Abstract
In brains of patients with Alzheimer’s disease (AD), Aβ peptides accumulate in parenchyma and, almost invariably, also in the vascular walls. Although Aβ aggregation is, by definition, present in AD, its impact is only incompletely understood. It occurs in a stereotypical spatiotemporal distribution within neuronal networks in the course of the disease. This suggests a role for synaptic connections in propagating Aβ pathology, and possibly of axonal transport in an antero- or retrograde way—although, there is also evidence for passive, extracellular diffusion. Striking, in AD, is the conjunction of tau and Aβ pathology. Tau pathology in the cell body of neurons precedes Aβ deposition in their synaptic endings in several circuits such as the entorhino-dentate, cortico-striatal or subiculo-mammillary connections. However, genetic evidence suggests that Aβ accumulation is the first step in AD pathogenesis. To model the complexity and consequences of Aβ aggregation in vivo, various transgenic (tg) rodents have been generated. In rodents tg for the human Aβ precursor protein, focal injections of preformed Aβ aggregates can induce Aβ deposits in the vicinity of the injection site, and over time in more distant regions of the brain. This suggests that Aβ shares with α-synuclein, tau and other proteins the property to misfold and aggregate homotypic molecules. We propose to group those proteins under the term “propagons”. Propagons may lack the infectivity of prions. We review findings from neuropathological examinations of human brains in different stages of AD and from studies in rodent models of Aβ aggregation and discuss putative mechanisms underlying the initiation and spread of Aβ pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracellular Aβ deposits and intracellular tau aggregates are required to make the definite neuropathological diagnosis of Alzheimer disease (AD) [60]. Attempts to develop new therapeutic strategies have fostered intense investigations to understand their formation and their consequences. Research has benefited from the neuropathological examinations of AD brains as well as from the use of rodent models exhibiting age-related Aβ deposition due to transgenic (tg) overexpression of human Aβ peptides. Some of the questions raised by human neuropathology have found answers in the controlled genetic environment of tg animals. Possible prion-like mechanisms involved in Aβ aggregation have recently been extensively studied in the rodent model and are the focus of this review.
Is prion-like aggregation the key to understanding AD? Which ‘prion-like’ aspects apply to Aβ aggregation in humans? What are the properties of the Aβ seeds? What exactly would propagate within neuronal networks and how? Those are some of the questions that are considered here. In attempting to answer them, the “prion-like” qualifier, currently applied to different pathological processes, often appeared inadequate or ambiguous. We propose to adopt the term “propagon” for all misfolded, multimeric proteins that can catalyze the misfolding and aggregation of homotypic proteins and lead to the spread of pathological protein misfolding. A more detailed definition of the term and the different levels of this process can be found below. The term “propagon” was initially coined to describe propagation of the misfolded form of the yeast Sup35p protein [24].
We focus on Aβ pathology, since tau pathology is discussed in another chapter of this review cluster [79]. However, Aβ and tau pathology in AD are interrelated and tau pathology will also be considered where necessary.
AD and Aβ
Plaques and tangles vs. Aβ and tau pathology in the human brain
AD pathology was initially characterized by the presence of senile plaques and neurofibrillary tangles, two lesions that were identified by silver techniques. The discovery that the core of the senile plaque consists of accumulated Aβ peptides (Aβ), whereas hyperphosphorylated tau proteins aggregate to form neurofibrillary tangles, greatly advanced the understanding of AD. Immunohistochemistry (IHC), with sensitive tau and Aβ antibodies, reveals a picture of pathology that appears very different from the one obtained with silver staining methods. Unfortunately, this major improvement has not been accompanied by a change in vocabulary to account for the subtypes of deposits recognized by IHC [31]. The term senile plaque has thus become ambiguous since it is used indiscriminately to designate diffuse Aβ deposits that are large, convoluted and devoid of any neuritic component, as well as focal deposits that are spherical and dense, sometimes Congo red positive, and also the mature senile plaque composed of a center of Aβ in an amyloid conformation and of a crown of tau-positive neurites (Fig. 1)—a complex lesion also involving astrocytes and microglia. Aβ deposition can also occur in vessel walls (cerebral amyloid angiopathy: CAA) and is typically dense and Congo red positive.
Human brain. Diffuse Aβ deposits free from tau-positive neurites. Focal deposit with a corona of degenerating neurites (senile plaque). a, b Diffuse Aβ deposit in the putamen with a low density of tau-positive neurites. The same fields have been located in digitized pictures of two adjacent sections (with the use of a Hamamatsu slide scanner). The plus signs indicate the same two vessels, and the asterisk sign indicates the same two contiguous neurons. a Tau (AT8) immunohistochemistry b Aβ (6F3D) immunohistochemistry. A few threads or dots (arrows) are identified after tau immunohistochemistry, but the Aβ deposits are devoid of a neuritic component. Scale bar 100 µm. c, d Tau and Aβ double labeling in the neocortex. AT8 antibody against hyperphosphorylated tau staining with secondary antibody coupled to alkaline phosphatase using true red as chromogen. 6F3D antibody against Aβ with the secondary antibody coupled to peroxidase using diaminobenzidine as chromogen. c Illustrates a diffuse deposit (brown) containing only rare tau-positive dots (white arrow): neurites (red) are visible (black arrows) in the surrounding neuropil. In d, on the contrary, the deposit has a focal core (large arrow), more dense than the rest of the deposit. Several degenerating neurites (smaller arrows) are visible in the corona of the deposits. A (mature) senile plaque is made of a focal Aβ deposit and a corona of degenerating neurites. Scale bar 50 µm
The visible pool of Aβ detectable by microscopy corresponds to deposits that are relatively abundant and readily detected by IHC or other staining methods. It does not include the various small and soluble species of the peptide [85] that could play an essential role in the pathogenesis. Obtaining a better understanding of Aβ pathology is complicated by the fact that the production and clearance of Aβ peptides, as well as the aggregation process, are highly complex and insufficiently understood.
Origin of Aβ peptides
Aβ peptides of various length are derived by two consecutive proteolytic cleavages of the Aβ precursor protein (APP, also termed amyloid precursor protein). The β-site APP cleaving enzyme 1 (BACE1) cleaves APP in its extracellular region, giving rise to a secreted fragment (APPsβ) and to the transmembrane fragment C99 (or CTFβ). C99 is subsequently cleaved by a γ-secretase complex, in which presenilin is the catalytic subunit. The cleavage releases soluble Aβ peptides [118, 122]. Alternatively, APP is cleaved by α-secretase within the Aβ sequence, and then by γ-secretase. In this pathway, generation of Aβ peptides is prevented. It was recently discovered that APP processing is even more complex. η-Secretase processing generates longer APP-C-terminal fragments that are further processed to long and short Aη fragments by α- or β-secretases (Aη-α, Aη-β). These fragments can specifically lower neuronal activity and long-term potentiation [130].
The physiological role of APP processing and of the various fragments that are generated is currently unclear [5]. Aβ peptides are constitutively produced in soluble forms, with a short half-life in the brain: 8 % of the total amount of Aβ present in the central nervous system is synthesized and cleared every hour [3]. In the mouse, half-life of Aβ in the interstitial fluid is 2 h [22]. Generation of Aβ peptides is not the main pathway of APP processing, but it is the aggregation of Aβ peptides that is the hallmark of AD.
Is there a toxic form of Aβ?
Native Aβ peptides are presumably unfolded, but intrinsically aggregation prone, especially the longer forms (e.g., Aβ42 compared to Aβ40). In vitro and in vivo Aβ peptides can form dimers, trimers, higher order oligomers, protofibrils, as well as amyloid fibrils [126]. The pathogenic role of soluble, misfolded Aβ species and of insoluble Aβ fibrils is unknown. Great emphasis has been put on the putative toxicity of soluble oligomers [127] and on the innocuity of insoluble fibrils, for example in the J20 tg line [19]. Soluble aggregates, however, diffuse rapidly through the brain and quickly become widespread [38]. If such soluble Aβ aggregates were directly toxic, the cortical symptoms should be generalized rapidly, producing a global cortical dysfunction, in contrast to the progressive worsening of the symptoms that is observed clinically in AD. The involvement of a third species—diffusible, but neither soluble nor fibrillar—has also been advocated [121].
The opposite view, i.e., that the fibrillization of Aβ is important for toxicity has also been expressed [80]. In humans [120] as in animals (for example, in APParc tg mice [104]), phases of progression of amyloid deposits have been described: localized deposits, made of insoluble (possibly misfolded) Aβ, affect an ever-increasing number of regions of the brain. The aggregation propensity of Aβ peptides may influence the distribution of the deposits: Aβ40, being less aggregation prone than Aβ42, may reach the vessels whereas Aβ42 more readily aggregates in the parenchyma [53, 54]. The observed stepwise progression of AD symptoms is more in accordance with the stepwise progression of localized deposits of insoluble Aβ than with the widespread distribution of soluble oligomers. In humans, fibrillar deposits are often surrounded by tau-positive degenerating neurites that could also play an important role in the pathogenesis and in the neurological deficits that cause the clinical symptoms. Interestingly, it is well known from neuropathology [28, 29] and brain imaging with Aβ ligands [63] that individuals can have significant Aβ pathology without cognitive impairment [123]. It is, therefore, important to carefully dissect and analyze the process of Aβ aggregation and the various aggregate species that form, to decipher the mechanisms of toxicity.
Misfolding and aggregation of proteins
Why and how soluble peptides, such as Aβ, aggregate and become insoluble is only partially known. A native protein is soluble because it is naturally unfolded or because it has been correctly folded, possibly with the help of chaperone proteins [114]. The native, normal protein generally includes α-helical and unordered structures. A misfolded, amyloidogenic protein is enriched in β-sheets. The transition from α-helix or unordered structure to β-sheets is associated with the exposure of hydrophobic amino-acid residues, promoting protein aggregation. As a consequence, a normally soluble protein may become insoluble and form aggregates without any change in its amino-acid sequence [36, 114]. Misfolded proteins can be refolded into their native conformation or degraded by specific cellular pathways. Some amyloidogenic proteins escape degradation or refolding, especially when aggregated, and accumulate. These misfolded or aggregated proteins, participating in aberrant interactions with other macromolecules or with cellular components, may be the toxic species.
Aβ aggregation
In humans
Aβ aggregation in the human brain is age dependent and occurs on the time scale of decades [62, 63, 95]. The cause of Aβ aggregation is unknown, except in the rare familial AD cases (FAD) in which the production of Aβ peptides and/or the ratio of Aβ42/Aβ40 peptides is increased. Mutations found in FAD are highly penetrant and involve either APP or presenilin 1 or 2 genes [6]. Examples of APP mutations are the “London” mutation (APP V717I) that increases the Aβ42/Aβ40 ratio by modifying the γ-secretase cleavage of APP, or the “Swedish” mutation (APP KM670/671NL) enhancing β-cleavage. Mutations in the Aβ sequence itself can also favor aggregation as observed in the “Arctic” mutation (APP E693G). Triplication of the APP gene located on chromosome 21 as in Down’s syndrome (Trisomy 21) [131], or in rare familial cases of AD with duplication of the APP gene [105] also lead to AD pathology [82]. A role for polymorphisms in the promoter region of the APP gene has been discussed [56]. The presenilins are the catalytic subunits of the γ-secretase complex and FAD-associated mutations typically promote an increase in longer and more amyloidogenic Aβ peptides [18, 108].
Sporadic AD cases are considered multifactorial [6, 17]. Deficient Aβ clearance that could decrease the ability of a cell to get rid of misfolded proteins, and altered proteostasis are advocated and appear linked to aging [96]. In both familial and sporadic cases, an increased concentration of aggregation-prone Aβ is thus presumed to occur [73]. In vitro, the solubility of Aβ42 is around 10 µM. Above this value, and in a concentration-dependent manner, a slow nucleation process may take place, followed by relatively fast elongation [64, 65]. Aggregated Aβ may then play the role of nuclei and induce seeded propagation of misfolding. Aβ aggregation appears to be necessary to trigger AD, although it may not be sufficient. A complex pathogenic cascade downstream of AD likely mediates neurodegeneration [92].
In animal models
There is no natural animal model for AD. Very old apes, monkeys, and some other mammals like bears, dogs and cats may have diffuse Aβ deposits and minor CAA, but not full AD pathology or neurodegeneration [26, 55, 97, 112] Thus, tg mice and rats have become invaluable to study Aβ aggregation in vivo. Murine Aβ differs from the human homologue by three amino acids and is less aggregation prone. Spontaneous Aβ deposition has not been observed in this species within its lifetime of 2–3 years [2]. However, progressive Aβ aggregation is observed in mice and rats that express human APP with FAD-associated mutations [16, 20, 107], or human Aβ [84], by tg or knock-in strategies.
To achieve Aβ aggregation, FAD-associated APP mutations such as the “London”, “Swedish”, or “Arctic” mutation (see above) are often used. The age of onset of Aβ deposition in these single human APP transgenics inversely correlates with the level of APP overexpression (the higher the APP level the earlier the onset), and is also affected by the APP sequence expressed (the more total Aβ and the more aggregation-prone Aβ peptides are generated, the earlier the onset of deposition).
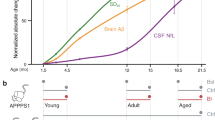
Typical examples with high levels of APP overexpression (five- to sevenfold over endogenous, murine APP) related to the APP Swedish mutation (APPSwe) are the widely used APP23 and Tg2576 tg mice with onset of Aβ deposition in mid-adulthood (7–11 months of age) [57, 117]. Onset in late adulthood (15–18 months of age) is often observed in tg strains with moderate APP overexpression (two- to threefold over endogenous), e.g., in R1.40 mice, also harboring the APPSwe mutation [75]. When only low levels of tg APP overexpression are achieved and/or wild-type APP is overexpressed, no amyloid pathology is observed within the normal lifespan of the mice [90] (Fig. 2).
Aβ pathology in APP transgenic (tg) rodents and the principle of ‘molecular propagons’. a Rodents tg for human APP spontaneously develop Aβ pathology in the brain depending on the level of APP overexpression (the higher the level, the earlier the occurrence) and the generation of amyloidogenic Aβ variants (the more amyloidogenic Aβ, the earlier the occurrence). Aβ pathology can be observed by IHC as early as a few weeks of age in some APP transgenics (dark red line), while other lines develop pathology later (red and orange lines), or do not develop any pathology within their life span (blue line). Non-tg rodents do not develop Aβ pathology within their life span (dashed black line). b Intracerebral injection of young, predepositing APP tg rodents with preformed Aβ aggregates (seeding) leads to earlier onset of Aβ pathology, typically by many months (dashed red line vs. solid red line). Seeding induces Aβ pathology also in rodents tg for human APP, that would normally not develop Aβ pathology within their life span (dashed blue line vs. solid blue line). Since murine and human Aβ differ in their aggregation propensity, seeding does not induce Aβ aggregation in non-tg rodents (not shown). c Molecular Aβ propagons. Native Aβ peptides can spontaneously misfold and assemble into various types of aggregates. Aβ seeds seem to catalyze the misfolding of native Aβ peptides by templated misfolding, presumably by assisting unfolding, misfolding and incorporation into the growing aggregate. Different types of Aβ aggregates, shown as strain A and strain B, were shown to propagate their specific conformation to the newly incorporated Aβ peptides in vitro and in vivo. Fragmentation (not shown) can generate more seeds. This leads to a cascade of progressive Aβ aggregation and spreading of pathology
Amyloid deposition in APP tg rodents is typically accelerated by coexpression of FAD-associated mutant human presenilin 1 or 2 (PS1 or PS2) by tg or knock-in strategies that modify the γ-secretase cleavage, and thus, promote generation of longer and more amyloidogenic Aβ peptides, i.e., Aβ42 and Aβ43 [18, 108]. Overexpression of FAD-associated human PS may decrease the age of onset of cerebral amyloid deposition in APP tg mice to a few weeks of age [102] (Fig. 2).
Tg mice overexpressing human mutant tau, in addition to one or several APP and PS mutations, have been developed to study the interaction between Aβ and tau pathologies [47, 94, 115]. Tg rats have been generated utilizing similar strategies [16]. In general, in APPxtau double tg mice Aβ pathology seems to accelerate tau pathology, whereas tau overexpression does not affect Aβ pathology (see below).
In the tg rodents, Aβ aggregation is often observed in the form of diffuse plaques, with time-dependent maturation into mature, congophilic plaques, and is accompanied by a varying extent of vascular Aβ deposition. Congophilic plaques are accompanied by reactive astrogliosis and microgliosis, as well as dystrophic boutons with accumulation of hyperphosphorylated tau, but no neurofibrillary tangles [20]. Prominent Aβ deposition in the hippocampus and neocortex, which are brain regions also predominantly affected by β-amyloidosis in AD, is often achieved by choosing brain-selective neuronal promoters to drive transgene expression, or utilizing the endogenous APP gene including its promoter sequence. Vascular Aβ deposits can lead to microhemorrhages [53]. Aβ lesions in APP tg rodents include diffuse, focal and amyloid deposits as well as amyloid angiopathy; they appear thus similar to the ones found in human AD brains. By contrast, tau pathology in the single APP tg rodents is lacking or very mild contrary to what is seen in the humans [31].
Even though abundant cerebral β-amyloidosis can be observed in APP and APP PS tg mice, the overall phenotype appears mild. For example, behavioral deficits in the Morris water maze have been described [70, 129], and also neuritic abnormalities [88], but hardly any neuron loss has been found despite massive amyloid deposition [14, 106]. Since APP or APP PS tg rodents show age-related Aβ deposition but no extensive neuron loss, they are considered good models for the early, presymptomatic stage of the disease [81]. Importantly, Aβ aggregation can be studied in vivo under genetically and environmentally controlled conditions.
Seeding and Aβ aggregation
An aggregate of a specific protein may induce the aggregation of the homotypic protein present in tissue or in solution. The aggregate acts as a ‘seed’, catalyzing the aggregation, comparable to the first ice crystal that initiates (‘seeds’) the freezing of water at 0° C.
In vitro, the addition of preformed Aβ aggregates to a solution of soluble Aβ peptides significantly shortens the time for Aβ aggregate formation [50]. Moreover, Aβ aggregation is induced by seeding under conditions (low Aβ concentration, below the threshold for aggregation), and on a time scale in which, without seeds, Aβ peptides would remain soluble. When morphologically different types of Aβ aggregates are added, the resulting aggregates possess conformational properties of the seeds [98]—an observation that almost necessarily implies a direct contact of the native Aβ peptides with the preformed Aβ aggregates (Fig. 2c).
Prions, prion-like proteins and propagons
The theory of “infectious” protein misfolding has initially been developed in prion diseases [101]. Prion diseases, such as bovine spongiform encephalopathy, scrapie, and Creutzfeldt–Jakob disease (CJD) are caused by PrPSc, a misfolded and aggregated version, of the normal cellular prion protein (PrPc). According to the prion theory, a correctly folded PrPc protein becomes secondarily “misfolded” when it comes into contact with an already misfolded, aggregated form of the same protein (PrPSc). The term templated misfolding describes this misfolding event as a direct interaction of the aggregate with the native protein that then adopts the same misfolded conformation. The ‘transmissible’ or ‘infectious’ nature of PrPSc occurs on four levels: (1) the molecular level, i.e., the conformation of the misfolded prion protein is passed on to the native prion protein by templated misfolding (‘from molecule to molecule’); (2) the spreading within tissue, i.e., PrPSc particles can spread within a certain type of tissue, be it within peripheral tissue or within the brain; (3) across tissue, i.e., the prion disorders typically originate in peripheral tissues (e.g., spleen, peripheral nervous tissue) and later reach the brain of an infected individual, where they cause a fatal neurological disorder; and lastly, (4) from organism to organism, for example, in scrapie-affected sheep PrPSc particles that are present in peripheral tissue can be excreted into the environment, where they can persist due to their resistance to degradation and inactivation. These particles can then be taken up by other members of the flock that may develop the disease after a long incubation [110].
More than 30 different proteins are known to aggregate and cause amyloid disorders, often age related and, for some of them, associated with neurodegeneration [113]. However, only the prion disorders are known to be ‘infectious’ in the sense of level 4 above. The discovery that several of the proteins involved in protein misfolding disorders at least in vitro and possibly in vivo in animal models show similarities to the ‘infectious’ nature of the prion particles on the molecular and possibly the tissue level (in the sense of levels 1, 2, and 3 defined above), has led to somewhat confusing terminology. The term ‘prion-like’ is used to describe similarities of proteins, such as Aβ, tau, and α-synuclein, with PrPSc prion particles, on the molecular and possibly the tissue level. It does not imply a transmission between organisms (in the sense of level 4). However, this possibility is currently being discussed at least for Amyloid A (AA) amyloidosis in cheetahs, since systemic AA amyloidosis has been transmitted between cheetahs by ingested excrements [91]. Recent neuropathological data from iatrogenic CJD in recipients of growth hormones (GH) isolated from cadaver pituitary glands (CGH) raise the possibility of an interindividual transmission of cerebral Aβ amyloidosis (in the sense of level 4 above) under exceptional circumstances [66]. In this study, four of eight iatrogenic CJD patients showed substantial and, in two of the remaining four, some Aβ deposition in the parenchyma and in the vessel walls in addition to typical CJD lesions, suggesting that CGH, contaminated not only with PrPSc but possibly also with Aβ aggregates, had initiated seeded Aβ deposition at a relatively young age (36–51 years) and after long incubation times (21–32 years) [66]. However, despite the presence of Aβ deposits in these brains, none of the individuals showed AD symptoms, and it is currently unclear if the CGH indeed contained Aβ seeds. The review of the US National Hormone and Pituitary Program (NHPP) cohort database and of the medical literature did not show any increase in the incidence of neurodegenerative diseases in CGH recipients [61].
Attempts have been made to introduce new terminology to better describe and differentiate prion-like proteins such as Aβ from PrPSc prions. However, none of these is widely used so far possibly because the different levels of this complex process are not readily reflected and are still controversial for some of these proteins. Thus, instead of ‘prion’ or ‘prion-like’ we suggest adopting the term ‘propagon’, originally used by Cox et al. [24] in the context of [PS+] prions in yeast. We suggest expanding this concept by adding a description of what is being propagated or which specific aspect has been investigated. For example, a protein that propagates its conformation from molecule to homotypic molecule, i.e., on the ‘molecular level’, would be a ‘molecular propagon’ (Fig. 2c). Proteins that have the ability to spread within tissue and transmit their conformation would be ‘tissue propagons’ (Fig. 3a, b); spreading across tissue becomes a ‘systemic propagon’; and only proteins that transmit pathological conformations between individuals would be ‘infectious propagons’. The term ‘propagon’ implies a conformational variant of a protein that typically exists as a multimer. This terminology can be broadened to include functional amyloids that convey and execute diverse biological functions, for example in bacteria, in yeast, and possibly also in humans [21]: ‘functional propagon’ vs. ‘pathological propagon’.
Hypothetical propagation of Aβ pathology via diffusion or transport of Aβ seeds (‘tissue propagons’), or by indirect effects (non-prion-like). a Initial Aβ seeds and deposits (in red) form spontaneously in a permissive environment (e.g., high concentration of Aβ42 peptides). Since Aβ peptides are secreted and amyloid plaques form in the extracellular space, extracellular diffusion (or transport) of Aβ seeds could spread Aβ seeds and propagate seeded Aβ aggregation within tissue. b Alternatively, after initial formation of Aβ seeds, cellular uptake, intracellular transport, and release of Aβ seeds at the synapse could lead to seeded secondary deposits within neuronal networks. Aβ seeds (aka ‘molecular propagons’) that spread extracellularly (a) or intracellularly (b) would be considered ‘tissue propagons’. c Thirdly, neuronal impairment caused by Aβ aggregation may lead to cellular adaptation, including an increase in Aβ levels. Since Aβ aggregation is concentration dependent, this may lead to spontaneous Aβ aggregation at sites within the neuronal network. This scenario does not require the diffusion or transport of Aβ aggregates within neuronal networks. While the three scenarios highlight different possible mechanisms, they are not mutually exclusive
However, progressive spread of pathology as observed in AD or in other neurodegenerative diseases does not necessarily imply the existence of ‘propagons’. The plausibility of ‘propagons’—i.e., of protein aggregates that spread pathology by catalyzing pathological misfolding and aggregation of homotypic proteins—has to be carefully assessed experimentally, ideally by isolating the ‘propagon’, and interpreted in the light of human pathology.
Seeding in animal models: evidence for Aβ propagons
The APP tg rodents show that high levels of human Aβ peptides promote Aβ aggregation into amyloid deposits and cerebral amyloid angiopathy. However, it was unknown if each aggregation event (causing the development of one Aβ deposit) occurs independently and spontaneously, for example, as a consequence of an increase in the local concentration of Aβ peptides, or if Aβ aggregation once initiated, triggers further Aβ aggregation by a domino effect related to propagon mechanisms on one or several of the four levels discussed above. The experimental approach to test the hypothesis of a propagon mechanism requires two components: preformed Aβ aggregates and soluble, normally folded Aβ peptides, with a primary structure that can be subject to secondary misfolding. The classical experiment consists of the injection of a few microliters of a brain homogenate with Aβ aggregates (from an AD patient or a tg mouse with Aβ deposits) into the brain of a host that can develop—but does not yet show—any Aβ pathology, for example, a young APP tg mouse several months before spontaneous Aβ deposits would form (Fig. 2b).
The nature of Aβ seeds
In the initial experiment of Walker et al. [68, 125], dilute extracts of brain homogenates from AD cases were injected unilaterally into the hippocampus and the overlying cortex of tg mice bearing the APP “Swedish” mutation (Tg 2576 mice). Five months after the inoculation, Aβ deposition was observed at the site of injection and, to a lesser degree, contralaterally. The induced Aβ deposits were similar to spontaneous deposits that normally form much later in these animals, and, in many aspects, were indistinguishable to those seen in AD brains. At the age of analysis (8 months) Tg2576 mice do not show Aβ deposits spontaneously, or after injection with a control brain homogenate from a young non-AD case. IHC of mouse brains, up to 4 weeks after the injection with AD brain extracts, remained negative: Aβ deposits present in the inoculate could not be detected. The Aβ deposits observed at 8 months of age had thus developed de novo from Aβ secreted by the host, induced by the AD brain extract. Brain extracts from non-demented, aged individuals whose brains harbor some Aβ deposits can also induce Aβ aggregation in mouse brains, but to a lesser extent [68, 125]. Aβ accumulated in brains of presymptomatic, non-demented AD cases is thus in a conformation that is permissive for templated misfolding. By contrast, cerebrospinal fluid (CSF) from AD patients does not induce Aβ pathology even though CSF contains more than tenfold higher levels of Aβ peptides than soluble brain extracts, suggesting that Aβ seeds exist only in the brain, the site of Aβ aggregation and deposition [40]. Extracts from APP tg mouse brains harboring extensive Aβ deposits were shown to be also effective seeds [87]. In such mouse brain extracts, the likelihood of potentially confounding factors such as antigens able to evoke an immune response in the host (mouse against human proteins) or the presence of tangles (possibly present in the human homogenate) is avoided.
However, extracts from brains with Aβ deposits, once immunodepleted of Aβ, lose their seeding activity [87]. A similar effect is observed when the extract is treated with formic acid, which is known to denature proteins, including Aβ aggregates [87]. Finally, synthetic Aβ fibrils are able to induce Aβ aggregation in young APP tg mice [116]. These experiments led to the conclusion that Aβ peptides, in specific, aggregated conformations, are indeed the essential seeds.
Seeding extracts from tg mice may be separated by 100,000×g ultracentrifugation into insoluble (pellet) and soluble (supernatant) fractions. Both fractions can seed Aβ pathology [76]. The majority of Aβ immunoreactivity is found in the pellet (99.9 %) although the soluble fraction retains significant seeding activity—indicating that soluble Aβ seeds are more potent than insoluble Aβ aggregates [76]. One femtogram of soluble Aβ seeds (corresponding to ~130,000 Aβ molecules) derived from amyloid-laden AD brains can still induce Aβ aggregation in APP23 tg mice [40]. Sonication increases the amyloid-inducing activity of the extract—probably because it increases the number of seeds by fragmentation of the Aβ aggregates [76].
Aβ seeds seem remarkably stable and persistent. Boiling of brain homogenates harboring Aβ seeds reduces the seeding activity, but does not abolish it [87]. Likewise, formaldehyde treatment of brain tissue harboring Aβ aggregates reduces, but does not abolish, seeding activity [39]. It was found that insoluble Aβ seeds are relatively proteinase K (PK) resistant with 80 % of insoluble Aβ in brain homogenates remaining detectable and retaining seeding activity after 30 min of PK treatment. Aβ in the soluble fraction is largely PK sensitive and loses its seeding activity after PK digestion [76]. A recent study by Jucker and colleagues found that Aβ seeds can persist in APP-null mouse brain for months, and regain seeding activity in the presence of host Aβ [133].
The conformation of misfolded Aβ acting as seeds is still largely unknown [132]. Conformation-sensitive dyes suggest that several conformations are possible, and that the conformation present in the seed is passed on to the induced deposits [51]. This suggests a direct contact of the Aβ seed with the soluble, hitherto not aggregated Aβ peptides, and possibly the incorporation of the soluble peptides into a growing seed (Fig. 2c).
Modulators of Aβ seeding in APP tg rodents
Seeding is time dependent—the longer the incubation, the more Aβ deposition is observed. Anti-Aβ IHC of mouse brains is able to detect seeded Aβ deposits after a lag time of a few weeks [87]. More sensitive methods suggest that Aβ aggregation is induced immediately after injection of the seeding extract and builds up over time [134]. Seeding is less efficient when the original extract is diluted [40, 87], and more efficient with enhanced sonication of the seeding extracts that presumably leads to fragmentation of existing seeds [76]. This suggests that the effect also depends on the number and the concentration of seeds. The levels of soluble, native Aβ peptides available in the host also determine the efficiency of Aβ seeding (the higher the Aβ levels in the host mice, the shorter the lag time) [35]. Passive immunization of host mice against Aβ peptides reduces the efficacy of seeding, as does mixing the seeding extract with an anti-Aβ antibody before the inoculation, and suggests that binding of antibodies to Aβ seeds facilitates their degradation or can inactivate them in other ways [87].
The local environment in which the seed is placed plays an important role in the efficiency and in the morphology of the induced Aβ aggregates. The contrast between hippocampus and striatum is illustrative in this respect. In aged APP23 tg mice, spontaneous Aβ deposits are abundant and occur early in the hippocampus and are absent or rare in the striatum [117]. Aβ seeding extract injected into the hippocampus of young APP23 tg mice may induce Aβ deposits within a few weeks, and significant amounts are detectable by IHC 3 months after the inoculation [34, 87]. Induced deposits are largely diffuse, but mature, congophilic plaques are also observed, especially with longer incubation [76]. When the same seeding extract is injected into the striatum, a brain region where tg APP is expressed at lower levels than in the hippocampus and where no Aβ deposition is usually observed, seeding results in the development of only diffuse deposits within the observation period [34]. This suggests that factors provided by the cellular microenvironment can modulate the polymorphism of induced Aβ aggregates.
For the initiation of cerebral β-amyloidosis, the presence of Aβ seeds in the seeding extract, but not the age of the host at the time of injection, seems critical [48]. The typical age-related onset of Aβ aggregation in the human brain is probably due to the late occurrence of seeds; were persistent seeds present at a younger age, progressive Aβ aggregation would likely occur earlier. The modulators of Aβ seeding could be exploited therapeutically to delay pathological Aβ aggregation. Current efforts aiming to lower Aβ levels by BACE or γ-secretase inhibitors or modulators, or removal of Aβ peptides and Aβ aggregates by anti-Aβ immunotherapy all should also reduce seeding efficiency [36].
Does seeding of Aβ pathology occur in humans?
In experimental models, the initial amyloid deposits occur at the site of injection of Aβ seeds. In human sporadic cases, the neocortex is the initial focus. Neuropathology or imaging studies do not point to a specific area in the neocortex. Such a topography is poorly compatible with the involvement of an exogenous seed—at least to our current state of knowledge. The alternative of initial, spontaneous, and concentration-dependent Aβ aggregation due to a defect of clearance or to excessive production of Aβ is plausible. The spontaneously formed aggregate could then subsequently act as an endogenous seed. Currently, evidence for this mechanism is sparse in AD, but seems possible, based on the neuroanatomical spread of Aβ pathology (discussed in more detail below). The recent observation of unusual Aβ deposits in iatrogenic CJD patients who may have received CGH contaminated with Aβ seeds adds new elements to the discussion. Aβ seeding in humans might be fairly inefficient, since it seems to take decades for Aβ deposits to form [66]. The progression from initial Aβ deposits in sporadic AD cases to widespread Aβ pathology also takes years to decades [9, 32].
Dissemination of the misfolding: molecular Aβ propagons?
According to the prion hypothesis, aggregates present in the seeding extract impose their misfolded conformation directly onto soluble, homotypic proteins of the host. Direct contact of misfolded Aβ with host Aβ has not been visualized. Currently, the characteristics of the misfolding and of the aggregates cannot be directly accessed.
In animal models
There is indirect evidence that immediate contact of Aβ seeds and soluble Aβ takes place. Different types of Aβ aggregates, assessed by different staining affinity and morphology, propagate their respective conformation in seeding experiments: APP23 and APPPS1 tg mice accumulate Aβ in deposits that have different morphologies and tinctorial affinity. When brain extracts from aged, amyloid-laden APP23 mice are injected into brains of young APPPS1 mice, the induced deposits observed in APPPS1 brains have characteristics reminiscent of the APP23 deposits and vice versa [51]. In the same way, susceptible mice, injected with extracts from sporadic AD cases or familial cases with either the APP Swedish or the APP Arctic mutations, developed different types of deposits. These morphologically distinct types could still be recognized after a second passage [128]. Finally, synthetic fibrils, containing a variable proportion of Aβ40 and Aβ42, also induce the development of morphologically different deposits [116]. In addition, the animal seeding studies suggest that at least some of the seeded Aβ deposits may be diffuse initially and convert to mature, congophilic plaques over time [76].
In humans
Identification of a specific mechanism of Aβ misfolding in humans would require the detection of a specific type of deposits that itself would be linked to a particular type of misfolding. However, the variable shapes of the Aβ deposits observed in AD principally depend on their maturation stage and on their topography [86]: given the limits of cross-sectional observations, one can suppose that all the Aβ deposits are initially diffuse, i.e., devoid of an amyloid core. In the striatum, they remain diffuse, whereas in the neocortex, they become amyloid (i.e., with a dense, Congo red-positive core) and are secondarily surrounded by a neuritic crown. In the presubiculum, as in layer pre-α of the entorhinal cortex, the deposits are large and diffuse. Once those time and space determinants have been taken into account, there are no peculiar aspects that could distinguish types of deposits specific to a given “strain” of Aβ-with the sole exception of cotton-wool plaques. Cotton-wool plaques, homogeneous and Congo red negative, have a distinct aspect; they were initially described in FAD caused by the deltaE9 PS1 mutation, and are also rarely found in sporadic cases [77]. To our knowledge, there has been no attempt to seed the pathology in tg mice with homogenates of cerebral cortex containing this type of plaque.
Progression of Aβ pathology: tissue propagons?
Possible modes of progression: stochastic, by selective vulnerability, or through propagation
The time-dependent increase in the number of brain areas affected by Aβ pathology could be explained by several mechanisms. Protein aggregation in the different foci could occur independently and be related to a stochastic process. This possibility can readily be dismissed in the case of Aβ deposition. The stereotypical progression of the lesions observed in animals and humans is incompatible with a random process. Alternatively, progression could be the consequence of different sensitivities of different neuronal populations—a phenomenon described as “pathoclisis” or “selective vulnerability”. Some neuronal populations may be more vulnerable because the expression level of the amyloidogenic, disease-defining protein is high. Selective vulnerability could also be related to the proteome of the cell that facilitates or protects against protein aggregation. Lastly, progressive Aβ pathology could be governed by propagation.
Possible ways of propagation
The term propagation, applied to the pathology observed in neurodegenerative diseases, means that a change in one primary focus is seen at a more advanced stage of the disease in a secondary focus. When the propagation concerns an accumulation of a protein that is not, or only incompletely, cleared, the primary focus remains affected when the secondary focus becomes involved. The primary focus, where disease continues to progress, is usually affected more heavily than the secondary one. The number of areas in which the accumulation of the specific protein is observed increases with time (secondary foci give rise to tertiary foci, etc.). Propagation implies a transport of a pathogenic molecule or signal from the primary to the secondary focus (Fig. 3). Most probably, it is the aggregated protein itself that is transported. It can recruit homotypic soluble proteins and incorporate them into the growing aggregates in the primary as well as in the secondary foci.
Remarkably little is known about the possible existence of propagation of Aβ aggregates (i.e., Aβ propagons) in the human brain, and even less about how Aβ propagons might be transported (in the extracellular space, in axons or dendrites, antero- or retrogradely, in connection with tau pathology or independently).
Transport in the brain may occur along at least three different pathways:
Connections
Propagation through connection implies selectivity in the secondary focus: it must be a target zone of the axons of the primary focus; alternatively, the primary focus may be a target zone of the secondary focus (if the propagation implies retrograde transport). This selectivity is never as apparent as when the primary and secondary foci are not contiguous.
Diffusion
If passive diffusion of the aggregates takes place through the extracellular space, it is expected that the involved areas would be contiguous unless modified by specific vulnerability.
Diffusion through basement membrane of the vessels
A third way of propagation is through the basement membrane of the capillaries or arteries [15]. The protein accumulation would then be centered around the vessels.
Propagation of seeded Aβ aggregation in tg animals
The induced deposits are first detectable by IHC several weeks to months after the injection and appear locally at the site of injection [34, 48, 68, 87, 124, 125]. With longer post-injection incubations, the amyloid load at the site of injection increases, and can expand to additional brain areas [34, 48, 125]. The newly affected brain regions are areas connected to the primary site of injection. For example, when Tg2576 mice were inoculated unilaterally into the hippocampus, induced deposits appeared in the ipsilateral and later in the contralateral hippocampus, but also in the ipsilateral entorhinal cortex [68, 125]. Likewise, injection of Aβ seeds into the entorhinal cortex in young APP23 tg mice leads to the induction of Aβ deposits locally and later in the outer molecular layer of the dentate gyrus, connected to the entorhinal cortex via the perforant path [34, 67]. The propagation can thus be retrograde (from the hippocampus to the entorhinal cortex) or anterograde (from the entorhinal cortex to the molecular layer of the dentate gyrus). The entire cortex of R1.40 mice appears filled with Aβ deposits 12 months after a single injection of Aβ-laden brain extract into the hippocampus and overlaying cortex [48].
In young APP23 tg mice still devoid of Aβ deposits, cerebral β-amyloidosis can not only be induced by intracerebral, but also by intraperitoneal application of the seeding extract [35, 37]. Much higher amounts and longer incubation periods are then needed. While the induction seems related to misfolded Aβ species in the inoculum, it is unclear if and how Aβ seeds are shuttled to the brain. The integrity of the blood–brain barrier (BBB) in APP tg mice has been questioned. BBB leakage could contribute to the transfer of Aβ seeds from the periphery to the brain. Other peripheral routes (intravenous, intranasal, intraocular) have been tested for Aβ seeding in the rodent models, but did not induce cerebral β-amyloidosis at the concentration and incubation times assessed [34, 67].
The mechanisms involved in the spread of seeded Aβ pathology are still unknown. Secondary Aβ deposits are observed several months after the inoculation of the seeds in the APP tg mice. This delay seems related to three complementary processes: the build up of new seeds at the site of the inoculation; the transport or the diffusion of the seeds; and the seed-initiated Aβ aggregation at the secondary site (Fig. 3). The spread of the initial (injected) seeds is probably limited [34, 67]. The lag period observed for the development of secondary deposits is partly due to the generation of new seeds at the initial site that could precede the spread [134]. The transport of the seeds could be assisted by extra- or intracellular components, and would then be guided, directional, and non-random. It could also be explained by a concentration gradient of Aβ seeds from the initial site of injection to nearby and connected brain regions; a non-directional, random distribution of seeds is then expected. Such a homogeneous distribution of seeds does not necessarily mean, however, that the induced Aβ deposits have to be homogeneous or random. The concentration of seeds is but one factor determining Aβ aggregation. The availability of soluble, native Aβ peptides for misfolding is also critical.
The spatiotemporal progression of seeded Aβ deposits in APP tg rodents suggests that at least part of the spreading takes place along neuroanatomical pathways [67, 134]. From the hippocampus where the seeds are inoculated, Aβ aggregation progresses in the limbic connectome and propagates beyond the first-order synapses to distant regions of the brain [67, 134]. The progression may be modified by experimental lesions: in one experiment involving young tg mice overexpressing APP with the Arctic mutation E693G, the subiculum, the first structure with Aβ deposits in that tg line, has been partly destroyed by ibotenic acid. That lesion impeded the spread of Aβ pathology in CA1, which projects to the subiculum, and in the retrosplenial cortex, which receives projections from it [41].
It is currently unknown if Aβ seeds are being transported in vivo, and if such transport is extracellular or intracellular (Fig. 3). Until more direct evidence for the transport or spread of Aβ seeds along neuroanatomical pathways in vivo is available, alternative hypotheses need to be considered. Alternatively, or in addition, propagation of Aβ pathology could also be influenced by the activity of the neurons that modifies Aβ levels. Changes in neuronal activity due to local Aβ aggregation could lead to an increase in Aβ secretion in some connected areas where it could result in spontaneous Aβ aggregation (Fig. 3c).
Does propagation occur in humans?
The progression of Aβ deposition in the human cortex is not random. A recurrence in the distribution of Aβ deposits is evidence of a progression that has been “sliced” into stages (A, B, C) by Braak and Braak [8], or into “phases” by Thal et al. [120]. Briefly, the neocortex is involved in phase 1 (the initial cortical focus from which the pathology develops has not been identified, if it exists); the hippocampus is additionally involved in phase 2, followed by the lenticular nucleus and thalamus (phase 3), the mesencephalon (phase 4), and lastly, the cerebellum (phase 5). The “phases” adequately describe a reproducible, stable and stereotyped gradient of lesion density that has not found yet its definite explanation. Is that gradient the consequence of propagation? Generally speaking, Aβ deposits are found in the gray matter and rarely and in small quantity in the white matter. This specific topography indicates that they are more probably related to the somatodendritic compartment of neurons, or to synapses, confined in the gray matter, than to glia or to axons, also abundant in the white matter. Study of Aβ distribution within the brain provides compelling evidence of both, diffusion of Aβ and of its transport through connections.
Transport through connections
If passive diffusion of Aβ throughout the brain were the only mechanism responsible for the propagation of Aβ pathology, one would expect a continuity of the involved areas. This is not the case: there are striking examples of spared areas in the immediate neighbor of heavily involved ones. A few examples are presented here:
-
In the lenticular nucleus, the putamen may contain numerous diffuse deposits while the pallidum next to it is spared (Fig. 4). Many neurons of the putamen are monosynaptically connected with neurons in the external and internal pallidum [78]. Selective vulnerability could, however, be held responsible for the striking contrast between the two parts of the lenticular nucleus.
Fig. 4 Human brain. Discontinuity in the propagation of Aβ deposits. Diffuse deposits are seen in the putamen (shown by ‘plus’ sign), but are absent in the immediately adjacent pallidum (indicated by ‘asterisk’). Immunohistochemistry with 6F/3D antibody (Dako). The diagram on the left side shows the position of the microscopic view (composite images). Scale bar 500 µm
-
In the dentate gyrus of the hippocampus, the first Aβ deposits are found in the outer zone of the molecular layer, which only receives the axons of the pre-α layer of the entorhinal cortex [30, 59]. Diffusion or selective vulnerability cannot explain that particular topography: deposition, in both instances, should involve the whole molecular layer (Fig. 5). Connection must be involved.
Fig. 5 Human brain. Tau pathology precedes Aβ deposits in the outer molecular layer of the dentate gyrus. Ammon’s horn of one case, stained with haematein–eosin (a, b) and immunostained with AT8 phospho-tau (c) and 6F3D Aβ (d) antibodies. The same area has been captured with a Hamamatsu slide scanner and viewed at low magnification (enlargement ×1.25) in a and at ×20 in b, c, and d. a The rectangle is located in the molecular layer of the dentate gyrus and corresponds to the microscopic fields shown in b, c, d. In b, c, and d the limit between the inner (plus sign) and outer molecular layers (asterisk sign) is indicated by arrows. There is vacuolation of the outer molecular layer (asterisk) which receives the axons from the pre-α layer of the entorhinal area in which tau pathology is abundant. b Haematein–eosin stain. c Aβ IHC. No deposit is visible in the molecular layer. d Tau IHC: accumulation of phosphorylated tau in thin neurites and dots exclusively located in the outer molecular layer (short black arrows)—projection zone of the pre-α layer of the entorhinal area. Inset: digital enlargement to show tau-positive neurites and dots. Note that, at this stage, tau pathology affects only very thin processes devoid of spines, probably axons
-
In the neocortex, Aβ deposits are mainly located in the upper part of the cortical ribbon with differences depending on the type of deposits [27] and the area (reviewed in [74]). This differential distribution is generally taken as evidence for the involvement of cortico-cortical connection.
-
In the molecular layer of the cerebellum, diffuse deposits may form streaks, perpendicular to the surface of the folium, mimicking the projection of the climbing fibers (Fig. 6d). To our knowledge, a correlation between this aspect and the involvement of the inferior olive from which the climbing fibers originate has never been sought.
Fig. 6 Human brain. Specific types of Aβ deposits that suggest passive diffusion, or transport through connections. a–d Anti-Aβ immunohistochemistry with 6F/3D antibody (Dako). a Subpial Aβ deposits. The deposits (arrows) are not related to connections but are more likely due to diffusion to or from the cerebrospinal fluid. Scale bar 50 µm. b Aβ deposits along calcified vessels. The calcified vessels (arrows) are seen in the hippocampal region—a common finding in aged AD cases. Aβ deposits are seen around some of the calcified profiles. Passive diffusion of soluble Aβ probably explains the deposits. Scale bar = 20 µm. c Tangle-associated amyloid deposit. A long arrow points to the ghost tangle (stained in blue by haematoxylin). Aβ deposits (short arrow) are in contact with the tangle. Scale bar 10 µm. d Aβ deposit in the molecular layer of the cerebellum. The deposit is perpendicular to the axis of the parallel fibers, as are the climbing fibers, originating from the inferior olive. Arrow on a Purkinje cell. Scale bar 50 µm
Diffusion in the extracellular space
The role of extracellular diffusion has been shown experimentally: wild-type grafts in young APP23 tg mice contain Aβ deposits as soon as 3 months after grafting. Extracellular diffusion appears to be the most likely means of propagation since few axons cross the border between host tissue and graft [89]. The shape and topography of the deposits in humans, also suggest a mechanism of deposition that is independent from connections in some instances.
We illustrate this point with the following examples:
-
The subpial deposits form a continuous band of immunoreactive material of variable thickness along the surface of the cortex, in close contact with the CSF (Fig. 6a); similarly some diffuse deposits border and cover the small pyramidal cell clusters of layer II of the presubiculum. The shape and the distribution of those deposits are poorly compatible with connections.
-
The Virchow–Robin spaces are often surrounded by a ring of immunoreactive material. The shape of the deposits is best explained by the flow of the extracellular fluid.
-
Extracellular neurofibrillary tangles may form the nidus of an Aβ deposit—at the origin of “TAAD” (tangle-associated amyloid deposit) [58, 111] (Fig. 6c).
-
Aβ may aggregate in contact with calcified vessels (Fig. 6b).
-
The vascular deposits are not tightly related to the parenchymal deposits and probably not linked to vascular innervation, being also present in veins. CAA in the cerebellum is for instance observed in cases without parenchymal deposition in the cerebellum and often in the absence of deposition in the vessel walls of the basal ganglia. The basal ganglia may, however, already contain parenchymal deposits as noticed by Thal et al. [119] who proposed a CAA staging different from the phases of parenchymal deposition [120].
In summary, the distribution and the shape of the Aβ deposits indicate that both diffusion of extracellular molecules and transport through connection likely take place. The role of connections seems less exclusive for Aβ than for tau progression. An exceptional post mortem case illustrates the contrast. Aβ deposits were present in a piece of cerebral cortex that had been disconnected by a surgical lesion decades before AD developed. In contrast, the disconnected cortex was devoid of tangles and neurites: Aβ deposits did develop, but tau pathology did not in the absence of connections [33].
Possible mechanisms of propagation
There are several ways by which connections may play a role in the propagation of Aβ deposits. It is tempting to draw arrows along fiber tracts from one region of the brain to another to fit the phases of the disease (for instance, from the neocortex to the entorhinal cortex and from there, to the hippocampus, from the cortex to the basal ganglia, from the occipital cortex to the superior colliculus, etc.), but one has to remain aware of the numerous connective pathways of the brain. The saying that “four synapses are enough to go anywhere in the brain” must be kept in mind to avoid construction of hypothetical propagation pathways.
If Aβ were to behave like a tissue propagon, similar to prions, misfolded Aβ should be involved in the propagation through connections. In that hypothesis, Aβ seeds are taken up by the neuron, transported to another area by anterograde or retrograde transport and secreted (“pure models”). However, there is strong evidence, in animals as in humans, that tau pathology plays a major role in the progression of Aβ pathology that will be discussed later (“hybrid models”).
Pure model-anterograde: propagation of Aβ aggregates from primary to secondary foci by anterograde transport
In the simplest hypothesis, Aβ produced at a primary focus is internalized and transported anterogradely to the next synapse (Fig. 7a). Such a mechanism has been suggested for the progression of Aβ pathology from the neocortex to the entorhinal cortex and hence to the hippocampus, or from the neocortex to the putamen. There is also evidence for a link between the deposits observed in the brainstem and in the cerebellum [23]. In that hypothesis, the neocortex, for a reason that remains to be elucidated, is the initial focus (not fed by any other initial focus of aggregation) and Aβ is transported from the neocortex to secondary foci (entorhinal cortex and hippocampus) and from secondary to tertiary foci, etc.
Hypothetical ways by which Aβ is transported antero- or retrogradely in a model where only Aβ is implicated (“pure models”). a The initial Aβ deposit occurs around the soma and the dendrites of a neuron. Aβ is internalized and transported anterogradely to the axon ending. There it seeds a secondary focus. b The primary focus is found at the axon ending. The Aβ is then internalized and transported retrogradely to the soma and the dendrites, where the secondary deposits develop
This hypothesis faces several drawbacks:
The model implies the presence of Aβ within the neurons: the role of intracellular Aβ has been advocated by some [45] and criticized by others, at least in regard to human pathology [1]. Any conclusions drawn from IHC studies are highly dependent on the sensitivity and specificity of the antibodies used. In humans, the detection of an intracellular signal is mainly observed with antibodies directed against the N-terminal part of Aβ, antibodies that appear to also recognize C-terminally cleaved APP (C99). Antibodies directed against the C terminus of Aβ may, however, label intracellular Aβ in severely affected cases, leaving open the possibility of an intraneuronal circulation of aggregated Aβ in the late AD stages.
The absence of Aβ immunoreactivity in the white matter and, in general in fascicles of axons (such as the pillars of the fornix) argues against the direct transport of fibrillar Aβ from one region to another. However, the argument is not decisive: traces of fibrillar Aβ might be enough to induce seeded aggregation and could remain undetectable by current methods. The contrast between Aβ and tau is, however, striking: there is no trace of Aβ microscopically visible in the axons, which, on the contrary, may contain aggregated tau.
Finally, a negative argument may be added: there are cases in which Aβ deposits in a secondary focus are not associated with deposition of Aβ in the primary focus. The early deposition of Aβ in the outer zone of the molecular layer of the dentate gyrus, for instance, is rarely associated with Aβ accumulation in the entorhinal cortex. More numerous, probably, are the situations in which the accumulation of Aβ in a primary focus is not accompanied by deposition in the projecting zone: the most illustrative example is the putamen that projects massively to the pallidum. Early in the progression of the disease, the putamen may be filled with Aβ deposits while the pallidum remains unaffected.
Pure model retrograde: propagation of Aβ aggregates from primary to secondary foci by retrograde transport
Could the alternative hypothesis of a retrograde transport of Aβ aggregates from a primary to a secondary focus be plausible (Fig. 7)? The hypothesis does not fit the late occurrence of Aβ deposits in the subcortical nuclei sending their axons to the cortex such as the nucleus basalis of Meynert, the raphe nuclei, and the locus coeruleus (which by contrast are rapidly and severely affected by neurofibrillary pathology). Similarly, if retrograde transport were the rule, the putamen, which receives massive axonal projections from the neocortex, should be involved first and the neocortex but secondarily. The opposite is actually true.
From the above discussion, one may infer that connections are probably involved in the propagation of part of Aβ pathology. An anterograde transport of Aβ seeds from the neocortex where the first deposits are seen to the other structures that are successively involved is more plausible than the retrograde transport—although both anterograde and retrograde propagation of seeded Aβ pathology have been identified in tg mice—see above [41].
Synergy between Aβ and tau pathology: hybrid models of propagation
Several lines of evidence, in vitro, in animal models, and in humans, indicate that tau and Aβ interact.
In vitro
There is evidence that the N-terminal fragments of tau [13] or the “C-terminally truncated forms of Tau” [69] are secreted into the extracellular space. This extracellular tau is regulated by neuronal activity [99] and could modulate Aβ secretion [13]—although data are contradictory [69].
In animals
Most data in animal models indicate that Aβ enhances the induction and progression of tau pathology while tau pathology does not seem to influence Aβ deposition. Compact, congophilic Aβ deposits, induced or spontaneously formed in APP tg animals, are surrounded by degenerating neuritic boutons in which hyperphosphorylated tau has accumulated [76]. Human mutated APP and human mutated tau tg mice have been crossed to study the interaction of Aβ and tau pathologies [100]. Neurofibrillary tangles are initially found in the entorhinal cortex in tg mice expressing P301L human tau predominantly in that area (rTgTauEC) [135]. With age, tau pathology progresses along connections. APPswe/PS1dE9 tg mice develop amyloid deposits which are already numerous at 10 months of age. Both Aβ and tau pathology are observed in crossed rTgTauEC × APPswe/PS1dE9 tg mice. While Aβ pathology is not worsened by tau aggregation, tau pathology develops more rapidly, spreads more widely, and is associated with more severe neuronal loss in the presence of Aβ deposits [100]. Tau truncation and misfolding are also increased when a tg tau mouse is crossed with an APPxPS1 mouse [52]. Injection of Aβ42 fibrils into tau P301L tg mice caused a fivefold increase in neurofibrillary tangles in the amygdala from where neurons project to the injection site [44]. Tau pathology occurs earlier in B6/tau P301L mice after infusion of brain extracts containing Aβ deposits [7]. Finally, clearance of Aβ by immunotherapy induces a partial clearance of tau aggregates [93]. If Aβ enhances tau pathology, it appears that tau is implicated in Aβ toxicity, which is reduced when endogenous tau levels are decreased [103].
In humans
Are there data supporting the induction of tau aggregation by Aβ accumulation?
According to the amyloid cascade hypothesis [49], Aβ deposition occurs first in AD and leads to tau hyperphosphorylation and intracellular tau aggregation (Fig. 8a). In rodents, tau pathology is accelerated by Aβ accumulation. In humans, however, tau pathology appears to precede Aβ accumulation at least in some areas [10, 32]. Tau and Aβ pathologies do not develop in the same areas simultaneously—as would be predicted if they interacted through the plasma membrane of the neuronal cell body or of its dendrites. Does tau pathology then develop in neurons projecting to areas where amyloid deposits are found? The subcortical neurons that are affected early and selectively by tau pathology are indeed those projecting to the cortex [42]. According to Mann and Hardy [83], it is Aβ deposition in the cortex that induces tau aggregation in the subcortical neurons whose axons reach the deposits.
Hypothetical ways by which Aβ and tau could interact. Tau and Aβ pathologies could interact in two contrasted ways. The extracellular Aβ seeds could be endocytosed by the neuron and initiate tau pathology by mechanisms which remain to be elucidated (a). This is the hypothesis defended by Mann and Hardy [83]. In the alternative hypothesis (b), developed by Del Tredici and Braak [12], tau pathology is initial. The neurons in which tau has aggregated could be responsible for Aβ accumulation at least in two ways: they could abnormally secrete Aβ maybe in “non-junctional varicosities of axons generated from abnormal tau-containing brainstem nuclei” [11], or in terminal fields (neuron labeled α). Alternatively, as the neuron labeled β, they could become unable to clear Aβ, secreted by other neurons (in blue)
Are there, on the contrary, data supporting the induction of Aβ accumulation by tau aggregation?
According to the alternative hypothesis, “extracellular and aggregated amyloid-Aβ may only be produced under pathological conditions by nerve cells that contain abnormal tau” [12] (Fig. 8b). Many neuropathological observations in humans indeed support, or are at least compatible with, the possibility that tangle-bearing neurons are those that secrete Aβ in their terminal fields. Tau pathology developing in the locus coeruleus [10] and in the raphe nuclei [46] could initiate (rather than be the consequence of) the development of cortical Aβ deposits [11]. Aβ could be secreted, in the cerebral cortex, by the non-junctional varicosities found on the axons of subcortical neurons (such as those of the locus coeruleus) when they are affected by tau pathology [11]. There are other examples of amyloid deposition occurring in the projection zone of tangle-bearing neurons. Three striking examples illustrate this point.
In the entorhinal–dentate system
As mentioned earlier, Aβ deposits are initially found in the outer zone of the molecular layer of the dentate gyrus. Their presence is directly correlated with the previous development of tau pathology in layer pre-α of the entorhinal cortex, which is, at this stage, devoid of Aβ deposits [30, 59]. The layer pre-α neurons of the entorhinal cortex project precisely to the outer molecular layer of the dentate gyrus. Degenerating neurites—principally axons [109]—surround focal deposits in “mature” or “neuritic” senile plaques. The degenerating axons found in the plaques of the outer molecular layer necessarily originate from the neurons of the entorhinal cortex (see Fig. 5).
In the subiculum–fornix–mammillary body system
Aβ deposits develop in the mammillary body when tau pathology affects the subiculum that projects to the mammillary body.
In the neocortical–putaminal system
Aβ deposits do not appear immediately in the putamen at Thal phase 1 when numerous diffuse deposits appear in the neocortex still devoid of tau pathology. The development of Aβ deposits in the putamen (Fig. 4) occurs only at Braak neurofibrillary stages V or VI [4]—i.e., when tau pathology involves the neocortical neurons that project to it.
The hypothetical initiation of Aβ accumulation by tau pathology raises questions. Neuronal activity has been shown to increase Aβ secretion and, at an early stage, tau pathology is responsible for neuronal hyperexcitability [25]. In tangle-bearing neurons, however, tau accumulates also in the axon and probably impedes the axonal transport (although normal functioning of tangle-bearing neurons has also been advocated [72]). It is dubious that a degenerating axon, in which the transport is hindered, secretes more Aβ. Could it be then that a defect in the clearance of Aβ, possibly secreted by the receptive neuron, causes the accumulation (Fig. 8, b neuron labeled β)? The mere interruption of the axonal transport, however, cannot be held responsible for Aβ accumulation in the receptive synapse: there are many pathological circumstances in which axonal flow is impeded or areas are disconnected, without Aβ accumulation.
Despite the morphological evidence of the early development of tau aggregation, the role of Aβ as the trigger of AD pathology cannot be dismissed for several reasons. Aβ accumulation is lacking (or is contingent) in all tauopathies but AD [71]. Genetic evidence also strongly supports the crucial role of Aβ: there is no mutation on tau pathways that induces Aβ deposition [43]. All the mutations that cause FAD involve genes implicated in Aβ metabolism [92]. It is still unclear why such mechanistic evidence is not associated with morphological proof: the understanding of Aβ pathology could be biased by the morphological approach. Only the visible accumulations of Aβ are included in the model, not a possible, but invisible increase in Aβ concentration.
Increased Aβ concentration due to enhanced production or decreased clearance appears thus to be a prerequisite to the aggregation and deposition of Aβ. The deposits themselves may then be localized to certain foci by the effect of connections, especially when those connections are affected by tau pathology, a “molding” process that explains their peculiar distribution. Taken together, the data suggest a synergistic action: increased Aβ concentration is necessary to induce the extensive tau pathology observed in AD. Tau pathology shapes the Aβ deposits and contributes to concentrating them in specific areas, layers or subnuclei.
Summary and perspective
Genetic and neuropathological evidence demonstrates that Aβ aggregation and deposition are integral elements of AD pathogenesis. In vitro and in animal models, aggregated Aβ peptides can have ‘propagon’ properties: minute amounts of Aβ aggregates (Aβ seeds) can impose the misfolded state onto homotypic proteins, and induce Aβ aggregation. The seeds are active at low concentration and are relatively resistant to denaturation and degradation. Seeding is more efficient in hosts that produce high levels of soluble Aβ for incorporation into aggregates. Active or passive transport of the seeds explains the propagation of Aβ aggregation in the mouse brain, or, in some experimental settings, from the periphery to the brain. Human data suggest that such a ‘propagon’ mechanism could explain at least part of the propagation of Aβ pathology in AD.
In prion diseases, the pathogenic prions and the subsequent templated misfolding may be transmitted from molecule to molecule (level 1), may spread in tissues (level 2), across tissues (level 3), and from one individual to another (level 4). Experimental evidence indicates that Aβ can have a prion-like behavior up to level 3. There is no evidence of interindividual transmission, except possibly in the exceptional circumstance of iatrogenic CJD due to cadaver GH that could be associated with Aβ amyloidosis. To better differentiate and describe the different aspects of this process for proteins other than the prion protein PrP, we suggest the term ‘propagon’ qualified by the level at which the propagation has been investigated or observed (e.g., molecular propagon, tissue propagon).
There is no direct evidence for seeding in human AD, but the propagation of Aβ pathology follows stereotypical stages that may suggest transmission of templated misfolding through diffusion and via connections. Experimentally, Aβ can accelerate tau pathology in AD models but tau has never been shown to induce Aβ pathology. However, tau pathology in humans seems to precede focal Aβ accumulation in several circuits such as the entorhino-dentate, the cortico-putaminal and the subiculo-mammillary axonal projections. Aβ accumulation appears crucial to the extension of tau pathology, and tau pathology appears to confine at least part of Aβ pathology to certain networks of connections.
In summary, much remains to be done in experimental animals and in humans to better understand AD pathology and to open new therapeutic perspectives: to understand the molecular mechanism of Aβ misfolding, to identify the structural identity of Aβ propagons, and to improve our knowledge of the propagation of pathology within the brain tissue. New tools have recently been developed, such as new conformation-selective amyloid stains and new ligands that allow researchers to follow the initiation and propagation of tau and Aβ pathology in vivo. These tools will hopefully allow us to better analyze the propagation of Aβ aggregation in the brain and to better understand its relationship with tau pathology.
References
Aho L, Pikkarainen M, Hiltunen M, Leinonen V, Alafuzoff I (2010) Immunohistochemical visualization of amyloid-beta protein precursor and amyloid-beta in extra- and intracellular compartments in the human brain. J Alzheimers Dis 20:1015–1028. doi:10.3233/JAD-2010-091681
Ashe KH, Zahs KR (2010) Probing the biology of Alzheimer’s disease in mice. Neuron 66:631–645. doi:10.1016/j.neuron.2010.04.031
Bateman RJ, Munsell LY, Morris JC, Swarm R, Kevin E, Holtzman DM (2006) Quantifying CNS protein production and clearance rates in humans using in vivo stable isotope labeling, immunoprecipitation, and tandem mass spectrometry. Nat Med 12:856–861. doi:10.1038/nm1438.Quantifying
Beach TG, Sue LI, Walker DG, Sabbagh MN, Serrano G, Dugger BN et al (2012) Striatal amyloid plaque density predicts Braak neurofibrillary stage and clinicopathological Alzheimer’s disease: implications for amyloid imaging. J Alzheimers Dis 28:869–876. doi:10.3233/JAD-2011-111340
Benilova I, Karran E, De Strooper B (2012) The toxic Aβ oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat Neurosci 15:349–357. doi:10.1038/nn.3028
Bertram L, Tanzi RE (2012) The genetics of Alzheimer’s disease. Prog Mol Biol Transl Sci 107:79–100. doi:10.1016/B978-0-12-385883-2.00008-4
Bolmont T, Clavaguera F, Meyer-Luehmann M, Herzig MC, Radde R, Staufenbiel M et al (2007) Induction of tau pathology by intracerebral infusion of amyloid-beta-containing brain extract and by amyloid-beta deposition in APP × Tau transgenic mice. Am J Pathol 171:2012–2020. doi:10.2353/ajpath.2007.070403
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82:239–259
Braak H, Braak E, Silverman W, Wisniewski HM, Bobinski M, Wegiel J (1997) Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging 18:351–357
Braak H, Del Tredici K (2011) The pathological process underlying Alzheimer’s disease in individuals under thirty. Acta Neuropathol 121:171–181. doi:10.1007/s00401-010-0789-4
Braak H, Del Tredici K (2013) Amyloid-β may be released from non-junctional varicosities of axons generated from abnormal tau-containing brainstem nuclei in sporadic Alzheimer’s disease: a hypothesis. Acta Neuropathol 126:303–306. doi:10.1007/s00401-013-1153-2
Braak H, Del Tredici K (2015) The preclinical phase of the pathological process underlying sporadic Alzheimer’s disease. Brain 138:2814–2833. doi:10.1093/brain/awv236
Bright J, Hussain S, Dang V, Wright S, Cooper B, Byun T et al (2015) Human secreted tau increases amyloid-beta production. Neurobiol Aging 36:693–709. doi:10.1016/j.neurobiolaging.2014.09.007
Calhoun ME, Wiederhold KH, Abramowski D, Phinney AL, Probst A, Sturchler-Pierrat C et al (1998) Neuron loss in APP transgenic mice. Nature 395:755–756. doi:10.1038/27351
Carare RO, Hawkes CA, Jeffrey M, Kalaria RN, Weller RO (2013) Cerebral amyloid angiopathy, prion angiopathy, CADASIL and the spectrum of protein elimination failure angiopathies (PEFA) in neurodegenerative disease with a focus on therapy. Neuropathol Appl Neurobiol 39:593–611. doi:10.1111/nan.12042
Do Carmo S, Cuello AC (2013) Modeling Alzheimer’s disease in transgenic rats. Mol Neurodegener 8:37. doi:10.1186/1750-1326-8-37
van Cauwenberghe C, Van Broeckhoven C, Sleegers K (2015) The genetic landscape of Alzheimer disease: clinical implications and perspectives. Genet Med. doi:10.1038/gim.2015.117
Chávez-Gutiérrez L, Bammens L, Benilova I, Vandersteen A, Benurwar M, Borgers M et al (2012) The mechanism of γ-Secretase dysfunction in familial Alzheimer disease. EMBO J 31:2261–2274. doi:10.1038/emboj.2012.79
Cheng IH, Scearce-Levie K, Legleiter J, Palop JJ, Gerstein H, Bien-Ly N et al (2007) Accelerating amyloid-beta fibrillization reduces oligomer levels and functional deficits in Alzheimer disease mouse models. J Biol Chem 282:23818–23828. doi:10.1074/jbc.M701078200
Chin J (2011) Selecting a mouse model of Alzheimer’s disease. Methods Mol Biol 670:169–189. doi:10.1007/978-1-60761-744-0_13
Chiti F, Dobson CM (2006) Protein misfolding, functional amyloid, and human disease. Annu Rev Biochem 75:333–366. doi:10.1146/annurev.biochem.75.101304.123901
Cirrito JR, May PC, O’Dell M, Taylor JW, Parsadanian M, Cramer JW et al (2003) In vivo assessment of brain interstitial fluid with microdialysis reveals plaque-associated changes in amyloid-beta metabolism and half-life. J Neurosci 23:8844–8853. doi:10.1186/1750-1326-8-13
Cole G, Neal JW, Singhrao SK, Jasani B, Newman GR (1993) The distribution of amyloid plaques in the cerebellum and brain stem in Down’s syndrome and Alzheimer’s disease: a light microscopical analysis. Acta Neuropathol 85:542–552. doi:10.1007/BF00230495
Cox B, Ness F, Tuite M (2003) Analysis of the generation and segregation of propagons: entities that propagate the [PSI+] prion in yeast. Genetics 165:23–33
Crimins JL, Rocher AB, Luebke JI (2012) Electrophysiological changes precede morphological changes to frontal cortical pyramidal neurons in the rTg4510 mouse model of progressive tauopathy. Acta Neuropathol 124:777–795. doi:10.1007/s00401-012-1038-9
Cummings BJ, Satou T, Head E, Milgram NW, Cole GM, Savage MJ et al (1996) Diffuse plaques contain C-terminal A beta 42 and not A beta 40: evidence from cats and dogs. Neurobiol Aging 17:653–659
Delaère P, Duyckaerts C, He Y, Pierre F, Hauw JJ (1991) Subtypes and differential laminar distributions of βA4 deposits in Alzheimer’s disease: relationship with the intellectual status of 26 cases. Acta Neuropathol 81:328–335
Delaère P, Duyckaerts C, Masters C, Beyreuther K, Piette F, Hauw JJ (1990) Large amounts of neocortical beta A4 deposits without neuritic plaques nor tangles in a psychometrically assessed, non-demented person. Neurosci Lett 116:87–93
Dickson DW, Crystal HA, Mattiace LA, Masur DM, Blau AD, Davies P et al (1992) Identification of normal and pathological aging in prospectively studied nondemented elderly humans. Neurobiol Aging 13:179–189
Duyckaerts C, Colle M-A, Seilhean D, Hauw J-J (1998) Laminar spongiosis of the dentate gyrus: a sign of disconnection, present in cases of severe Alzheimer’s disease. Acta Neuropathol 95:413–420. doi:10.1007/s004010050818
Duyckaerts C, Delatour B, Potier M-C (2009) Classification and basic pathology of Alzheimer disease. Acta Neuropathol 118:5–36. doi:10.1007/s00401-009-0532-1
Duyckaerts C, Hauw J-J (1997) Prevalence, incidence and duration of Braak’s stages in the general population: can we know? Neurobiol Aging 18:362–369
Duyckaerts C, Uchihara T, Seilhean D, He Y, Hauw JJ (1997) Dissociation of Alzheimer type pathology in a disconnected piece of cortex. Acta Neuropathol 93:501–507
Eisele YS, Bolmont T, Heikenwalder M, Langer F, Jacobson LH, Yan Z-XX et al (2009) Induction of cerebral beta-amyloidosis: intracerebral versus systemic Abeta inoculation. Proc Natl Acad Sci USA 106:12926–12931. doi:10.1073/pnas.0903200106
Eisele YS, Fritschi SK, Hamaguchi T, Obermüller U, Füger P, Skodras A et al (2014) Multiple factors contribute to the peripheral induction of cerebral β-amyloidosis. J Neurosci 34:10264–10273. doi:10.1523/JNEUROSCI.1608-14.2014
Eisele YS, Monteiro C, Fearns C, Encalada SE, Wiseman RL, Powers ET et al (2015) Targeting protein aggregation for the treatment of degenerative diseases. Nat Rev Drug Discov. doi:10.1038/nrd4593
Eisele YS, Obermüller U, Heilbronner G, Baumann F, Kaeser SA, Wolburg H et al (2010) Peripherally applied Abeta-containing inoculates induce cerebral beta-amyloidosis. Science 330:980–982. doi:10.1126/science.1194516
Epelbaum S, Youssef I, Lacor P, Chaurand P, Duplus E, Brugg B et al (2015) Acute amnestic encephalopathy in amyloid-ß oligomers injected mice is due to their widespread diffusion in vivo. Neurobiol Aging 36:2043–2052. doi:10.1016/j.neurobiolaging.2015.03.005
Fritschi SK, Cintron A, Ye L, Mahler J, Buhler A, Baumann F et al (2014) Abeta seeds resist inactivation by formaldehyde. Acta Neuropathol 128:477–484. doi:10.1007/s00401-014-1339-2
Fritschi SK, Langer F, Kaeser SA, Maia LF, Portelius E, Pinotsi D et al (2014) Highly potent soluble amyloid-beta seeds in human Alzheimer brain but not cerebrospinal fluid. Brain 137:2909–2915. doi:10.1093/brain/awu255
George S, Ronnback A, Gouras GK, Petit GH, Grueninger F, Winblad B et al (2014) Lesion of the subiculum reduces the spread of amyloid beta pathology to interconnected brain regions in a mouse model of Alzheimer’s disease. Acta Neuropathol Commun 2:17. doi:10.1186/2051-5960-2-17
German DC, White CL, Sparkman DR (1987) Alzheimer’s disease: neurofibrillary changes in nuclei that project to the cerebral cortex. Neuroscience 21:305–312
Ghetti B, Oblak AL, Boeve BF, Johnson KA, Dickerson BC, Goedert M (2015) Invited review: frontotemporal dementia caused by microtubule-associated protein tau gene (MAPT) mutations: a chameleon for neuropathology and neuroimaging. Neuropathol Appl Neurobiol 41:24–46. doi:10.1111/nan.12213
Gotz J, Chen F, van Dorpe J, Nitsch RM, Götz J, Chen F et al (2001) Formation of neurofibrillary tangles in P301 l tau transgenic mice induced by Abeta 42 fibrils. Science (80-) 293:1491–1495. doi: 10.1126/science.1062097
Gouras GK, Willén K, Tampellini D (2012) Critical role of intraneuronal Aβ in Alzheimer’s disease: technical challenges in studying intracellular Aβ. Life Sci 91:1153–1158. doi:10.1016/j.lfs.2012.06.004
Grinberg LT, Rüb U, Ferretti REL, Nitrini R, Farfel JM, Polichiso L et al (2009) The dorsal raphe nucleus shows phospho-tau neurofibrillary changes before the transentorhinal region in Alzheimer’s disease. A precocious onset? Neuropathol Appl Neurobiol 35:406–416. doi:10.1111/j.1365-2990.2009.00997.x
Haass C, Kaether C, Thinakaran G, Sisodia S (2012) Trafficking and proteolytic processing of APP. Cold Spring Harb Perspect Med 2:a006270. doi:10.1101/cshperspect.a006270
Hamaguchi T, Eisele YS, Varvel NH, Lamb BT, Walker LC, Jucker M (2012) The presence of Abeta seeds, and not age per se, is critical to the initiation of Abeta deposition in the brain. Acta Neuropathol 123:31–37. doi:10.1007/s00401-011-0912-1
Hardy JA, Higgins GA (1992) Alzheimer’ s Disease: The Amyloid Cascade Hypothesis. Science (80-) 256:184–185
Harper JD, Lansbury PT Jr (1997) Models of amyloid seeding in Alzheimer’s disease and scrapie: mechanistic truths and physiological consequences of the time-dependent solubility of amyloid proteins. Annu Rev Biochem 66:385–407. doi:10.1146/annurev.biochem.66.1.385
Heilbronner G, Eisele YS, Langer F, Kaeser SA, Novotny R, Nagarathinam A et al (2013) Seeded strain-like transmission of β-amyloid morphotypes in APP transgenic mice. EMBO Rep 14:1017–1022. doi:10.1038/embor.2013.137
Héraud C, Goufak D, Ando K, Leroy K, Suain V, Yilmaz Z et al (2013) Increased misfolding and truncation of tau in APP/PS1/tau transgenic mice compared to mutant tau mice. Neurobiol Dis 62:100–112. doi:10.1016/j.nbd.2013.09.010
Herzig MC, Van Nostrand WE, Jucker M (2006) Mechanism of cerebral beta-amyloid angiopathy: murine and cellular models. Brain Pathol 16:40–54
Herzig MC, Winkler DT, Burgermeister P, Pfeifer M, Kohler E, Schmidt SD et al (2004) Abeta is targeted to the vasculature in a mouse model of hereditary cerebral hemorrhage with amyloidosis. Nat Neurosci 7:954–960. doi:10.1038/nn1302
Heuer E, Rosen RF, Cintron A, Walker LC (2012) Nonhuman primate models of Alzheimer-like cerebral proteopathy. Curr Pharm Des 18:1159–1169
Hooli BV, Mohapatra G, Mattheisen M, Parrado AR, Roehr JT, Shen Y et al (2012) Role of common and rare APP DNA sequence variants in Alzheimer disease. Neurology 78:1250–1257. doi:10.1212/WNL.0b013e3182515972
Hsiao K, Chapman P, Nilsen S, Eckman C, Harigaya Y, Younkin S et al (1996) Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice. Science (80-) 274:99–102
Hyman BT, Van Hoesen GW, Beyreuther K, Masters CL (1989) A4 amyloid protein immunoreactivity is present in Alzheimer’s disease neurofibrillary tangles. Neurosci Lett 101:352–355
Hyman BT, Van Hoesen GW, Damasio AR, Barnes CL (1984) Alzheimer’s disease: cell-specific pathology isolates the hippocampal formation. Science (80-) 225:1168–70
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC et al (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement 8:1–13. doi:10.1016/j.jalz.2011.10.007
Irwin DJ, Abrams JY, Schonberger LB, Leschek W, Mills JL, Lee VM et al (2013) Evaluation of potential infectivity of Alzheimer and Parkinson disease proteins in recipients of cadaver-derived human growth hormone. JAMA Neurol 70:462–468. doi:10.1001/jamaneurol.2013.1933.Evaluation
Jack CR, Jorge J, Vladimir RB (2013) Cerebral amyloid PET imaging in Alzheimer’ s disease. Acta Neuropathol 126:643–657. doi: 10.1007/s00401-013-1185-7
Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FR et al (2015) Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA 313:1924–1938. doi:10.1001/jama.2015.4668
Jarrett JT, Berger EP, Lansbury PT (1993) The carboxy terminus of the beta-amyloid protein is critical for the seeding of amyloid formation: implications for the pathogenesis of Alzheimer’s disease. Biochemistry 32:4693–4697. doi:10.1021/bi00069a001
Jarrett JT, Lansbury PT (1993) Seeding “one-dimensional crystallization” of amyloid: a pathogenic mechanism in Alzheimer’s disease and scrapie? Cell 73:1055–1058. doi:10.1016/0092-8674(93)90635-4
Jaunmuktane Z, Mead S, Ellis M, Wadsworth JDF, Nicoll AJ, Kenny J et al (2015) Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy. Nature 525:247–250. doi:10.1038/nature15369
Jucker M, Walker LC (2011) Pathogenic protein seeding in Alzheimer disease and other neurodegenerative disorders. Ann Neurol 70:532–540. doi:10.1002/ana.22615
Kane MD, Lipinski WJ, Callahan MJ, Bian F, Durham RA, Schwarz RD et al (2000) Evidence for seeding of beta -amyloid by intracerebral infusion of Alzheimer brain extracts in beta-amyloid precursor protein transgenic mice. J Neurosci 20:3606–3611
Kanmert D, Cantlon A, Muratore CR, Jin M, O’Malley TT, Lee G et al (2015) C-terminally truncated forms of tau, but not full-length tau or its C-terminal fragments, are released from neurons independently of cell death. J Neurosci 35:10851–10865. doi:10.1523/JNEUROSCI.0387-15.2015
Kelly PH, Bondolfi L, Hunziker D, Schlecht HP, Carver K, Maguire E et al (2003) Progressive age-related impairment of cognitive behavior in APP23 transgenic mice. Neurobiol Aging 24:365–378
Kovacs GG (2015) Invited review: neuropathology of tauopathies: principles and practice. Neuropathol Appl Neurobiol 41:3–23. doi:10.1111/nan.12208
Kuchibhotla KV, Wegmann S, Kopeikina KJ, Hawkes J, Rudinskiy N, Andermann ML et al (2014) Neurofibrillary tangle-bearing neurons are functionally integrated in cortical circuits in vivo. Proc Natl Acad Sci USA 111:510–514. doi:10.1073/pnas.1318807111
Kuo YM, Emmerling MR, Vigo-Pelfrey C, Kasunic TC, Kirkpatrick JB, Murdoch GH et al (1996) Water-soluble Abeta (N-40, N-42) oligomers in normal and Alzheimer disease brains. J Biol Chem 271:4077–4081
De Lacoste MC, White CL (1993) The role of connectivity in Alzheimer’s disease pathogenesis. A review and model system. Neurobiol Aging 14:1–16
Lamb BT, Call LM, Slunt HH, Bardel KA, Lawler AM, Eckman CB et al (1997) Altered metabolism of familial Alzheimer’s disease-linked amyloid precursor protein variants in yeast artificial chromosome transgenic mice. Hum Mol Genet 6:1535–1541
Langer F, Eisele YS, Fritschi SK, Staufenbiel M, Walker LC, Jucker M (2011) Soluble Abeta seeds are potent inducers of cerebral beta-amyloid deposition. J Neurosci 31:14488–14495. doi:10.1523/JNEUROSCI.3088-11.2011
Le TV, Crook R, Hardy J, Dickson DW (2001) Cotton wool plaques in non-familial late-onset Alzheimer disease. J Neuropathol Exp Neurol 60:1051–1061
Lévesque M, Parent A (2005) The striatofugal fiber system in primates: a reevaluation of its organization based on single-axon tracing studies. Proc Natl Acad Sci USA 102:11888–11893. doi:10.1073/pnas.0502710102
Lewis J, Dickson DW (2016) Propagation of tau pathology: hypotheses, discoveries, and yet unresolved questions from experimental and human brain studies. Acta Neuropathol. doi:10.1007/s00401-015-1507-z
Lorenzo A, Yankner BA (1994) Beta-amyloid neurotoxicity requires fibril formation and is inhibited by congo red. Proc Natl Acad Sci USA 91:12243–12247
Maia LF, Kaeser SA, Reichwald J, Hruscha M, Martus P, Staufenbiel M et al (2013) Changes in amyloid-beta and Tau in the cerebrospinal fluid of transgenic mice overexpressing amyloid precursor protein. Sci Transl Med 5:194re2. doi:10.1126/scitranslmed.3006446
Mann DMA, Esiri MM (1989) The pattern of acquisition of plaques and tangles in the brains of patients under 50 years of age with Down’s syndrome. J Neurol Sci 89:169–179
Mann DMA, Hardy J (2013) Amyloid or tau: the chicken or the egg? Acta Neuropathol 126:609–613. doi:10.1007/s00401-013-1162-1
McGowan E, Pickford F, Kim J, Onstead L, Eriksen J, Yu C et al (2005) Abeta42 is essential for parenchymal and vascular amyloid deposition in mice. Neuron 47:191–199. doi:10.1016/j.neuron.2005.06.030
McLean CA, Cherny RA, Fraser FW, Fuller SJ, Smith MJ, Beyreuther K et al (1999) Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer’s disease. Ann Neurol 46:860–866
Metsaars W, Hauw J-J, Welsem M, Duyckaerts C (2003) A grading system of Alzheimer disease lesions in neocortical areas. Neurobiol Aging 24:563–572
Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E et al (2006) Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science 313:1781–1784. doi:10.1126/science.1131864
Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A et al (2008) Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer’s disease. Nature 451:720–724. doi:10.1038/nature06616
Meyer-Luehmann M, Stalder M, Herzig MC, Kaeser SA, Kohler E, Pfeifer M et al (2003) Extracellular amyloid formation and associated pathology in neural grafts. Nat Neurosci 6:370–377. doi:10.1038/nn1022
Mucke L, Masliah E, Yu GQ, Mallory M, Rockenstein EM, Tatsuno G et al (2000) High-level neuronal expression of abeta 1–42 in wild-type human amyloid protein precursor transgenic mice: synaptotoxicity without plaque formation. J Neurosci 20:4050–4058
Murakami T, Ishiguro N, Higuchi K (2014) Transmission of systemic AA amyloidosis in animals. Vet Pathol 51:363–371. doi:10.1177/0300985813511128
Musiek ES, Holtzman DM (2015) Three dimensions of the amyloid hypothesis: time, space and “wingmen”. Nat Neurosci 18:800–806. doi:10.1038/nn.4018
Oddo S, Billings L, Kesslak JP, Cribbs DH, LaFerla FM (2004) Abeta immunotherapy leads to clearance of early, but not late, hyperphosphorylated tau aggregates via the proteasome. Neuron 43:321–332. doi:10.1016/j.neuron.2004.07.003
Oddo S, Caccamo A, Shepherd JD, Murphy MP, Golde TE, Kayed R et al (2003) Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Abeta and synaptic dysfunction. Neuron 39:409–421
Ossenkoppele R, Jansen WJ, Rabinovici GD, Knol DL, van der Flier WM, van Berckel BN et al (2015) Prevalence of amyloid PET positivity in dementia syndromes: a meta-analysis. JAMA 313:1939–1949. doi:10.1001/jama.2015.4669
Patterson BW, Elbert DL, Mawuenyega KG, Kasten T, Ovod V, Ma S et al (2015) Age and amyloid effects on human central nervous system amyloid-beta kinetics. Ann Neurol 78:439–453. doi:10.1002/ana.24454
Perez SE, Raghanti MA, Hof PR, Kramer L, Ikonomovic MD, Lacor PN et al (2013) Alzheimer’s disease pathology in the neocortex and hippocampus of the western lowland gorilla (Gorilla gorilla gorilla). J Comp Neurol 521:4318–4338. doi:10.1002/cne.23428
Petkova AT, Leapman RD, Guo Z, Yau WM, Mattson MP, Tycko R (2005) Self-propagating, molecular-level polymorphism in Alzheimer’s beta-amyloid fibrils. Science (80-) 307:262–265. doi: 10.1126/science.1105850
Pooler AM, Phillips EC, Lau DHW, Noble W, Hanger DP (2013) Physiological release of endogenous tau is stimulated by neuronal activity. EMBO Rep 14:389–394. doi:10.1038/embor.2013.15
Pooler AM, Polydoro M, Maury EA, Nicholls SB, Reddy SM, Wegmann S et al (2015) Amyloid accelerates tau propagation and toxicity in a model of early Alzheimer’ s disease. Acta Neuropathol Commun 3:1–11. doi:10.1186/s40478-015-0199-x
Prusiner SB (1982) Novel proteinaceous infectious particles cause scrapie. Science (80-) 216:136–144
Radde R, Duma C, Goedert M, Jucker M (2008) The value of incomplete mouse models of Alzheimer’s disease. Eur J Nucl Med Mol Imaging 35(Suppl 1):S70–S74
Roberson ED, Scearce-Levie K, Palop JJ, Yan F, Cheng IH, Wu T et al (2007) Reducing endogenous Tau ameliorates amyloid beta–Induced deficits in an Alzheimer’s disease mouse model. Science (80-) 316:750–754
Ronnback A, Sagelius H, Bergstedt KD, Naslund J, Westermark GT, Winblad B et al (2012) Amyloid neuropathology in the single Arctic APP transgenic model affects interconnected brain regions. Neurobiol Aging 33:831.e11–831.e19. doi: 10.1016/j.neurobiolaging.2011.07.012
Rovelet-Lecrux A, Hannequin D, Raux G, Le Meur N, Laquerriere A, Vital A et al (2006) APP locus duplication causes autosomal dominant early-onset Alzheimer disease with cerebral amyloid angiopathy. Nat Genet 38:24–26
Rupp NJ, Wegenast-Braun BM, Radde R, Calhoun ME, Jucker M (2011) Early onset amyloid lesions lead to severe neuritic abnormalities and local, but not global neuron loss in APPPS1 transgenic mice. Neurobiol Aging 32:2324.e1–2324.e6. doi: 10.1016/j.neurobiolaging.2010.08.014
Saito T, Matsuba Y, Mihira N, Takano J, Nilsson P, Itohara S et al (2014) Single APP knock-in mouse models of Alzheimer’s disease. Nat Neurosci 17:661–663. doi:10.1038/nn.3697
Saito T, Suemoto T, Brouwers N, Sleegers K, Funamoto S, Mihira N et al (2011) Potent amyloidogenicity and pathogenicity of Aβ43. Nat Neurosci 14:1023–1032. doi:10.1038/nn.2858
Schmidt ML, Lee VM, Trojanowski JQ (1991) Comparative epitope analysis of neuronal cytoskeletal proteins in Alzheimer’s disease senile plaque, neurites and neuropil threads. Lab Invest 64:352–357
Schneider K, Fangerau H, Michaelsen B, Raab WH-M (2008) The early history of the transmissible spongiform encephalopathies exemplified by scrapie. Brain Res Bull 77:343–355. doi:10.1016/j.brainresbull.2008.09.012
Schwab C, Steele JC, Akiyama H, McGeer EG, McGeer PL (1995) Relationship of amyloid β/A4 protein to the neurofibrillary tangles in Guamanian parkinsonism-dementia. Acta Neuropathol 90:287–298. doi:10.1007/BF00296513
Selkoe DJ, Bell DS, Podlisny MB, Price DL, Cork LC (1987) Conservation of brain amyloid proteins in aged mammals and humans with Alzheimer’s disease. Science (80-) 235:873–877
Sipe JD, Benson MD, Buxbaum JN, Ikeda S, Merlini G, Saraiva MJM et al (2014) Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid 21:221–224. doi:10.3109/13506129.2014.964858
Soto C (2003) Unfolding the role of protein misfolding in neurodegenerative diseases. Nat Rev Neurosci 4:49–60. doi:10.1038/nrn1007
St George-Hyslop PH (2000) Molecular genetics of Alzheimer’s disease. Biol Psychiatry 47:183–199
Stohr J, Condello C, Watts JC, Bloch L, Oehler A, Nick M et al (2014) Distinct synthetic Abeta prion strains producing different amyloid deposits in bigenic mice. Proc Natl Acad Sci USA 111:10329–10334. doi:10.1073/pnas.1408968111
Sturchler-Pierrat C, Abramowski D, Duke M, Wiederhold KH, Mistl C, Rothacher S et al (1997) Two amyloid precursor protein transgenic mouse models with Alzheimer disease-like pathology. Proc Natl Acad Sci USA 94:13287–13292
Takami M, Nagashima Y, Sano Y, Ishihara S, Morishima-Kawashima M, Funamoto S et al (2009) Gamma-Secretase: successive tripeptide and tetrapeptide release from the transmembrane domain of beta-carboxyl terminal fragment. J Neurosci 29:13042–13052. doi:10.1523/JNEUROSCI.2362-09.2009
Thal DR, Ghebremedhin E, Orantes M, Wiestler OD (2003) Vascular pathology in Alzheimer disease: correlation of cerebral amyloid angiopathy and arteriosclerosis/lipohyalinosis with cognitive decline. J Neuropathol Exp Neurol 62:1287–1301
Thal DR, Rüb U, Orantes M, Braak H (2002) Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology 58:1791–1800
Thal DR, Walter J, Saido TC, Fändrich M (2015) Neuropathology and biochemistry of Aβ and its aggregates in Alzheimer’s disease. Acta Neuropathol 129:167–182. doi:10.1007/s00401-014-1375-y
Vassar R, Kuhn P-H, Haass C, Kennedy ME, Rajendran L, Wong PC et al (2014) Function, therapeutic potential and cell biology of BACE proteases: current status and future prospects. J Neurochem 130:4–28. doi:10.1111/jnc.12715
Vlassenko AG, Mintun MA, Xiong C, Sheline YI, Goate AM, Benzinger TLS et al (2011) Amyloid-beta plaque growth in cognitively normal adults: longitudinal [11C] Pittsburgh compound B data. Ann Neurol 70:857–861. doi:10.1002/ana.22608
Walker LC, Bian F, Callahan MJ, Lipinski WJ, Durham RA, LeVine H (2002) Modeling Alzheimer’s disease and other proteopathies in vivo: is seeding the key? Amino Acids 23:87–93. doi:10.1007/s00726-001-0113-7
Walker LC, Callahan MJ, Bian F, Durham RZ, Roher AE, Lipinski WJ (2002) Exogenous induction of cerebral beta-amyloidosis in betaAPP-transgenic mice. Peptides 23:1241–1247
Walsh DM, Hartley DM, Kusumoto Y, Fezoui Y, Condron MM, Lomakin A et al (1999) Amyloid beta-protein fibrillogenesis. Structure and biological activity of protofibrillar intermediates. J Biol Chem 274:25945–25952
Walsh DM, Selkoe DJ (2007) A beta oligomers: a decade of discovery. J Neurochem 101:1172–1184
Watts JC, Condello C, Stohr J, Oehler A, Lee J, DeArmond SJ et al (2014) Serial propagation of distinct strains of Abeta prions from Alzheimer’s disease patients. Proc Natl Acad Sci USA 111:10323–10328. doi:10.1073/pnas.1408900111
Westerman MA, Cooper-Blacketer D, Mariash A, Kotilinek L, Kawarabayashi T, Younkin LH et al (2002) The relationship between Abeta and memory in the Tg2576 mouse model of Alzheimer’s disease. J Neurosci 22:1858–1867
Willem M, Tahirovic S, Busche MA, Ovsepian SV, Chafai M, Kootar S et al (2015) η-Secretase processing of APP inhibits neuronal activity in the hippocampus. Nature 526:443–447. doi:10.1038/nature14864
Wiseman FK, Al-Janabi T, Hardy J, Karmiloff-Smith A, Nizetic D, Tybulewicz VLJ et al (2015) A genetic cause of Alzheimer disease: mechanistic insights from Down syndrome. Nat Rev Neurosci 16:564–574. doi:10.1038/nrn3983
Xiao Y, Ma B, McElheny D, Parthasarathy S, Long F, Hoshi M et al (2015) Aβ(1–42) fibril structure illuminates self-recognition and replication of amyloid in Alzheimer’s disease. Nat Struct Mol Biol 22:499–505. doi:10.1038/nsmb.2991
Ye L, Fritschi SK, Schelle J, Obermüller U, Degenhardt K, Kaeser SA et al (2015) Persistence of Aβ seeds in APP null mouse brain. Nat Neurosci 18:1559–1561. doi:10.1038/nn.4117
Ye L, Hamaguchi T, Fritschi SK, Eisele YS, Obermuller U, Jucker M et al (2015) Progression of seed-induced abeta deposition within the limbic connectome. Brain Pathol 25:743–752. doi:10.1111/bpa.12252
Yetman MJ, Lillehaug S, Bjaalie JG, Leergaard TB, Jankowsky JL (2015) Transgene expression in the Nop-tTA driver line is not inherently restricted to the entorhinal cortex. Brain Struct Funct. doi:10.1007/s00429-015-1040-9
Acknowledgments
YSE is supported by a postdoctoral fellowship from the German Academic Exchange Service (DAAD). CD thanks Benoît Delatour, Marie-Claude Potier, Manon Thierry, the members of the Alzheimer-Prion team for useful discussions. Neuropathological studies of AD cases have been made possible thanks to the Brain Bank GIE NeuroCEB funded by the patients’ Associations France Alzheimer, France Parkinson, Foundation ARSEP, Comprendre les Syndromes Cérébelleux, IHU A-ICM and Fondation Plan Alzheimer. We are grateful to the patients and to their families. The help of Foundation Claude Pompidou and IHU A-ICM is also greatly acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Eisele, Y.S., Duyckaerts, C. Propagation of Aß pathology: hypotheses, discoveries, and yet unresolved questions from experimental and human brain studies. Acta Neuropathol 131, 5–25 (2016). https://doi.org/10.1007/s00401-015-1516-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-015-1516-y