Abstract
Background
Metabolic syndrome (MetS) is a clinical syndrome characterized by multiple metabolic disorders and is a serious global health problem. The coffee effect, acting as one of the most prevalent beverages on metabolic syndrome, is debatable.
Methods
We included patients from the National Health and Nutrition Examination Survey 2003–2018 and used a comprehensive evaluation called the MetS z-score to assess the severity of metabolic syndrome. The relationship between coffee, decaffeinated coffee, tea, and MetS z-scores was explored using a weighted linear regression. We also divided the participants into metabolic and non-metabolic syndrome groups according to the NCEP/ATP III criteria for the subgroup analysis.
Results
A total of 14,504 participants were included in this study. The results demonstrated that drinking more than three cups of coffee daily was significantly linked to lower MetS z-scores (p < 0.001). Daily coffee consumption was also associated with lower BMI (p = 0.02), systolic blood pressure (p < 0.001), Homeostatic Model Assessment for Insulin Resistance (p < 0.001), and triglycerides (p < 0.001), while it was positively correlated with HDL-C (p = 0.001). Participants who consumed more than three cups of coffee daily had a lower MetS z-score in the MetS (p < 0.001) and non-MetS (p = 0.04) groups.
Conclusion
This research indicates that coffee consumption is linked to MetS severity. However, decaffeinated coffee and tea intake were unrelated to MetS severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS) is characterized by high fasting plasma glucose, abdominal obesity, high blood pressure, low high-density lipoprotein cholesterol (HDL-C), and high serum triglyceride levels. The present MetS definition is inconsistent. Several researchers have expounded that the five definitions of metabolic syndrome are similar in their prognostic and management effectiveness. The National Cholesterol Education Program (NCEP/ATPIII) definition is the most widespread [1]. Although the mechanism is unknown, the underlying pathophysiology may be related to insulin resistance [2]. The high prevalence, morbidity, and poor prognosis of MetS have made it a major socioeconomic burden on global public health systems [3,4,5]. Consequently, MetS evaluation is important. Current methods focus on individually assessing each MetS component to determine its severity; however, their accuracy is limited because of the interdependence of the component factors. The MetS z-score, an emerging assessment tool, quantifies MetS components by sex and ethnicity to produce a total score to assess MetS status, which is already considered to have potential clinical applications [6]. In addition to pharmacological treatment, lifestyle modifications (e.g., smoking cessation, alcohol cessation, adequate sleep, and a balanced diet) are among the major treatment modalities [7]. Because dietary structure modification as part of lifestyle intervention affects blood glucose, obesity, lipids, and blood pressure, it is considered the primary preventive intervention [2]. As one of the most prevalent beverages worldwide, coffee embodies social norms and cultural traditions to some extent. Several studies have investigated the link between coffee intake and MetS risk by its widespread consumption; however, the results are contradictory. A population-based prospective cohort study that included 9514 middle-aged adults found no relationship between MetS incidence and coffee consumption [8]. Similarly, the Tianliao Old People (TOP) study that included elderly men in remote areas of China did not suggest a significant association between MetS and coffee consumption [9]. A Polish population study examining the relationship between coffee and MetS using a food frequency questionnaire displayed that coffee was linked to a reduced risk of MetS [10]. Another retrospective study from Japan that included participants older than 40 years suggested that coffee consumption was inversely correlated with MetS [11]. These diverse results might be due to option bias in the study population (middle-aged adults and elderly males) and study designs (cross-sectional surveys and using a food frequency questionnaire rather than a 24-hour dietary review). Furthermore, quantifying the severity of MetS is more beneficial for healthy population prevention and management of MetS patients than determining whether the patient is at risk. However, no correlation between MetS severity and coffee consumption has been established without validated assessment tools. Our study included a representative population of US adults and used a 24-hour dietary review to collect their dietary data, whereas we used the MetS z-score as a tool to quantify the severity of metabolic syndrome. This made our findings more reliable.
To explore the association between MetS severity and coffee consumption in this study, we assessed MetS severity using the MetS BMI z-score in a nationally representative and large American cohort and obtained dietary intake data using the gold criteria of nutritional epidemiology and two 24-hour dietary recalls.
Materials and methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is a population-based survey program implemented by the National Center for Health Statistics (NCHS) with a two-year cycle since 1971. Participants were enrolled using an oversampling device and multistage probability, allowing for a weighted dissection presenting the health and nutritional status of the non-institutional U.S. population.
Socioeconomic, demographic, dietary, and health information was initially gathered in a mobile examination center (MEC) through interviews. Interviewers who have gone through one week of strict training collected the second 24-hour dietary recall by telephone interview 3–10 days later. In this way, two 24-hour dietary recalls were completed in collaboration with the U.S. Department of Agriculture (USDA) and Health and Human Services. A subset of participants underwent additional laboratory tests, examinations, and questionnaires.
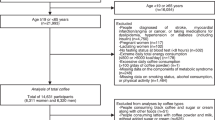
A secondary data analysis of eight consecutive NHANES cycles from 2003 to 2018 was conducted. We included 20 years old and above participants with a complete MetS z-score component, and 14,504 participants were selected. The cohort construction flowchart is displayed in Supplementary Fig. 1.
Assessment of MetS severity
Numerous studies have been conducted to evaluate each MetS component individually; however, determining MetS severity in this manner is difficult. In contrast, confirmatory factor analysis was used to calculate MetS z-scores for various MetS components. Unlike traditional MetS definitions, which establish separate thresholds for its components, MetS z-score is calculated by assigning values to the MetS components and summing them, allowing MetS z-score to recognize the crucial MetS state (for example, a dieting triglyceride level of 1.69 mmol/L while the amount of cutoff reaches 1.7 mmol/L). Moreover, considering the effects of sex and race/ethnicity on MetS, the MetS z-score has different algorithms for different sex and race/ethnicity populations to eliminate this bias.
The MetS z-score was derived from a nationally representative population in the U.S. (NHANES). Similar to other z-scores, it is the number of standard deviations from the mean American population.
We divided patients into MetS and non-MetS groups according to the NCEP/ATP III, one of the widely used MetS criteria, to separately observe the effect of coffee on metabolic levels in MetS patients and normal subjects.
Prescription medications were collected by drilled interviewers using a Computer-Assisted Personal Interview (CAPI) mechanism. In addition to body mass index (BMI), fasting glucose, triglycerides, HDL-C level, and waist were examined in the MEC. Aside from the diastolic blood pressure, the systolic blood pressure was averaged after four measurements.
Dietary intake assessment
Dietary intake data were gathered through dietary interviews in the form of 24-hour dietary retrospection. Nutrients and energy in food/beverages and their categorization were derived from USDA’s Food and Nutrient Database for Dietary Studies. In this study, tea, decaffeinated coffee, and coffee consumption were converted to six ounces per serving and classified by the number of cups consumed (non-drinkers: 0–1, 1–2, 2–3, or > 3 cups/day). Fat, cholesterol, and sugar of any origin claimed by the participants were converted to milligrams. All substances consumed during the day were converted into energy intake and recorded.
Covariates
Education level (below high school, high school, some college, and college), low-density lipoprotein cholesterol (LDL-C), poverty-income ratio (PIR), waist circumference, age, fasting insulin, smoking exposure (smoked at least 100 cigarettes during lifetime), alcohol exposure (not less than 12 alcohol drinks yearly or not), daily fat, cholesterol, sugar, and total energy intake were introduced as potential covariates that may affect MetS severity. The euglycemic insulin clamp technique is the gold standard for measuring insulin resistance [12]. However, this method has not yet been widely used because of its limited clinical applications. The homeostatic model assessment for insulin resistance (HOMA-IR) has been developed recently and is widely used (fasting glucose × fasting insulin/22.5) as an alternative insulin resistance or sensitivity measure [13]. Apart from HOMA-IR, insulin levels were employed to evaluate insulin resistance in the study. To clarify the unique effects of caffeine and coffee on metabolic syndrome, tea consumption, and decaffeinated coffee were used as controls. We also divided the participants into four groups: non-drinker, coffee-only, decaffeinated coffee-only, tea-only, and mixed-drink groups. Since the MetS z-score is produced by ethnicity/race, BMI, sex, fasting glucose, systolic blood pressure, triglycerides, and HDL-C, they were not included as covariates in the pattern, with the z-score as the dependent variable.
Statistical analysis
Statistical dissections were implemented using R version 3.4.3 and STATA (version 17.0), with two-tailed p < 0.01, showing statistical significance. For the study population to be nationally representative, all statistical analyses were weighted, and the novel sample weight (original two-year sample weight split by eight) was calculated using the NHANES Analytic Guidelines. Categorical variables were expressed as proportions with 95% confidence interval (95% CI), whereas continuous variables were expressed as mean and standard error. The chi-square test was used for categorical variables, and weighted linear regression was used for group comparisons.
Weighted linear regression was used in the current study to determine the connections between decaffeinated coffee, tea, coffee, and MetS z-scores in three different models. The coefficients were standardized to make the results more practical and avoid the bias associated with large sample sizes. In the first model, model 1, no variables were adjusted. We then introduced education, age, PIR, and waist circumference in model 2 based on model (1) Finally, the covariates in the fully adjusted model (model 3) included LDL-C, fasting insulin, smoking exposure, drinking status, and daily fat, cholesterol, sugar, and total energy intake, as well as those regulated in model (2) Furthermore, we investigated the effect of coffee on participants with and without metabolic syndrome using the NCEP/ATP III. Weighted multivariate regression was also performed for fasting glucose, triglycerides, HOMA-IR, HDL-C, systolic pressure, and BMI as dependent variables to explore how coffee affects metabolic syndrome severity.
Results
Demographic information and clinical features
The clinical and sociodemographic features of 14,504 participants are depicted in Table 1. Participants were 47.29 ± 0.17 years old, 49% were males, 73.7% were white, and 28.2% received a college education or higher. Approximately 77.4% of all participants had at least one drink in the past year, whereas 46.3% smoked more than 100 cigarettes in their lifetime. The weighted mean PIR, MetS z-score, systolic blood pressure, and waist circumference were 2.98 ± 0.02, 0.15 ± 0.01, 121.2 ± 17 mmHg, and 99.54 ± 0.18 cm, respectively. Statistically significant differences were observed (p < 0.01) in the allocation of age, sex, race, educational level, PIR, BMI, smoking status, waist circumference, systolic blood pressure, MetS z-score, and daily fat, cholesterol, sugar, and total energy intake between individuals with different coffee intakes (Table 1). There was no significant difference in the MetS z-score (p = 0.56) between individuals with different decaffeinated coffee consumptions (Supplementary Table 1). In contrast, people who consumed different amounts of tea had an elevated MetS z-score (p < 0.001, Supplementary Table 2). Participants were divided into non-MetS and MetS teams based on the NCEP/ATP III, and an obvious connection was observed between lower education level and MetS, severe insulin resistance status (HOMA-IR), lower PIR, and female sex (p < 0.001, Supplementary Table 3).
Association between MetS z-score and coffee, decaffeinated coffee, and tea consumption
We introduced different covariates to detect the connection between MetS severity and coffee consumption, while tea and coffee served as control groups to reduce study bias. In pattern 1, blessed with the unadjusted variables (Supplementary Table 4), drinking 2–3 cups of tea (p = 0.003) and > 3 cups of coffee (p = 0.002) were linked to a lower MetS z-score than non-drinkers, while daily tea intake of more than three cups was associated with an elevated MetS z-score. Behind the adjustment for education level, PIR, age, and waist circumference in model 2, only consuming over three cups daily was linked to a lower MetS z-score than non-drinkers. We considered all confounding variables mentioned in the inside method section of the fully adjusted model, model 3, and observed similar results to model 2 (Table 2). In addition to coffee consumption and higher educational level (p < 0.01), PIR (p < 0.001) was correlated with a lower MetS z-score.
We explored the association between various components of MetS z-score and coffee intake to determine the role of coffee in MetS severity (Table 3). In the multivariate-adjusted analysis, a daily coffee intake of > 3 cups was associated with a lower BMI (p = 0.02), HOMA-IR(p < 0.001), systolic blood pressure (p < 0.001), and triglycerides (p < 0.001) among all participants, whereas HDL-C was positively correlated with a daily coffee intake of more than three cups (p = 0.001). Considering the potential effect of insulin resistance on MetS [2], we also performed a correlation analysis between HOMA-IR and coffee intake and discovered a negative correlation between the daily intake of more than one cup of coffee and HOMA-IR in all participants.
Subgroup analysis
We implemented a weighted linear regression using multiple variable adjustments for the MetS z-score in the two teams based on the presence or absence of MetS. In addition to the demographic data, the clinical characteristics are illustrated in Supplementary Table 3. Participants who consumed more than three cups of coffee daily were, in turn, linked to a lower MetS z-score with tea and decaffeinated coffee as controls (p < 0.001) in the MetS group (Table 4). Moreover, educational level (p < 0.01) was associated with a lower MetS z-score. Individuals who had consumed at least 12 drinks in the previous year (p < 0.01) had high MetS z-scores. The daily intake of more than three cups of coffee was also linked to low z-scores (p = 0.04) in participants without MetS (Table 5) compared with non-drinkers (no statistically significant difference existed); nevertheless, no obvious connection was observed for decaffeinated coffee or tea consumption. Similar to the metabolic syndrome group, high PIR (p = 0.02), college education or higher (p < 0.001), and no alcohol exposure (p < 0.001) were associated with a lower MetS z-score for coffee consumption. We conducted a correlation study between fasting glucose, BMI, HDL-C, HOMA-IR, systolic blood pressure, triglyceride levels, and coffee consumption (Table 3). Coffee intake of more than three cups daily was linked to lower systolic blood pressure (p = 0.003), HOMA-IR (p = 0.005), and triglycerides (p = 0.001) in the MetS group; however, only systolic blood pressure (p < 0.001) and triglycerides (p = 0.03) remained the same in the healthy group. When the participants were categorized into non-drinker, coffee-only, tea-only, and mixed-drink groups, the MetS Z-score was lower among participants in the coffee-only group (p = 0.004) than among non-drinkers (Supplementary Table 5).
Considering that different teas contain different caffeine amounts, we categorized the tea-drinking participants into green tea and black tea groups. The results suggest that although the two teas contain different caffeine amounts, neither of them had a statistically significant effect on metabolic syndrome (Supplementary Table 6).
Depending on the preparation method of the coffee, we categorized the patients into three groups: brewed, instant, and mixed-drink groups. After adjusting for the same variables as in model 3, participants who drank brewed coffee had a lower severity of metabolic syndrome compared with instant coffee (Supplementary Table 6). However, we did not find that participants who drank both types of coffee had a higher or lower severity of metabolic syndrome.
Sensitivity analysis
Considering previous research concerning the impact of tea and coffee on metabolic syndrome and their same composition as coffee [14], we used model 3 to adjust for decaffeinated coffee and tea as independent variables for sensitivity analysis (Supplementary Table 7). The results demonstrated that participants with more than three cups of coffee daily had a lower z-score inside the newly constructed model, consistent with model 3 (p < 0.001, p < 0.001, and p = 0.01 for all MetS patients and healthy participants, respectively). MetS z-score had no significant association with the other stratified drinking categories. Furthermore, because of the significant connection between the MetS z-score and coffee in the current models, but not decaffeinated coffee, the relationship between daily caffeine consumption and MetS z-score was investigated. We categorized caffeine consumption into three groups: non-drinkers, 0–100 mg/day, and > 100 mg/day. We then adjusted for related covariates, as in model 3, for daily caffeine intake in all participants, MetS, and healthy participants (Supplementary Table 8). Nevertheless, no obvious differences were observed between the caffeine consumption groups.
Discussion
Numerous studies have provided evidence for MetS prevention by investigating the influence of coffee on MetS risk [8, 10, 15, 16]. However, the bias introduced by the study design and subject selection in observational studies makes the correlation between metabolic syndrome and coffee inconsistent across studies. Therefore, unlike previous studies, we selected a diverse and nationally representative population and determined dietary intake using two 24-hour dietary retrospections (the gold criteria for nutrition epidemiology). The severity of MetS and the influence of coffee on MetS were evaluated in this study. Third, we included tea and decaffeinated coffee as controls and performed a sensitivity analysis to make the results of this study more reliable. Ultimately, we discovered a reproducible connection between reduced severity of MetS and coffee in participants with or without MetS. To the best of our knowledge, this is the first research that focuses on coffee consumption and MetS severity.
Coffee is negatively linked to insulin resistance. Coffee consumption was evidently linked to a reduction in HOMA-IR in overweight participants (BMI ≥ 25 kg/m2) in a Japanese population-based cross-sectional epidemiological study [17]. A recent meta-analysis including four randomized controlled trials (RCTs) reported that coffee consumption could significantly lower HOMA-IR levels [18]. Although the potential relationship between insulin resistance and coffee consumption is not fully understood, this effect is believed to occur through three different mechanisms. First, chlorogenic acid-rich coffee was shown to lower blood glucose levels in a rat model, and quinides derived from chlorogenic acid were observed to improve insulin sensitivity [19]. Second, because systemic inflammation and oxidative pressure are closely connected to insulin resistance pathogenesis [20, 21], the antioxidant and anti-inflammatory properties of coffee prevent the development of insulin resistance [22, 23]. Third, magnesium—one of the main trace elements in coffee—is negatively associated with insulin resistance [24, 25]. We used HOMA-IR as a measure of insulin resistance in the current study and discovered that daily coffee of over three cups was inversely linked to HOMA-IR. This observation is consistent with that of previous studies. This may be because MetS patients are prone to inflammation and oxidative stress.
Consuming over three cups of coffee daily was apparently and inversely associated with systolic blood pressure in participants with or without MetS in the current study. Considering the widespread consumption of coffee and the socioeconomic burden of hypertension, the interaction between coffee consumption and blood pressure has been the subject of extensive research. A dose-response meta-analysis revealed that increased intake was linked to a reduced risk of hypertension [26]. A recent Brazilian prospective study enrolled 8,780 participants without hypertension and discovered that intake reduced the risk of hypertension [27]. Another recent finding from the Brisighella Heart Study also demonstrated that regular coffee drinking is linked to lower systolic blood pressure [28]. However, another meta-analysis, including 11 clinical controlled trials, suggested a slight increase in blood pressure with increased coffee consumption [29]. This inconsistency in the study results may be related to the chronic effects of caffeine on blood pressure. A systemic review indicated that eight RCTs caused a sharp increase in blood pressure more than three hours after administration, whereas no significant increase was observed for long-term intervention [30]. Therefore, although coffee intake may temporarily increase blood pressure, there is no conclusive evidence that regular coffee intake intensifies the hazard of hypertension over time. We used nationally representative data from this study and discovered that coffee intake was linked to lower systolic blood pressure than non-drinkers. In addition to solid data and rigorous collection methods for coffee intake and blood pressure, the results may be explained by the following two factors. First, caffeine acts as an immunomodulatory agent by participating in both intrinsic and adaptive immune processes [23], which may reduce the effects of inflammatory states on endothelial cells and the renin system [31, 32], especially in MetS patients. Second, other compounds in coffee also have antihypertensive effects, such as ferulic acid, which increases the bioavailability of nitric oxide to restore endothelial function [33], and phenolic compounds (chlorogenic acid and caffeic acid), which act as antioxidants to achieve dilatation [24]. The preparation method of the coffee was also one of the factors influencing the severity of metabolic syndrome in our subgroup analyses, which may be related to chlorogenic acid. One study demonstrated that 180 mL of brewed coffee provided more polyphenols than instant coffee (396 vs. 316 mg) [34].
Furthermore, we discovered that coffee affects blood lipid levels, particularly triglycerides. Dyslipidemia is an important metabolic syndrome characterized by high triglyceride and low HDL-C levels. The impact of coffee on lipid metabolism is complicated and varies with composition. Cafestol, a lipidic compound in coffee, reduces bile acid synthesis by affecting the activity of rate-limiting enzymes in the bile acid synthesis pathway and by increasing cholesterol [35]. The residual caffeine content was low after filtration. Therefore, unfiltered coffee increases plasma cholesterol levels [36]. In addition to the ingredients responsible for elevated blood lipids, animal studies have revealed that chlorogenic acid has anti-lipidemic properties [37]. The effect of coffee on blood lipid composition is difficult to determine, and a series of clinical studies have been conducted. Zhou et al. studied 362,571 UK Biobank participants to investigate the association between plasma lipid profiles and coffee consumption [38]. They discovered that participants who drank up to three cups of coffee daily had lower plasma triglyceride concentrations than non-habitual drinkers, consistent with our findings. However, a recent meta-analysis of 12 RCTs examined the connections between coffee consumption and whole cholesterol, LDL-C, and triglycerides and demonstrated that they were positively correlated [37].
The correlation between coffee consumption and metabolic syndrome severity was evaluated using z-scores. The underlying mechanisms, including the effects of coffee and its components on metabolic syndrome, were also investigated. However, it is important to recognize that metabolic syndrome is a collection of five interrelated symptoms; consequently, it must be viewed holistically. Further clinical and basic studies are demanded to identify the mechanisms by which coffee affects MetS severity.
However, this study has some limitations. First, this was a cross-sectional study that constrained causal inferences; accordingly, it was difficult to generalize the results of this study to a causal relationship between coffee consumption and MetS severity. Next, we did not categorize coffee according to bean sort and roasting, which are important factors that affect the amount of active ingredients in coffee. Furthermore, with a very large sample, even small differences can reach statistical significance, and there is also the possibility of over-emphasizing statistical significance without proper consideration of the effect sizes. Although utilizing the MetS z-score for deciding a patient’s MetS hazard might not be the most integrated, some studies have illustrated the reliability of the scoring mechanism [6, 39].
Conclusion
Daily intake of more than three cups of coffee was linked to lower MetS severity. This may be related to the beneficial effects of coffee on insulin resistance, blood lipid levels, and blood pressure.
References
Ferraz-Amaro I, Gonzalez-Juanatey C, Lopez-Mejias R, Riancho-Zarrabeitia L, Gonzalez-Gay MA (2013) Metabolic syndrome in rheumatoid arthritis. Mediators Inflamm 2013(710928). https://doi.org/10.1155/2013/710928
Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Van Pelt RE, Wang H, Eckel RH (2008) The metabolic syndrome. Endocr Rev 29(7):777–822. https://doi.org/10.1210/er.2008-0024
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365(9468):1415–1428. https://doi.org/10.1016/s0140-6736(05)66378-7
Scholze J, Alegria E, Ferri C, Langham S, Stevens W, Jeffries D, Uhl-Hochgraeber K (2010) Epidemiological and economic burden of metabolic syndrome and its consequences in patients with hypertension in Germany, Spain and Italy; a prevalence-based model. BMC Public Health 10:529. https://doi.org/10.1186/1471-2458-10-529
Wu SH, Liu Z, Ho SC (2010) Metabolic syndrome and all-cause mortality: a meta-analysis of prospective cohort studies. Eur J Epidemiol 25(6):375–384. https://doi.org/10.1007/s10654-010-9459-z
DeBoer MD, Filipp SL, Gurka MJ (2018) Use of a metabolic syndrome severity Z score to Track Risk during Treatment of prediabetes: an analysis of the Diabetes Prevention Program. Diabetes Care 41(11):2421–2430. https://doi.org/10.2337/dc18-1079
Shang F, Li X, Jiang X (2016) Coffee consumption and risk of the metabolic syndrome: a meta-analysis. Diabetes Metab 42(2):80–87. https://doi.org/10.1016/j.diabet.2015.09.001
Lutsey PL, Steffen LM, Stevens J (2008) Dietary intake and the development of the metabolic syndrome: the atherosclerosis risk in communities study. Circulation 117(6):754–761. https://doi.org/10.1161/circulationaha.107.716159
Chang CS, Chang YF, Liu PY, Chen CY, Tsai YS, Wu CH (2012) Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: the Tianliao old people (TOP) study 02. PLoS ONE 7(6):e38874. https://doi.org/10.1371/journal.pone.0038874
Grosso G, Stepaniak U, Micek A, Topor-Mądry R, Pikhart H, Szafraniec K, Pająk A (2015) Association of daily coffee and tea consumption and metabolic syndrome: results from the Polish arm of the HAPIEE study. Eur J Nutr 54(7):1129–1137. https://doi.org/10.1007/s00394-014-0789-6
Hino A, Adachi H, Enomoto M, Furuki K, Shigetoh Y, Ohtsuka M, Kumagae S, Hirai Y, Jalaldin A, Satoh A, Imaizumi T (2007) Habitual coffee but not green tea consumption is inversely associated with metabolic syndrome: an epidemiological study in a general Japanese population. Diabetes Res Clin Pract 76(3):383–389. https://doi.org/10.1016/j.diabres.2006.09.033
Tam CS, Xie W, Johnson WD, Cefalu WT, Redman LM, Ravussin E (2012) Defining insulin resistance from hyperinsulinemic-euglycemic clamps. Diabetes Care 35(7):1605–1610. https://doi.org/10.2337/dc11-2339
Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A (2015) Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metabol 19(1):160–164. https://doi.org/10.4103/2230-8210.146874
Sae-tan S, Grove KA, Lambert JD (2011) Weight control and prevention of metabolic syndrome by green tea. Pharmacol Res 64(2):146–154. https://doi.org/10.1016/j.phrs.2010.12.013
Hino A, Adachi H, Enomoto M, Furuki K, Shigetoh Y, Ohtsuka M, Kumagae S-I, Hirai Y, Jalaldin A, Satoh A, Imaizumi T (2007) Habitual coffee but not green tea consumption is inversely associated with metabolic syndrome: an epidemiological study in a general Japanese population. Diabetes Res Clin Pract 76(3):383–389. https://doi.org/10.1016/j.diabres.2006.09.033
Chang C, Chang Y, Liu P, Chen C, Tsai Y, Wu C (2012) Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: the Tianliao old people (TOP) study 02. PLoS ONE 7(6):e38874. https://doi.org/10.1371/journal.pone.0038874
Pham NM, Nanri A, Kochi T, Kuwahara K, Tsuruoka H, Kurotani K, Akter S, Kabe I, Sato M, Hayabuchi H, Mizoue T (2014) Coffee and green tea consumption is associated with insulin resistance in Japanese adults. Metabolism 63(3):400–408. https://doi.org/10.1016/j.metabol.2013.11.008
Moon SM, Joo MJ, Lee YS, Kim MG (2021) Effects of Coffee consumption on insulin resistance and sensitivity: a Meta-analysis. Nutrients 13(11). https://doi.org/10.3390/nu13113976
van Dam RM, Hu FB (2005) Coffee consumption and risk of type 2 DiabetesA. Syst Rev JAMA 294(1):97–104. https://doi.org/10.1001/jama.294.1.97
Shoelson SE, Herrero L, Naaz A (2007) Obesity, inflammation, and insulin resistance. Gastroenterology 132(6):2169–2180. https://doi.org/10.1053/j.gastro.2007.03.059
Henriksen EJ, Diamond-Stanic MK, Marchionne EM (2011) Oxidative stress and the etiology of insulin resistance and type 2 diabetes. Free Radic Biol Med 51(5):993–999. https://doi.org/10.1016/j.freeradbiomed.2010.12.005
Yashin A, Yashin Y, Wang JY, Nemzer B (2013) Antioxidant and antiradical activity of coffee. Antioxid (Basel) 2(4):230–245. https://doi.org/10.3390/antiox2040230
Sharif K, Watad A, Bragazzi NL, Adawi M, Amital H, Shoenfeld Y (2017) Coffee and autoimmunity: more than a mere hot beverage! Autoimmun Rev 16(7):712–721. https://doi.org/10.1016/j.autrev.2017.05.007
Higdon JV, Frei B (2006) Coffee and health: a review of recent human research. Crit Rev Food Sci Nutr 46(2):101–123. https://doi.org/10.1080/10408390500400009
Kim DJ, Xun P, Liu K, Loria C, Yokota K, Jacobs DR Jr., He K (2010) Magnesium intake in relation to systemic inflammation, insulin resistance, and the incidence of diabetes. Diabetes Care 33(12):2604–2610. https://doi.org/10.2337/dc10-0994
Grosso G, Micek A, Godos J, Pajak A, Sciacca S, Bes-Rastrollo M, Galvano F, Martinez-Gonzalez MA (2017) Long-term coffee consumption is Associated with decreased incidence of New-Onset Hypertension: a dose-response Meta-analysis. Nutrients 9(8). https://doi.org/10.3390/nu9080890
Miranda AM, Goulart AC, Benseñor IM, Lotufo PA, Marchioni DM (2021) Coffee consumption and risk of hypertension: a prospective analysis in the cohort study. Clin Nutr 40(2):542–549. https://doi.org/10.1016/j.clnu.2020.05.052
Cicero AFG, Fogacci F, D’Addato S, Grandi E, Rizzoli E, Borghi C, Study obotBH (2023) Self-reported Coffee Consumption and Central and Peripheral Blood pressure in the cohort of the Brisighella Heart Study. Nutrients 15(2):312
Jee SH, He J, Whelton PK, Suh I, Klag MJ (1999) The effect of chronic coffee drinking on blood pressure: a meta-analysis of controlled clinical trials. Hypertension 33(2):647–652. https://doi.org/10.1161/01.hyp.33.2.647
Mesas AE, Leon-Muñoz LM, Rodriguez-Artalejo F, Lopez-Garcia E (2011) The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr 94(4):1113–1126. https://doi.org/10.3945/ajcn.111.016667
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle DA (2002) Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation 105(16):1890–1896. https://doi.org/10.1161/01.cir.0000015126.83143.b4
Wang CH, Li SH, Weisel RD, Fedak PW, Dumont AS, Szmitko P, Li RK, Mickle DA, Verma S (2003) C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation 107(13):1783–1790. https://doi.org/10.1161/01.Cir.0000061916.95736.E5
Suzuki A, Yamamoto M, Jokura H, Fujii A, Tokimitsu I, Hase T, Saito I (2007) Ferulic acid restores endothelium-dependent vasodilation in aortas of spontaneously hypertensive rats. Am J Hypertens 20(5):508–513. https://doi.org/10.1016/j.amjhyper.2006.11.008
Godos J, Pluchinotta FR, Marventano S, Buscemi S, Li Volti G, Galvano F, Grosso G (2014) Coffee components and cardiovascular risk: beneficial and detrimental effects. Int J Food Sci Nutr 65(8):925–936. https://doi.org/10.3109/09637486.2014.940287
Wahrburg U, Martin H, Schulte H, Walek T, Assmann G (1994) Effects of two kinds of decaffeinated coffee on serum lipid profiles in healthy young adults. Eur J Clin Nutr 48(3):172–179
Whayne TF Jr (2015) Coffee: a selected overview of Beneficial or Harmful effects on the Cardiovascular System? Curr Vasc Pharmacol 13(5):637–648
Du Y, Lv Y, Zha W, Hong X, Luo Q (2020) Effect of coffee consumption on dyslipidemia: a meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis 30(12):2159–2170. https://doi.org/10.1016/j.numecd.2020.08.017
Zhou A, Hyppönen E (2021) Habitual coffee intake and plasma lipid profile: evidence from UK Biobank. Clin Nutr 40(6):4404–4413. https://doi.org/10.1016/j.clnu.2020.12.042
DeBoer MD, Filipp SL, Sims M, Musani SK, Gurka MJ (2020) Risk of ischemic stroke increases over the spectrum of metabolic syndrome severity. Stroke 51(8):2548–2552. https://doi.org/10.1161/strokeaha.120.028944
Acknowledgements
We thank the staff of the National Centers for Health Statistics of the Centers for Disease Control for designing, collecting, and managing the NHANES data and releasing the data available to the public.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 82071841), the National Natural Science Foundation of China (Grant No. 81901667), and the National High-Level Hospital Clinical Research Funding (Grant No. 2022-PUMCH-B-044).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Informed consent
The NHANES was approved by the Institutional Review Board of the NCHS, and written informed consent was obtained from each participant.
Conflict of interest
The authors declare no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, H., Wang, S., Han, Y. et al. Coffee consumption might be associated with lower potential risk and severity of metabolic syndrome: national health and nutrition examination survey 2003–2018. Eur J Nutr 63, 1705–1718 (2024). https://doi.org/10.1007/s00394-024-03367-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-024-03367-1