Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192
Warren RF (1985) Arthroscopic meniscus repair. Arthroscopy 1:170–172
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kocabey, Y., Nyland, J., Isbell, W.M. et al. Patient outcomes following T-Fix meniscal repair and a modifiable, progressive rehabilitation program, a retrospective study. Arch Orthop Trauma Surg 124, 592–596 (2004). https://doi.org/10.1007/s00402-004-0649-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-004-0649-6