Abstract
Enhanced reactive oxygen species (ROS) at the beginning of reperfusion activated signal transducer and activator of transcription 3 (STAT3) in intermittent hypobaric hypoxia (IHH)-afforded cardioprotection against ischemia/reperfusion (I/R). However, its mechanism remains largely unknown. This study aimed to investigate the role and the downstream of STAT3 in exogenous enhanced post-ischemic ROS-induced cardioprotection using the model of moderate hydrogen peroxide postconditioning (H2O2PoC) mimicking endogenous ROS in IHH. Moderate H2O2PoC not only improved the post-ischemic myocardial contractile recovery and reduced the infarct size in isolated rat I/R hearts, but also alleviated mitochondrial calcium overload and ameliorated Ca2+ transients, cell contraction, and mitochondrial membrane potential in rat I/R cardiomyocytes. However, the cardioprotective effects of moderate H2O2PoC were abrogated by Janus kinase 2 (JAK2)/STAT3 inhibitor AG490 in rat hearts as well as adenovirus-delivered short hairpin RNA specific for STAT3 and the opener of mitochondrial calcium uniporter (MCU) spermine in rat cardiomyocytes. Notably, the moderate H2O2PoC-afforded cardioprotection abrogated by spermine could be rescued by STAT3 over-expression with adenovirus in rat I/R cardiomyocytes. Besides, moderate H2O2PoC enhanced mitochondrial STAT3 expression during I/R. A co-localization/interaction of STAT3 or phospho-STAT3ser727 and MCU was observed in rat cardiomyocytes with moderate H2O2PoC at 5 and 30 min of reperfusion but not in rat I/R cardiomyocytes. Further, STAT3 interacted with the N-terminal domain (NTD) of MCU in rat cardiomyocytes with moderate H2O2PoC. These findings indicated that post-ischemic moderate ROS activate STAT3 against cardiac I/R by inhibiting MCU opening via its interaction with the NTD of MCU to alleviate mitochondrial calcium overload.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial ischemia/reperfusion (I/R) injury is the common clinical manifestation of the pathological scenario of ischemic heart disease. Myocardial contractile dysfunction due to I/R is partly incited by calcium overload [9]. Calcium overload in myocytes, including mitochondrial [Ca2+]m and cytosolic free calcium concentration [Ca2+]c overload, is especially considered as one of the primary elements resulting in cardiac I/R injury [44]. [Ca2+]m overload has been proved to be the cause of [Ca2+]c overload and contractile dysfunction [10, 15]. Thus, the reduction of [Ca2+]m overload is an essential way to achieve cardioprotection. During myocardial I/R, mitochondrial calcium uniporter (MCU) selectively transport significant amounts of calcium from the cytosol into mitochondria [14]. The observations show that MCU serves as an important ion channel in the regulation of [Ca2+]m overload, such as treatment with MCU inhibitor Ru360 decreasing [Ca2+]m overload in cardiac I/R [13], small interfering RNA targeting MCU reducing [Ca2+]m overload in cardiomyocytes [40] and conditional cardiac-specific MCU−/− mice subjected to I/R resulting in a significant reduction of [Ca2+]m overload [27]. However, the regulatory mechanism of MCU during cardiac I/R injury and cardioprotection remains unveiled.
Reactive oxygen species (ROS) production during early reperfusion should reach a threshold to trigger the ischemic preconditioning (IPC)-, ischemic postconditioning (IPoC)-, remote ischemic preconditioning (RIPC)- and intermittent hypobaric hypoxia (IHH) adaptation-induced cardioprotection [20, 42, 52, 53]. Meanwhile, ROS generated inadequately or excessively during early reperfusion are main factors of I/R injury [4, 53]. The stable form of ROS is hydrogen peroxide (H2O2) [4]. It has been found that moderate concentrations of H2O2 postconditioning (H2O2PoC), a model of enhanced ROS at early reperfusion in an exogenous manner, significantly promote post-ischemic left ventricular (LV) contractile recovery [53]. Besides, moderate H2O2 preconditioning alleviates calcium paradox in hearts and cardiomyocytes [12, 37]. However, whether moderate H2O2PoC protects the hearts and cardiomyocytes from calcium overload and contractile dysfunction due to I/R remains elusive. Although the inhibition of MCU seems to play a crucial role in IPC and IPoC [57, 60], whether moderate H2O2PoC can reduce calcium overload and improve cardiac contraction via inhibiting MCU is unknown.
Signal transducer and the activator of transcription 3 (STAT3) is a significant protein contributing to the signal transduction of cardioprotection [5, 18, 55]. Not only STAT3 acts as a transcription factor in the nucleus with its phosphorylation at tyrosine 705 and serine 727 for regulating gene transcription [3, 39, 41], but also STAT3 phosphorylated at tyrosine 705 (pY-STAT3) and serine727 (pS-STAT3) is required in the mitochondria for its fast cardioprotective effect in pig and mouse [6, 22, 23, 25]. Endogenous enhanced ROS in IHH can activate STAT3 during early reperfusion via improving postischemic sarcoplasmic reticulum (SR) Ca2+-ATPase (SERCA2) activity through increasing SR B cell lymphoma-2 (Bcl-2), which interacts with SERCA2 and maintains mitochondrial function [55]. However, whether STAT3 preserves mitochondrial function in moderate H2O2PoC is still unknown. Tumor necrosis factor-alpha (TNF-α) preconditioning only activates STAT3 during reperfusion [29] or inhibits the opening of MCU [16] to achieve cardioprotection in isolated rat I/R hearts, nevertheless, whether activated STAT3 in moderate H2O2PoC can alleviate myocyte calcium overload and improve cardiac contractile via inhibiting MCU against cardiac I/R insult is unclear.
To address the aforementioned issues, a model of moderate H2O2PoC was designed to examine (1) the effects of post-ischemic moderate ROS on [Ca2+]c in myoctes, [Ca2+]m in myocytes, mitochondrial membrane potential, Ca2+ transients, and myocytes contractile during I/R; (2) the role of STAT3 in post-ischemic moderate ROS-induced cardioprotection; (3) the role of MCU in post-ischemic moderate ROS-induced cardioprotection; (4) the correlation of STAT3 with MCU and its role in post-ischemic moderate ROS-induced cardioprotection; and (5) the molecular mechanism of action of STAT3 on MCU in post-ischemic moderate ROS-induced cardioprotection.
Methods
Animals
In this study, adult male Sprague–Dawley (SD) rats (Shanghai Slac Laboratory Animal Co. Ltd.) were used according to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication, 8th Edition, 2011) and animal procedures approved by the Institutional Review Board of Shanghai University of Medicine & Health Sciences (Shanghai, China). The weight of rats was from 280 to 320 g.
Langendorff-perfused rat I/R hearts
Sodium pentobarbital (50 mg/kg i.p.) was used to anesthetize the rats. The hearts were rapidly isolated from the rats and mounted on the Langendorff apparatus with the Krebs–Henseleit solution at 37 °C as previously described [12, 32]. The pressure transducer (Gould P23Db, AD Instrument, New South Wales, Australia) was coupled to a fluid-filled balloon and we inserted it into the LV cavity. After LV end-diastolic pressure (LVEDP) was maintained at 5–10 mmHg by inflating the balloon, the isolated heart was put onto the Langendorff system with global non-flow I/R (30-min/45-min). The PowerLab system (AD Instrument, New South Wales, Australia) was used to evaluate LV developed pressure (LVDP), LVEDP, maximum rates of pressure development or decay over time (± dP/dt max) and heart rate (HR). H2O2 (20 μmol/L, Merck, Darmstadt, Germany) [53] and AG490 (20 μmol/L, Merck, Darmstadt, Germany), a Janus kinase 2 (JAK2)/STAT3 inhibitor, were used at the beginning of reperfusion for 5 min (Online Fig. 1a).
Infarct size estimation
The isolated rat hearts were subjected to global non-flow I/R (30-min/2-h), following which they were frozen the hearts and cut LV into 2-mm-thick slices. Subsequently, 1% (w/v) triphenyltetrazolium chloride (phosphate buffer, pH 7.4) was used to stain the slices and used 10% formaldehyde to fix them [8, 31, 52, 61]. Image-Pro Plus software (Media Cybernetics, Maryland, USA) was used to calculate the infarct size and the infarct area was expressed as a percentage of the LV area at risk.
Construction of recombinant adenoviruses
Recombinant adenoviruses expressing rat STAT3 (AdSTAT3), short hairpin RNA of STAT3 (AdSTAT3shRNA), rat Flag-MCU (AdFlag-MCU WT), rat Flag-MCU with N-terminal domain (NTD) deletion (AdFlag-MCUΔ75–165), vector (AdVector) and short hairpin RNA of scramble (AdScramble) were prepared as described previously [32] using the pHBAd vector system (Hanbio, Shanghai, China). The detailed method is available in Supplementary materials online.
Isolation, culture, and adenoviral infection of myocytes
A standard method was used to isolate and culture LV myocytes as previously described [11, 32]. Then, the LV myocytes were infected with recombinant adenoviruses. The detailed method is available in Supplementary materials online.
Simulated I/R in isolated cardiomyocytes
A simulated I/R (20-min/30-min) model in isolated cardiomyocytes was set up as previously described [11, 15]. First, the myocytes were perfused in the modified Krebs–Henseleit solution (35 °C, pH 7.4) and then in ischemic solution, containing (mmol/L): NaCl, 123.0; KCl, 8.0; NaHCO3, 6.0; NaH2PO4, 0.9; MgSO4, 0.5; Na-lactate, 20.0; and CaCl2, 1.8, gassed with 95% N2/5% CO2, (pH 6.8) for 20 min. Finally, they were reperfused in the modified Krebs–Henseleit solution again for 30 min. Different concentrations of H2O2 (0.1, 0.3, 1, 3, 10 and 30 μmol/L), N-(2-mercaptopropionyl) glycine (2-MPG, 300 μmol/L, Merck), a ROS scavenger, AG490 (300 nmol/L), and spermine (2 μmol/L, Merck), a MCU agonist [36, 57, 58], were administered at the beginning of reperfusion for 5 min. LV myocytes were harvested from the same heart for protein extraction at preischemia (Pre), reperfusion 5 min (R5) and reperfusion 30 min (R30).
Measurement of [Ca2+]c, [Ca2+]m, Ca2+ transients and cell shortening
An IonOptix system (Milton, Massachusetts, USA) was used to measure Ca2+ transients and cell shortening simultaneously as previously described [11, 15, 32]. The calcium indicator Indo-1 AM (5 μmol/L, Thermo Fisher, Massachusetts, USA) was used to measure [Ca2+]c and Rhod 2-AM (5 μmol/L, Thermo Fisher, Massachusetts, USA) was used to measure [Ca2+]m as previously described [12]. The detailed method is available in Supplementary materials online.
ROS detection
ROS production in isolated cardiomyocytes during simulated I/R was detected using 5 (and 6)-carboxy-2,7-dichlorodihydrofluerescein diacetate (DCF; Thermo Fisher, Massachusetts, USA) as previously described [52]. Cardiomyocytes from control or moderate H2O2PoC groups were loaded with DCF (20 μmol/L) for 10 min before plating on the dish. The acetate groups of the probe can be removed by intracellular esterases, which allow the retention of the probe by the cells. Because DCF is nonfluorescent until it is oxidized by ROS within the cell, the intracellular generation of ROS was reflected by monitoring the increase in DCF fluorescence. Fluorescence was detected using an inverted microscope (Nikon, Tokyo, Japan) and recorded (excitation/emission: 495/525 nm) every 5 min during I/R with a fixed field of view including 30–50 rod-shaped cardiomyocytes. The excitation light source was set at low power to avoid inducing oxidation and opened only when it was needed for imaging. Fluorescence intensity was analyzed with Image-Pro Plus software (Media Cybernetics).
ATP quantification by luminescence
The ATP level within the mitochondria was quantified using the ATPlite luminescence ATP detection assay system (Perkin Elmer, Massachusetts, USA) as per the kit instructions.
Mitochondrial function
The electron transport chain supercomplex activities of mitochondrial function were estimated spectrophotometrically using specific donor–acceptors chemistry following the kit (GENMED, Shanghai, China) instructions. For complex I, rotenone-sensitive NADH-oxidoreductase was used; succinate decylubiquinone dichlorophenolindophenol (DCPIP) reductase was used to assess complex II. Ubiquinol reductase was used to assess the activities of complex III and cytochrome c was used to assess complex IV. All the mitochondrial activities were normalized with protein.
Mitochondrial membrane potential (ΔΨm) assay
ΔΨm was determined by a 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylimidacarbocyanine iodide (JC-1) assay kit (Beyotime, Nantong, China) using a Gemini™ EM fluorescence microplate reader (Molecular Devices, California, USA) as previously described [55]. The detailed method is available in Supplementary materials online.
Western blot analysis
The standard western blot analysis for mitochondrial protein or immunoprecipitates from LV myocytes was performed as previously described [11, 12, 32] with antibodies against STAT3 (1:2000, Cell Signaling Technology, Massachusetts, USA), MCU (1:2000, Cell Signaling Technology, Massachusetts, USA), Flag (1: 5000, Proteintech, Illinois, USA), phospho-STAT3ser727 (pS-STAT3) (1:2000, Cell Signaling Technology, Massachusetts, USA), cytochrome c oxidase IV (COXIV) (1:2000, Santa Cruz, California, USA) and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (1:8000, Cell Signaling Technology, Massachusetts, USA). The detailed method is available in Supplementary materials online.
Co-immunoprecipitation assay
The co-immunoprecipitation experiments were performed as described previously [32]. The LV myocytes lysates were immunoprecipitated with anti-STAT3 (Cell Signaling Technology), anti-pS-STAT3 (Cell Signaling Technology) anti-MCU (Cell Signaling Technology) and anti-Flag (Proteintech) as well as with negative control antibodies, normal rabbit (Proteintech) or mouse IgG antibodies (Santa Cruz). The detailed method is available in Supplementary materials online.
Immunofluorescence analysis
The immunofluorescence experiments were performed as described previously [32]. First, the myocytes were fixed with paraformaldehyde and then co-immunostained with antibodies against STAT3 (Cell Signaling Technology), MCU (Abcam, Cambridge, UK). Finally, laser-scanning confocal microscopy (Leica, Heidelberg, Germany) was used to observe them. The detailed method is available in Supplementary materials online.
Statistical analysis
All values were expressed as mean ± standard error of the mean (SEM) and analyze the differences among groups by one-way repeated or muti-way analysis of variance (ANOVA) followed by the Tukey–Kramer multiple-comparison post hoc tests using SPSS v 22.0 (SPSS). P < 0.05 was considered statistically significant.
Results
Moderate H2O2PoC promoted the post-ischemic myocardial contractile function recovery and decreased infarct size via activated STAT3
To determine the role of STAT3 in the cardioprotection afforded by moderate H2O2PoC, LV contractile function and infarct size were detected in the I/R injury model of Langendorff-perfused rat hearts. LVDP, LVEDP, + dP/dtmax and − dP/dtmax were remarkably suppressed after global non-flow I/R (30-min/45-min, Fig. 1a), while the suppression was markedly attenuated by moderate H2O2PoC (20 μmol/L, Fig. 1a) [53]. These protections were abrogated by AG490 (20 µmol/L) administered during reperfusion for the first 5 min (Fig. 1a, Online Fig. 1a), although the HR of the different groups remained similar after global non-flow I/R (30-min/45-min, Online Fig. 1b). Consistently, moderate H2O2PoC significantly attenuated myocardial infarct size after global non-flow I/R (30-min/2-h) and such a protection was attenuated in the AG490 group (28.8 ± 1.2% in H2O2PoC vs. 58.5 ± 2.9% in H2O2PoC with AG490, P < 0.001), but no effect was observed in the control I/R heart (Fig. 1b). These results suggested a key role of the activated STAT3 during early reperfusion in cardioprotection afforded by moderate H2O2PoC.
Effects of H2O2PoC (20 µmol/L) during global no-flow I/R (30-min/45-min) on post-ischemic myocardial contractile function recovery and infarct size with or without the suppression of STAT3 activation by AG490 (20 µmol/L). a Summarized effects of H2O2PoC on post-ischemic left ventricular (LV) developed pressure (LVDP) (left upper), LV end-diastolic pressure (LVEDP) (right upper), maximum left ventricular dP/dt (+ dp/dt) (left bottom) and minimum left ventricular dP/dt (− dp/dt) (right bottom) recovery with or without AG490. b Effects of H2O2PoC on myocardial infarct size with or without AG490 expressed as a percentage of the LV area at risk. n = 3–6 each. Pre, preischemia; Ctrl, I/R control; H2O2PoC, hydrogen peroxide postconditioning; AG490, inhibitor of JAK2/STAT3. Statistical significance was achieved by muti-way ANOVA followed by Tukey–Kramer multiple comparison: ##P< 0.01, ###P < 0.001 vs. corresponding I/R control; ††P < 0.01, †††P < 0.001 vs. corresponding H2O2PoC values
Moderate H2O2PoC achieved cardioprotection in cardiomyocytes and simulated enhanced ROS production during early reperfusion
To determine the different roles of H2O2 during reperfusion in I/R injury and cardioprotection in cardiomyocytes, the concentration-dependent effects of H2O2PoC on post-ischemic [Ca2+]c, Ca2+ transients and cell shortening were examined in isolated cardiomyocytes from rat hearts. Moderate H2O2PoC (1 μmol/L and 3 μmol/L) significantly reduced [Ca2+]c overload induced by I/R in cardiomyocytes, whereas low-dose H2O2PoC (0.1 μmol/L and 0.3 μmol/L) and high-dose H2O2PoC (10 μmol/L and 30 μmol/L) were the same with control I/R, without statistical significance (Fig. 2a). Moreover, moderate H2O2PoC (3 μmol/L) obviously reversed the I/R-altered parameters, including amplitude, maximum upstroke velocity (upstroke Vmax), and half-decay time (decay rate τ) or maximum return velocity (return Vmax) of Ca2+ transients (Online Fig. 2a) and cell shortening (Online Fig. 2b). However, H2O2PoC (1 μmol/L) improved the decay rate of Ca2+ transients (Online Fig. 2a) and return Vmax of cell shortening (Online Fig. 2b). Thus, H2O2PoC (3 μmol/L) was chosen as the moderate H2O2PoC.
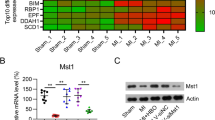
Moderate H2O2PoC (3 µmol/L) alleviated Ca2+ overload and improved the expression of mitochondrial phospho-STAT3 and STAT3 during I/R. a Cytosolic free calcium concentration [Ca2+]c in different concentrations (0.1, 0.3, 1, 3, 10, 30 μmol/L) of H2O2PoC. The number of myocytes is indicated in parentheses. b Expression of mitochondrial pS-STAT3 (left) and STAT3 (right) in isolated cardiomyocytes from control or H2O2PoC group with or without AG490, as detected by western blot analysis. COXIV, cytochrome c oxidase IV, was used as a housekeeping protein of mitochondria. n = 3–8 each. AG490, 300 nmol/L; Pre, preischemia; R5, 5 min of reperfusion; and R30, 30 min of reperfusion. Statistical significance was achieved by one-way repeated ANOVA followed by Tukey–Kramer multiple comparison: *P < 0.05, **P< 0.01, ***P < 0.01 vs. corresponding preischemic values; Statistical significance was achieved by muti-way ANOVA followed by Tukey–Kramer multiple comparison: #P < 0.05, ##P < 0.01, ###P < 0.001 vs. corresponding control values. †P < 0.05, †††P < 0.001 vs. corresponding H2O2PoC values
To determine whether H2O2PoC (3 μmol/L) could mimic the endogenously enhanced ROS production during early reperfusion seen in IHH [52], the ROS production was monitored in isolated cardiomyocytes subjected to simulated I/R using DCF fluorescence. The DCF fluorescence intensity was significantly enhanced during early reperfusion in the simulated I/R cardiomyocytes isolated from control rat hearts and was further enhanced by H2O2PoC. Such enhancement was totally suppressed by 2-MPG (Online Fig. 3a), a similar pattern seen in the IHH-enhanced ROS production during the early reperfusion [52]. Further, the mitochondrial function was detected. Moderate H2O2PoC significantly improved post-ischemic mitochondrial function, including the content of ATP (Online Fig. 3b) and the activities of complex I (Online Fig. 3c), complex II (Online Fig. 3d) and complex IV (Online Fig. 3f) at R30. H2O2PoC also improve the activities of complex III (Online Fig. 3e) at R30,but with no statistical significance.
Moderate H2O2PoC activated mitochondrial STAT3 during early reperfusion
To further confirm moderate H2O2PoC on activation of STAT3 in cardiomyocytes, the endogenous expression pattern of mitochondrial pS-STAT3 and STAT3 was examined in cardiomyocytes with or without I/R and moderate H2O2PoC. I/R suppressed the pS-STAT3 and STAT3 levels, although the COXIV level was still unchanged during reperfusion. Therefore, I/R decreased the ratios of pS-STAT3 to COXIV (Fig. 2b left) and STAT3 to COXIV (Fig. 2b right) at R5 and R30. The pS-STAT3, STAT3, and COXIV were comparable during preischemia among each group. Moderate H2O2PoC (3 μmol/L) further recovered the I/R-suppressed pS-STAT3 and STAT3 at R5 and R30, although moderate H2O2PoC did not affect COXIV. Interestingly, the mitochondrial pS-STAT3 and STAT3 expression in I/R cardiomyocytes was not changed by AG490 (300 nmol/L) treatment during reperfusion for the first 5 min, but the effects of H2O2PoC on the levels of mitochondrial pS-STAT3 and STAT3 were weakened by AG490 at both R5 and R30 (Fig. 2b). The aforementioned results demonstrated that mitochondrial STAT3 was required in moderate H2O2PoC-conferred cardioprotection.
Moderate H2O2PoC protected the post-ischemic [Ca2+]c, [Ca2+]m, ΔΨm, Ca2+ transients and cell shortening through activated STAT3
To examine whether activated STAT3 contributed to moderate H2O2PoC-induced calcium homeostasis, normal cell contraction and normal ΔΨm during reperfusion, [Ca2+]c in myocyes, [Ca2+]m in myocytes, ΔΨm, Ca2+ transients and cell shortening of LV myocytes were detected during simulated I/R (20-min/30-min). The preischemic and ischemic levels of [Ca2+]c and [Ca2+]m were similar in all groups. However, moderate H2O2PoC remarkably alleviated resting [Ca2+]c and [Ca2+]m overload due to I/R at R30. Such a protection was abolished by knocking down STAT3 with adenovirus delivery of shRNA (AdSTAT3shRNA, Online Fig. 4a), although the resting [Ca2+]c (Online Fig. 5a) and [Ca2+]m (Fig. 3a) of the control AdScramble group were not affected by the interventions (Online Fig. 4b). Moreover, I/R-induced decreases in ΔΨm (Fig. 3b) at R5 and R30 were completely reversed by moderate H2O2PoC, while these protective effects were abrogated by AdSTAT3shRNA (Fig. 3b).
Effects of H2O2PoC (3 µmol/L) during simulated I/R (20 min/30 min) on post-ischemic [Ca2+]m, ΔΨm, Ca2+ transients and cell shortening in cardiomyocytes with or without down-regulation of STAT3. a Mitochondrial free calcium concentration [Ca2+]m. b Mitochondrial membrane potential (ΔΨm). Amplitude, maximum upstroke velocity, and half-decay time or maximum return velocity of Ca2+ transients (c) and cell shortening (d). Adscramble, adenoviruses carrying the shRNA scramble; AdSTAT3shRNA, adenoviruses carrying the short hairpin RNA specific for STAT3. The number of myocytes is indicated in parentheses. Statistical significance was achieved by one-way repeated ANOVA followed by Tukey–Kramer multiple comparison: *P < 0.05, **P < 0.01, ***P < 0.001 vs corresponding preischemic values; Statistical significance was achieved by muti-way ANOVA followed by Tukey–Kramer multiple comparison: #P < 0.05, ##P < 0.01, ###P < 0.001 vs. corresponding control values; †P < 0.05, ††P < 0.01, †††P< 0.001 vs. corresponding H2O2PoC values
Consistently, moderate H2O2PoC obviously reversed the I/R-altered parameters, including amplitude, upstroke Vmax, and decay rate τ or return Vmax of Ca2+ transients (Fig. 3c) and cell shortening (Fig. 3d) at R30. No difference in these parameters was detected among all groups before ischemia. This protection was abolished by AdSTAT3shRNA (Fig. 3c, d), while the aforementioned parameters of the control AdScramble group were not affected by the interventions (Fig. 3). These results implied that STAT3 plays a vital role in H2O2PoC-induced maintenance of Ca 2+ homeostasis and enhancement of Ca2+ transients and cell shortening during I/R.
Moderate H2O2PoC protected the post-ischemic [Ca2+]c, [Ca2+]m, ΔΨm, Ca2+ transients and cell shortening via the inhibition of MCU
To explore whether inhibiting MCU contributed to the cardioprotective effects of H2O2PoC during reperfusion, [Ca2+]c, [Ca2+]m, ΔΨm, Ca2+ transients, and cell shortening with or without the MCU agonist spermine (2 μmol/L) were examined during I/R (Fig. 4, Online Fig. 4b). The preischemic and ischemic levels of [Ca2+]c and [Ca2+]m were similar in all groups, whereas moderate H2O2PoC (3 μmol/L) reduced [Ca2+]c (Online Fig. 5b) and [Ca2+]m (Fig. 4a) overload and preserved the reduced ΔΨm (Fig. 4b) due to I/R during reperfusion. These attenuations and preservations were abrogated by spermine added during reperfusion for the first 5 min. Similarly, the dynamics of Ca2+ transients and cell shortening were altered by I/R and improved by moderate H2O2PoC at R30, but such improvement was also totally inhibited by spermine (Fig. 4c, d). These parameters of the control group were not affected by the interventions (Fig. 4). These results indicated that inhibiting MCU played an important role in moderate H2O2PoC-induced maintenance of Ca 2+ homeostasis and enhancement of Ca2+ transients and cell shortening during I/R.
Effects of H2O2PoC (3 µmol/L) during simulated I/R (20 min/30 min) on [Ca2+]m, ΔΨm, Ca2+ transients and cell shortening in cardiomyocytes with or without opening of MCU. a Mitochondrial free calcium concentration [Ca2+]m. b Mitochondrial membrane potential (ΔΨm). Amplitude, maximum upstroke velocity, and half-decay time or maximum return velocity of Ca2+ transients (c) and cell shortening (d). Sper: spermine, the opener of MCU. The number of myocytes is indicated in parentheses. Statistical significance was achieved by one-way repeated ANOVA followed by Tukey–Kramer multiple comparison: ***P < 0.001 vs. corresponding preischemic values; Statistical significance was achieved by muti-way ANOVA followed by Tukey–Kramer multiple comparison: #P < 0.05, ##P < 0.01, ###P < 0.001 vs. corresponding control values; †P < 0.05, ††P < 0.01, †††P< 0.001 vs. corresponding H2O2PoC values
STAT3 inhibited the opening of MCU in moderate H2O2PoC-afforded cardioprotection
[Ca2+]m overload is caused by the opening of MCU during I/R and the activation of STAT3 in moderate H2O2PoC-alleviated [Ca2+]m overload. Hence, the role of MCU in STAT3-mediated moderate H2O2PoC-induced cardioprotection was clarified through simultaneously examining the time course of [Ca2+]c, [Ca2+]m, ΔΨm, Ca2+ transients, and cell shortening with spermine (2 μmol/L) in cardiomyocytes transfected with recombinant adenoviruses expressing rat STAT3 (AdSTAT3, Online, Fig. 6a) in H2O2PoC (Fig. 5, Online Fig. 4b). No significant differences were observed in preischemic resting [Ca2+]c (Online Fig. 5c), [Ca2+]m (Fig. 5a), ΔΨm (Fig. 5b) and the dynamics of Ca2+ transients (Fig. 5c) and cell shortening (Fig. 5d) among all groups. However, moderate H2O2PoC and STAT3 overexpression by adenoviruses significantly rescued I/R-changed resting [Ca2+]c (Online Fig. 5c), [Ca2+]m (Fig. 5a), ΔΨm (Fig. 5b) and the parameters of Ca2+ transients (Fig. 5c) and cell shortening (Fig. 5d). Moderate H2O2PoC-conferred cardioprotection was mimicked by AdSTAT3 but AdSTAT3-induced cardioprotection was blocked by spermine (Fig. 5a–d, Online Fig. 5c). Besides, the cardioprotective effects of H2O2PoC remained unchanged with spermine in cardiomyocytes transfected with AdSTAT3 (Fig. 5a–d, Online Fig. 5c). Therefore, it was concluded that STAT3 mediates the cardioprotection of H2O2PoC through inhibiting the opening of MCU.
Effects of H2O2PoC (3 µmol/L) and spermine during simulated I/R (20-min/30-min) on [Ca2+]m, ΔΨm, Ca2+ transients and cell shortening in cardiomyocytes with or without the overexpression of STAT3. a Mitochondrial free calcium concentration [Ca2+]m. b Mitochondrial membrane potential (ΔΨm). Amplitude, maximum upstroke velocity, and half-decay time or maximum return velocity of Ca2+ transients (c) and cell shortening (d). AdVector, adenoviruses carrying the vector; AdSTAT3, adenoviruses carrying the rat STAT3. The number of myocytes is indicated in parentheses. Statistical significance was achieved by one-way repeated ANOVA followed by Tukey–Kramer multiple comparison: ***P < 0.001 vs. corresponding preischemic values; Statistical significance was achieved by muti-way ANOVA followed by Tukey–Kramer multiple comparison: #P < 0.05, ###P < 0.001 vs. corresponding control values; †P < 0.05, †††P < 0.001 vs. corresponding H2O2PoC + Sper values
Moderate H2O2PoC facilitated the interaction between STAT3 or pS-STAT3 and MCU during reperfusion
Subsequently, whether MCU was the direct target of STAT3 was examined. The specific immunofluorescent images were used. STAT3 and MCU seem to be co-localized in the moderate- H2O2PoC cardiomyocytes at R5 and R30, whereas no co-localization of the two proteins was found in control simulated I/R cells and before ischemia (Fig. 6a). Next, co-immunoprecipitation was performed to check the protein interaction between STAT3 or pS-STAT3 and MCU. MCU was detected in the immunoprecipitates from cardiomyocytes of moderate-H2O2PoC groups with anti-STAT3 (Fig. 6b) or anti-pS-STAT3 (Fig. 6c). STAT3 (Fig. 6b) or pS-STAT3 (Fig. 6c) was detected in the immunoprecipitates from cardiomyoctes of moderate-H2O2PoC groups with anti-MCU at R5 and R30 but not before ischemia. The interaction of STAT3 or pS-STAT3 and MCU was not seen in the control I/R cadiomyocytes (Fig. 6b, c). These data were consistent with the effect on the expression of mitochondrial STAT3 and regulation of [Ca2+]c and [Ca2+]m by activated STAT3 through the inhibition of MCU by H2O2PoC.
Co-localization and interaction of STAT3 with MCU in rat cardiomyocytes. a Representative images of cardiomyocytes with dual immunostaining in the control and H2O2PoC groups at Pre, R5 and R30. Red represents STAT3, green represents MCU, and blue represents nuclei. Scale bars, 25 μm. b Co-immunoprecipitation analysis for the interaction between STAT3 and MCU in the control and H2O2PoC groups at Pre, R5 and R30. c Co-immunoprecipitation analysis for the interaction between pS-STAT3 and MCU in the control and H2O2PoC groups at Pre, R5 and R30. The interaction of STAT3 or pS-STAT3 with endogenous MCU in the immunoprecipitates was detected by Western blot analysis with anti-STAT3, anti-pS-STAT3 or anti-MCU antibodies. n = 3
To further explore the interacting domains of MCU and STAT3, mutant MCU with NTD deletion MCUΔ75–165 (Flag-MCUΔ75–165) was expressed as a Flag fusion protein. Wild-type MCU (Flag-MCU WT) also expressed as a Flag fusion protein (Fig. 7a).Co-immunoprecipitation was performed using lysates harvested from myocytes transfected with recombinant adenoviruses expressing rat Flag-MCU WT (AdFlag-MCU WT) or Flag-MCUΔ75–165 (AdFlag-MCUΔ75–165) subjected to simulated I/R with moderate H2O2PoC. Immobilized Flag-MCUΔ75–165 failed to interact with STAT3, whereas Flag-MCU WT still interacted with STAT3 at R5 (Fig. 7b). Immunoblotting with Flag antibody revealed the same amount of Flag-MCU WT or Flag-MCUΔ75–165 in the immunoprecipitates (Online, Fig. 6b). Thus, STAT3 probably prevented MCU activity via the interaction of STAT3 with MCU NTD.
Interacting regions of MCU with STAT3 in rat cardiomyocytes. a Schematic representation of 3×Flag-tagged wild-type MCU (Flag-MCU WT) and 3×Flag-tagged mutant MCU with the N-terminal domain (NTD) deletion (Flag-MCUΔ75-165) fusion proteins. b Co-immunoprecipitation analysis for the interacting regions between STAT3 and MCU at R5 in H2O2PoC. The interaction of STAT3 with exogenous Flag-MCU WT or Flag-MCUΔ75-165 in the immunoprecipitates was detected by Western blot analysis with anti-STAT3 or anti-Flag antibodies. n = 3
Discussion
This study demonstrated that (1) moderate H2O2PoC protected the heart from I/R injury via activating STAT3; (2) moderate H2O2PoC significantly activated mitochondrial STAT3; (3) moderate H2O2PoC alleviated I/R-induced calcium overload and contraction suppression in ventricular myocytes via activating STAT3 and inhibiting MCU; (4) STAT3 inhibited the opening of MCU in moderate H2O2PoC-alleviated I/R-induced [Ca2+]m overload through its interaction with MCU; (5) STAT3 could interact with MCU at NTD, which might be involved in the uptake of cytosolic calcium into mitochondria. These findings extended previous findings, demonstrated a vital role of STAT3 in the post-ischemic moderate ROS-induced cardioprotection, and provided new insights into the mechanisms underlying the cardioprotection of STAT3.
The role of ROS in cardioprotection or I/R injury depends on different kinds of ROS, ROS concentrations and availability of ROS reaction partners. Superoxide and H2O2 are produced normally and may have protective actions via signaling for preconditioning activating multiple groups of protective proteins. However, with I/R the normal balance is lost and hydroxyl radicals can be produced direct cellular injury [4]. Low levels of H2O2 aggravate contractile dysfunction through endoplasmic reticulum stress, moderate levels of H2O2 are associated with increased postischemic LV performance through protein kinase B (PKB/Akt) and protein kinase C epsilon (PKCε) activation. However, high amounts of H2O2 aggravate contractile dysfunction through oxidant stress [53]. In the models of cardioprotection by RIPC, IPC and TNF-α preconditioning, mitochondrial ROS was reduced [17, 24, 26, 49]. Myocardial I/R injury was effectively reduced after administering melatonin, vitamin C, resveratrol, N-acetylcysteine or N-mercaptopropionylglycine [7]. However, RIPC protected the heart from I/R injury through the ROS-dependent mechanism because ROS scavengers attenuated infarct size reduction by RIPC [19]. Besides, ROS signaling at the onset of reperfusion play an important role in a model of cardioprotection by IPoC because ROS scavenger administered during the whole reperfusion phase abolished its effects [7]. Excessive ROS production during early reperfusion is a critical cause of calcium overload in cardiomyocytes [1, 49]. However, enhanced ROS during early reperfusion in IHH significantly reduced calcium overload [55]. These findings suggested that ROS generation should be quantified at a moderate level to achieve calcium homeostasis. As the ROS production in the IHH model is endogenous and it is hard to quantified, the H2O2PoC model was designed to represent the exact concentration of ROS during early reperfusion in an exogenous manner. The data confirmed the previous findings that moderate H2O2PoC (20 μmol/L) promoted the recovery of post-ischemic myocardial contractile function and limited the infract size reported recently [53]. Moreover, this study demonstrated that moderate H2O2PoC (3 μmol/L) reduced calcium overload due to I/R in cardiomyocytes. This was consistent with the observation that moderate H2O2 (25 μmol/L) given at the beginning of reoxygenation alleviated calcium accumulation in isolated adult rat hypoxia/reoxygenation cardiomyocytes [46].
Although several signal pathways interacting with mitochondria such as the reperfusion injury salvage kinases (RISKs), including PKB/Akt and PKCε, are implicated in IPC, IPoC, RIPC, IHH and H2O2PoC [20, 21, 26, 33, 47, 52, 53], the role of the survivor activating factor enhancement (SAFE) pathway, including JAK2/STAT3, remains unclear in H2O2PoC. Similar to an increase of STAT3 phosphorylation in a ROS-dependent manner in the IHH rat heart [55], an increase in I/R-decreased mitochondrial STAT3 expression in moderate-H2O2PoC cardiomyocytes implied a crucial role of STAT3 in the moderate H2O2PoC-conferred cardioprotection against I/R insult. This was further supported by the disappeared better post-ischemic cardiac contraction and more infarct size of H2O2PoC rat hearts treated with AG490. Accordingly, IPC-, IPoC-, IHH-induced cardioprotection was attenuated by AG490 in rat/mouse hearts [5, 18, 55]. It has been also reported that along with reduced infarct size, the ratio of pY-STAT3/total STAT3 protein at early reperfusion was significantly increased by IPC, but only trendwise by IPoC and RIPC and the expression of pY-STAT3 was increased at late reperfusion by RIPC in pig heart [23, 25]. The possible reason for the difference is different animal model with different treatment. Moreover, moderate H2O2PoC attenuated I/R-induced [Ca2+]c and [Ca2+]m overload and improved I/R-altered Ca2+ transients and cell shortening depending on STAT3. This was also consistent with the observation that IHH-induced attenuation of [Ca2+]c and [Ca2+]m overload and enhancement of Ca2+ transients and cell shortening was cancelled by AG490 in cardiomyocytes [55]. These data revealed that STAT3 participated in ROS signal transduction during cardioprotection as an important down-stream mediator.
Mitochondria are one of the major effectors that regulate Ca2+ homeostasis in cardiomyocytes. Calcium enters the mitochondria primarily through the MCU [14]. Previous studies found that the cardioprotective effects of B-type natriuretic peptide (BNP) postconditioning were through preventing the opening of MCU partly related to recovering mitochondrial membrane potential and attenuating ROS generation in I/R cardiomyocytes [50]. However, inhibiting MCU was found to play a crucial role in post-ischemic moderate ROS-induced cardioprotection with the model of moderate H2O2PoC. This was similar to the finding on perfusing the heart with spermine, and the cardioprotective effects of IPC and IPoC were abolished [57, 60]. Although previous studies also found that ROS production was reduced in the mice with a dominant-negative form of MCU [45], the present study showed that inhibiting MCU contributed to moderate ROS-induced attenuation of [Ca2+]c and [Ca2+]m overload. This result was consistent with the previous results that Ru360 or ruthenium red, at certain concentrations, abolished [Ca2+]c and [Ca2+]m overload in cardiac I/R injury [1, 10]. These data demonstrated that inhibiting MCU was one of the targets of post-ischemic moderate ROS during cardioprotection.
Activated STAT3 is involved in TNF-α preconditioning and postconditioning [28, 29], and TNF-α preconditioning attenuates Ca2+ overload in rat organotypic hippocampal cultures [2]. Thus, activated STAT3 during reperfusion would act as an important mediator for the attenuation of calcium overload in cardiomyocytes as observed in IHH [55]. Moreover, diazoxide preconditioning against transient focal cerebral ischemia was attenuated by spermine in rats [58] and protected spinal cord from I/R insult by significantly increasing the phosphorylation of STAT3 [56]. The present study found that mitochondrial STAT3 during early reperfusion reduced Ca2+ overload via inhibiting the opening of MCU in H2O2PoC-induced cardioprotection. This was consistent with the finding that inhibiting MCU contributed to TNF-α preconditioning in isolated rat I/R hearts [16]. Drugs or RNAi-induced inhibition of MCU abrogated cell death in mouse heart during I/R, presumably by reducing Ca2+ influx into mitochondria and inhibiting the opening of mitochondrial permeability transition pore (mPTP) [27]. Inhibiting the opening of mPTP in cardiomyocytes isolated from preconditioning rats and skeletal muscle isolated from postconditioning rats significantly attenuated [Ca2+]m overload [35, 61]. pS-STAT3 inhibited the opening of mPTP via interacting with cyclophilin D in rat cardiomyocytes [6, 48]. This raised the question whether STAT3 inhibited the opening of MCU through the regulation of mPTP. However, no cardioprotective effect was found in MCU knockout mice I/R heart treated with the mPTP inhibitor [14]. Therefore, other mechanisms involved in the direct regulatory effect of STAT3 on MCU were explored.
pS-STAT3 is crucial for interacting with 14-3-3ζ, a regulatory signaling molecule in mitochondria that phosphorylates other proteins in an interaction-dependent manner and acts as a chaperone [59]. The 14-3-3 protein isoforms υ, β, ζ have been demonstrated to interact with uncoupling protein 2 (UCP2), a member of mitochondrial ion transporters and a mitochondrial membrane protein [43]. Further, UCP2 has been shown to probably interact with MCU to regulate the process of transferring calcium from the cytoplasm to mitochondria in cardiomyocytes [38]. The data revealed an interaction between the STAT3 protein and the MCU protein using co-immunoprecipitation and immunofluorescence. STAT3 has been proved to regulate ROS generation and mitochondrial respiration for its interacting with mitochondrial complex I and complex II [51, 54]. This study was novel in proving that STAT3 inhibited the opening of MCU via interacting with MCU in cardioprotection. STAT3 is imported into mitochondria and recruited into complex I located in the inner mitochondrial membrane [54] and MCU is an ion channel in mitochondria composed of transmembrane proteins with N- and C-termini facing the matrix [34]. Hence, the possible interaction domains of STAT3 and MCU need investigation. A previous study showed that the NTD of MCU was an essential domain of MCU interacting with the regulators to modulate the mitochondrial calcium uptake [30]. Thus, it was confirmed that STAT3 could not interact with mutant MCU with NTD deletion (MCUΔ75-165) but interact with MCU WT in an exogenous-overexpression manner in cardiomyocytes, indicating that STAT3 might serve as a new regulator for MCU.
In conclusion, this study demonstrated that moderate H2O2PoC-mimicked IHH protected the heart/cardiomyocytes from I/R-induced calcium overload and contractile dysfunction via mitochondrial STAT3 interaction with the NTD of MCU to achieve the inhibition of MCU opening (Online Fig. 7). These findings suggested that moderate H2O2PoC might be a proper approach to study the quantity of post-ischemic ROS during early reperfusion and its cardioprotective mechanism.
References
Abdallah Y, Kasseckert SA, Iraqi W, Said M, Shahzad T, Erdogan A, Neuhof C, Gunduz D, Schluter KD, Tillmanns H, Piper HM, Reusch HP, Ladilov Y (2011) Interplay between Ca2+ cycling and mitochondrial permeability transition pores promotes reperfusion-induced injury of cardiac myocytes. J Cell Mol Med 15:2478–2485. https://doi.org/10.1111/j.1582-4934.2010.01249.x
Barger SW, Hörster D, Furukawa K, Goodman Y, Krieglstein J, Mattson MP (1995) Tumor necrosis factors alpha and beta protect neurons against amyloid beta-peptide toxicity: evidence for involvement of a kappa B-binding factor and attenuation of peroxide and Ca2+ accumulation. Proc Natl Acad Sci USA 92:9328–9332
Barry SP, Townsend PA, Latchman DS, Stephanou A (2007) Role of the JAK-STAT pathway in myocardial injury. Trends Mol Med 13:82–89. https://doi.org/10.1016/j.molmed.2006.12.002
Becker LB (2004) New concepts in reactive oxygen species and cardiovascular reperfusion physiology. Cardiovasc Res 61:461–470. https://doi.org/10.1016/j.cardiores.2003.10.025
Boengler K, Buechert A, HeinenY Roeskes C, Hilfiker-Kleiner D, Heusch G, Schulz R (2008) Cardioprotection by ischemic postconditioning is lost in aged and STAT3-deficient mice. Circ Res 102:131–135. https://doi.org/10.1161/CIRCRESAHA.107.164699
Boengler K, Hilfiker-Kleiner D, Heusch G, Schulz R (2010) Inhibition of permeability transition pore opening by mitochondrial STAT3 and its role in myocardial ischemia/reperfusion. Basic Res Cardiol 105:771–785. https://doi.org/10.1007/s00395-010-0124-1
Boengler K, Lochnit G, Schulz R (2018) Mitochondria “THE” target of myocardial conditioning. Am J Physiol Heart Circ Physiol 315:H1215–H1231. https://doi.org/10.1152/ajpheart.00124.2018
Bøtker HE, Hausenloy D, Andreadou I, Antonucci S, Boengler K, Davidson SM, Deshwal S, Devaux Y, Di Lisa F, Di Sante M, Efentakis P, Femminò S, García-Dorado D, Giricz Z, Ibanez B, Iliodromitis E, Kaludercic N, Kleinbongard P, Neuhäuser M, Ovize M, Pagliaro P, Rahbek-Schmidt M, Ruiz-Meana M, Schlüter KD, Schulz R, Skyschally A, Wilder C, Yellon DM, Ferdinandy P, Heusch G (2018) Practical guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection. Basic Res Cardiol 113:39. https://doi.org/10.1007/s00395-018-0696-8
Brookes PS, Yoon Y, Robotham JL, Anders MW, Sheu SS (2004) Calcium, ATP, and ROS: a mitochondrial love-hate triangle. Am J Physiol Cell Physiol 287:C817–833. https://doi.org/10.1152/ajpcell.00139.2004
Cao CM, Yan WY, Liu J, Kam KW, Zhan SZ, Sham JS, Wong TM (2006) Attenuation of mitochondrial, but not cytosolic, Ca2+ overload reduces myocardial injury induced by ischemia and reperfusion. Acta Pharmacol Sin 27:911–918. https://doi.org/10.1111/j.1745-7254.2006.00391.x
Chen L, Lu XY, Li J, Fu JD, Zhou ZN, Yang HT (2006) Intermittent hypoxia protects cardiomyocytes against ischemia-reperfusion injury-induced alterations in Ca2+ homeostasis and contraction via the sarcoplasmic reticulum and Na+/Ca2+ exchange mechanisms. Am J Physiol Cell Physiol 290:C1221–1229. https://doi.org/10.1152/ajpcell.00526.2005
Chen YX, Liu JL, Zheng YJ, Wang JX, Wang ZH, Gu SS, Tan JL, Jing Q, Yang HT (2015) Uncoupling protein 3 mediates H2O2 preconditioning-afforded cardioprotection through the inhibition of MPTP opening. Cardiovasc Res 105:192–202. https://doi.org/10.1093/cvr/cvu256
de Jesus Garcia-Rivas G, Guerrero-Hernandez A, Guerrero-Serna G, Rodriguez-Zavala JS, Zazueta C (2005) Inhibition of the mitochondrial calcium uniporter by the oxo-bridged dinuclear ruthenium amine complex (Ru360) prevents from irreversible injury in postischemic rat heart. FEBS J 272:3477–3488. https://doi.org/10.1111/j.1742-4658.2005.04771.x
Finkel T, Menazza S, Holmstrom KM, Parks RJ, Liu J, Sun J, Liu J, Pan X, Murphy E (2015) The ins and outs of mitochondrial calcium. Circ Res 116:1810–1819. https://doi.org/10.1161/CIRCRESAHA.116.305484
Gao H, Chen L, Yang HT (2007) Activation of alpha1B-adrenoceptors alleviates ischemia/reperfusion injury by limitation of mitochondrial Ca2+ overload in cardiomyocytes. Cardiovasc Res 75:584–595. https://doi.org/10.1016/j.cardiores.2007.04.008
Gao Q, Zhang SZ, Mao HH, Li QS, Cao CM, Xia Q (2006) Mitochondrial calcium uniporter participates in TNF-alpha induced cardioprotection in isolated rat hearts subjected to ischemia/reperfusion. Zhongguo Ying Yong Sheng Li Xue Za Zhi 22:278–282
Gedik N, Maciel L, Schulte C, Skyschally A, Heusch G, Kleinbongard P (2017) Cardiomyocyte mitochondria as targets of humoral factors released by remote ischemic preconditioning. Arch Med Sci. 13:448–458. https://doi.org/10.5114/aoms.2016.61789
Hattori R, Maulik N, Otani H, Zhu L, Cordis G, Engelman RM, Siddiqui MA, Das DK (2001) Role of STAT3 in ischemic preconditioning. J Mol Cell Cardiol 33:1929–1936. https://doi.org/10.1006/jmcc.2001.1456
Hauerslev M, Mørk SR, Pryds K, Contractor H, Hansen J, Jespersen NR, Johnsen J, Heusch G, Kleinbongard P, Kharbanda R, Bøtker HE, Schmidt MR (2018) Influence of long-term treatment with glyceryl trinitrate on remote ischemic conditioning. Am J Physiol Heart Circ Physiol 315:H150–H158. https://doi.org/10.1152/ajpheart.00114.2018
Heusch G (2015) Molecular basis of cardioprotection: signal transduction in ischemic pre-, post-, and remote conditioning. Circ Res 116:674–699. https://doi.org/10.1161/CIRCRESAHA.116.305348
Heusch G (2017) Cardioprotection is alive but remains enigmatic: the nitric oxide-protein kinases-mitochondria signaling axis. Circulation 136:2356–2358. https://doi.org/10.1161/CIRCULATIONAHA.117.031978
Heusch G, Musiolik J, Gedik N, Skyschally A (2011) Mitochondrial STAT3 activation and cardioprotection by ischemic postconditioning in pigs with regional myocardial ischemia/reperfusion. Circ Res 109:1302–1308. https://doi.org/10.1161/CIRCRESAHA.111.255604
Kleinbongard P, Amanakis G, Skyschally A, Heusch G (2018) Reflection of cardioprotection by remote ischemic perconditioning in attenuated st-segment elevation during ongoing coronary occlusion in pigs: evidence for cardioprotection from ischemic injury. Circ Res 122:1102–1108
Klinbongard P, Gedik N, Kirca M, Stoian L, Frey U, Zandi A, Thielmann M, Jakob H, Peters J, Kamler M, Heusch G (2018) Mitochondrial and contractile function of human right atrial tissue in response to remote ischemic conditioning. J Am Heart Assoc 7:e009540. https://doi.org/10.1161/JAHA.118.009540
Kleinbongard P, Skyschally A, Gent S, Pesch M, Heusch G (2017) STAT3 as a common signal of ischemic conditioning: a lesson on “rigor and reproducibility” in preclinical studies on cardioprotection. Basic Res Cardiol. 113:3. https://doi.org/10.1007/s00395-017-0660-z
Kleinbongard P, Skyschally A, Heusch G (2017) Cardioprotection by remote ischemic conditioning and its signal transduction. Pflug Arch 469:159–181. https://doi.org/10.1007/s00424-016-1922-6
Kwong JQ, Lu X, Correll RN, Schwanekamp JA, Vagnozzi RJ, Sargent MA, York AJ, Zhang J, Bers DM, Molkentin JD (2015) The mitochondrial calcium uniporter selectively matches metabolic output to acute contractile stress in the heart. Cell Rep 12:15–22. https://doi.org/10.1016/j.celrep.2015.06.002
Lacerda L, Somers S, Opie LH, Lecour S (2009) Ischaemic postconditioning protects against reperfusion injury via the SAFE pathway. Cardiovasc Res 84:201–208. https://doi.org/10.1093/cvr/cvp274
Lecour S, Suleman N, Deuchar GA, Somers S, Lacerda L, Huisamen B, Opie LH (2005) Pharmacological preconditioning with tumor necrosis factor-alpha activates signal transducer and activator of transcription-3 at reperfusion without involving classic prosurvival kinases (AKT and extracellular signal-regulated kinase). Circulation 112:3911–3918. https://doi.org/10.1161/CIRCULATIONAHA.105.581058
Lee Y, Min CK, Kim TG, Song HK, Lim Y, Kim D, Shin K, Kang M, Kang JY, Youn HS, Lee JG, An JY, Park KR, Lim JJ, Kim JH, Kim JH, Park ZY, Kim YS, Wang J, Kim DH, Eom SH (2015) Structure and function of the N-terminal domain of the human mitochondrial calcium uniporter. EMBO Rep 16:1318–1333. https://doi.org/10.15252/embr.201540436
Lindsey ML, Bolli R, Canty JM Jr, Du XJ, Frangogiannis NG, Frantz S, Gourdie RG, Holmes JW, Jones SP, Kloner RA, Lefer DJ, Liao R, Murphy E, Ping P, Przyklenk K, Recchia FA, Schwartz Longacre L, Ripplinger CM, Van Eyk JE, Heusch G (2018) Guidelines for experimental models of myocardial ischemia and infarction. Am J Physiol Heart Circ Physiol 314:H812–H838. https://doi.org/10.1152/ajpheart.00335.2017
Lu XY, Chen L, Cai XL, Yang HT (2008) Overexpression of heat shock protein 27 protects against ischaemia/reperfusion-induced cardiac dysfunction via stabilization of troponin I and T. Cardiovasc Res 79:500–508. https://doi.org/10.1093/cvr/cvn091
Mallet RT, Manukhina EB, Ruelas SS, Caffrey JL, Downey HF (2018) Cardioprotection by intermittent hypoxia conditioning: evidence, mechanisms, and therapeutic potential. Am J Physiol Heart Circ Physiol 315:H216–H232. https://doi.org/10.1152/ajpheart.00060.2018
Martell JD, Deerinck TJ, Sancak Y, Poulos TL, Mootha VK, Sosinsky GE, Ellisman MH, Ting AY (2012) Engineered ascorbate peroxidase as a genetically encoded reporter for electron microscopy. Nat Biotechnol 30:1143–1148. https://doi.org/10.1038/nbt.2375
McAllister SE, Ashrafpour H, Cahoon N, Huang N, Moses MA, Neligan PC, Forrest CR, Lipa JE, Pang CY (2008) Postconditioning for salvage of ischemic skeletal muscle from reperfusion injury: efficacy and mechanism. Am J Physiol Regul Integr Comp Physiol 295:R681–689. https://doi.org/10.1152/ajpregu.90303.2008
Michels G, Khan IF, Endres-Becker J, Rottlaender D, Herzig S, Ruhparwar A, Wahlers T, Hoppe UC (2009) Regulation of the human cardiac mitochondrial Ca2+ uptake by 2 different voltage-gated Ca2+ channels. Circulation 119:2435–2443. https://doi.org/10.1161/CIRCULATIONAHA.108.835389
Miyawaki H, Wang Y, Ashraf M (1998) Oxidant stress with hydrogen peroxide attenuates calcium paradox injury: role of protein kinase C and ATP-sensitive potassium channel. Cardiovasc Res 37:691–699
Motloch LJ, Reda S, Wolny M, Hoppe UC (2015) UCP2 modulates cardioprotective effects of Ru360 in isolated cardiomyocytes during ischemia. Pharmaceuticals (Basel) 8:474–482. https://doi.org/10.3390/ph8030474
Negoro S, Kunisada K, Fujio Y, Funamoto M, Darville MI, Eizirik DL, Osugi T, Izumi M, Oshima Y, Nakaoka Y, Hirota H, Kishimoto T, Yamauchi-Takihara K (2001) Activation of signal transducer and activator of transcription 3 protects cardiomyocytes from hypoxia/reoxygenation-induced oxidative stress through the upregulation of manganese superoxide dismutase. Circulation 104:979–981
Oropeza-Almazan Y, Vazquez-Garza E, Chapoy-Villanueva H, Torre-Amione G, Garcia-Rivas G (2017) Small interfering RNA targeting mitochondrial calcium uniporter improves cardiomyocyte cell viability in hypoxia/reoxygenation injury by reducing calcium overload. Oxid Med Cell Longev 2017:5750897. https://doi.org/10.1155/2017/5750897
Oshima Y, Fujio Y, Nakanishi T, Itoh N, Yamamoto Y, Negoro S, Tanaka K, Kishimoto T, Kawase I, Azuma J (2005) STAT3 mediates cardioprotection against ischemia/reperfusion injury through metallothionein induction in the heart. Cardiovasc Res 65:428–435. https://doi.org/10.1016/j.cardiores.2004.10.021
Penna C, Mancardi D, Rastaldo R, Pagliaro P (2009) Cardioprotection: a radical view Free radicals in pre and postconditioning. Biochim Biophys Acta 1787:781–793. https://doi.org/10.1016/j.bbabio.2009.02.008
Pierrat B, Ito M, Hinz W, Simonen M, Erdmann D, Chiesi M, Heim J (2000) Uncoupling proteins 2 and 3 interact with members of the 14.3.3 family. Eur J Biochem 267:2680–2687
Piper HM, Meuter K, Schäfer C (2003) Cellular mechanisms of ischemia-reperfusion injury. Ann Thorac Surg 75:S644–648
Rasmussen TP, Wu Y, Joiner ML, Koval OM, Wilson NR, Luczak ED, Wang Q, Chen B, Gao Z, Zhu Z, Wagner BA, Soto J, McCormick ML, Kutschke W, Weiss RM, Yu L, Boudreau RL, Abel ED, Zhan F, Spitz DR, Buettner GR, Song LS, Zingman LV, Anderson ME (2015) Inhibition of MCU forces extramitochondrial adaptations governing physiological and pathological stress responses in heart. Proc Natl Acad Sci USA 112:9129–9134. https://doi.org/10.1073/pnas.1504705112
Sharikabad MN, Ostbye KM, Brors O (2004) Effect of hydrogen peroxide on reoxygenation-induced Ca2+ accumulation in rat cardiomyocytes. Free Radic Biol Med 37:531–538. https://doi.org/10.1016/j.freeradbiomed.2004.05.002
Skyschally A, Kleinbongard P, Lieder H, Gedik N, Stoian L, Amanakis G, Elbers E, Heusch G (2018) Humoral transfer and intramyocardial signal transduction of protection by remote ischemic perconditioning in pigs, rats, and mice. Am J Physiol Heart Circ Physiol. 315:H159–H172. https://doi.org/10.1152/ajpheart.00152.2018
Smith CC, Dixon RA, Wynne AM, Theodorou L, Ong SG, Subrayan S, Davidson SM, Hausenloy DJ, Yellon DM (2010) Leptin-induced cardioprotection involves JAK/STAT signaling that may be linked to the mitochondrial permeability transition pore. Am J Physiol Heart Circ Physiol 299:1265–1270. https://doi.org/10.1152/ajpheart.00092.2010
Sucher R, Gehwolf P, Kaier T, Hermann M, Maglione M, Oberhuber R, Ratschiller T, Kuznetsov AV, Bosch F, Kozlov AV, Ashraf MI, Schneeberger S, Brandacher G, Ollinger R, Margreiter R, Troppmair J (2009) Intracellular signaling pathways control mitochondrial events associated with the development of ischemia/reperfusion-associated damage. Transpl Int 22:922–930. https://doi.org/10.1111/j.1432-2277.2009.00883.x
Sun Y, Deng T, Lu N, Yan M, Zheng X (2010) B-type natriuretic peptide protects cardiomyocytes at reperfusion via mitochondrial calcium uniporter. Biomed Pharmacother 64:170–176. https://doi.org/10.1016/j.biopha.2009.09.024
Szczepanek K, Xu A, Hu Y, Thompson J, He J, Larner AC, Salloum FN, Chen Q, Lesnefsky EJ (2015) Cardioprotective function of mitochondrial-targeted and transcriptionally inactive STAT3 against ischemia and reperfusion injury. Basic Res Cardiol 110:53–63. https://doi.org/10.1007/s00395-015-0509-2
Wang ZH, Chen YX, Zhang CM, Wu L, Yu Z, Cai XL, Guan Y, Zhou ZN, Yang HT (2011) Intermittent hypobaric hypoxia improves postischemic recovery of myocardial contractile function via redox signaling during early reperfusion. Am J Physiol Heart Circ Physiol 301:1695–1705. https://doi.org/10.1152/ajpheart.00276.2011
Wang ZH, Liu JL, Wu L, Yu Z, Yang HT (2014) Concentration-dependent wrestling between detrimental and protective effects of H2O2 during myocardial ischemia/reperfusion. Cell Death Dis 5:e1297. https://doi.org/10.1038/cddis.2014.267
Wegrzyn J, Potla R, Chwae YJ, Sepuri NB, Zhang Q, Koeck T, Derecka M, Szczepanek K, Szelag M, Gornicka A, Moh A, Moghaddas S, Chen Q, Bobbili S, Cichy J, Dulak J, Baker DP, Wolfman A, Stuehr D, Hassan MO, Fu XY, Avadhani N, Drake JI, Fawcett P, Lesnefsky EJ, Larner AC (2009) Function of mitochondrial STAT3 in cellular respiration. Science 323:793–797. https://doi.org/10.1126/science
Wu L, Tan JL, Wang ZH, Chen YX, Gao L, Liu JL, Shi YH, Endoh M, Yang HT (2015) ROS generated during early reperfusion contribute to intermittent hypobaric hypoxia-afforded cardioprotection against postischemia-induced Ca2+ overload and contractile dysfunction via the JAK2/STAT3 pathway. J Mol Cell Cardiol 81:150–161. https://doi.org/10.1016/j.yjmcc.2015.02.015
Yamanaka K, Eldeiry M, Aftab M, Ryan TJ, Roda G, Meng X, Weyant MJ, Cleveland JC Jr, Fullerton DA, Reece TB (2019) Pretreatment with diazoxide attenuates spinal cord ischemia-reperfusion injury through signaling transducer and activator of transcription 3 pathway. Ann Thorac Surg 107:733–739. https://doi.org/10.1016/j.athoracsur.2018.09.031
Yu TN, Hong H, Yang JQ, Gao Q, Xia Q (2011) Role of mitochondrial calcium uniporter in cardioprotection induced by ischemic postconditioning in isolated rat heart. Zhejiang Da Xue Xue Bao Yi Xue Ban 40:304–308
Zhang L, Wang S, Dong H, Li Y, Wang P, Li S, Guo Y, Yao R (2014) Spermine attenuates the preconditioning of diazoxide against transient focal cerebral ischemia in rats. Neurol Res 36:666–672. https://doi.org/10.1179/1743132813Y.0000000299
Zhang J, Chen FJ, Li WL, Xiong Q, Yang MK, Zheng P, Li CY, Pei JF, Ge F (2012) 14-3-3zeta interacts with STAT3 and regulates its constitutive activation in multiple myeloma cells. PLoS One 7:e29554. https://doi.org/10.1371/journal.pone.0029554
Zhang SZ, Gao Q, Cao CM, Bruce IC, Xia Q (2006) Involvement of the mitochondrial calcium uniporter in cardioprotection by ischemic preconditioning. Life Sci 78:738–745. https://doi.org/10.1016/j.lfs.2005.05.076
Zhu WZ, Xie Y, Chen L, Yang HT, Zhou ZN (2006) Intermittent high altitude hypoxia inhibits opening of mitochondrial permeability transition pores against reperfusion injury. J Mol Cell Cardiol 40:96–106. https://doi.org/10.1016/j.yjmcc.2005.09.016
Acknowledgements
This work was supported by National Natural Sciences Foundation of China (81600246), Shanghai Excellent Young Teachers Funding Project (zzjkyx16004) and Shanghai Municipal Education Commission (Plateau Disciplinary Program for Medical Technology of SUMHS, 2018-2020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, L., Tan, JL., Chen, ZY. et al. Cardioprotection of post-ischemic moderate ROS against ischemia/reperfusion via STAT3-induced the inhibition of MCU opening. Basic Res Cardiol 114, 39 (2019). https://doi.org/10.1007/s00395-019-0747-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-019-0747-9