Abstract
Purpose
Non-alcoholic fatty liver disease (NAFLD) is a complex disease, resulting from a variety of genetic and environmental factors. The aim of this case–control study was to evaluate the effect of selected genetic polymorphisms, nutrition aspects and their interaction on the risk of NAFLD.
Methods
The sample consisted of 134 patients with NAFLD and 217 controls. Disease was diagnosed by liver ultrasound and volunteers were clinically and nutritionally assessed. Food groups were extracted from a 172 food-item FFQ questionnaire. Three genetic polymorphisms were assessed: PNPLA3 rs738409, TM6SF2 rs58542926 and GCKR rs780094.
Results
We replicated the effect of previously reported risk factors for NAFLD, such as elevated liver enzymes, obesity and metabolic syndrome. Food groups rich in simple sugars, fat and especially saturated fat were positively associated with NAFLD risk, whereas food groups rich in polyunsaturated fatty acids were reversely associated with the possibility of developing the disease (p < 0.05). Only the PNPLA3 genetic variant was statistically significantly associated with the disease (padditive = 0.015). However, it was found that a one-portion increase in fish intake increased the risk of NAFLD in carriers of the risk allele of TM6SF2 rs58542926 polymorphism compared to non-carriers, after adjusting for age, gender, energy intake, pack-years, PAL, TM6SF2 genotype and fish consumption (ORdominant = 1.503, 95% CI 1.094–2.064).
Conclusions
Fish intake exerts an additive effect on NAFLD risk for carriers of the TM6SF2 polymorphism. This novel finding provides further rationale on the need for personalized nutritional advice, based on the genetic background of NAFLD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of non-alcoholic fatty liver disease (NAFLD) shows an upward trend, in parallel with the prevalence of obesity and type 2 diabetes mellitus (T2DM) [1]. NAFLD is believed to be the hepatic manifestation of the metabolic syndrome (MetS) and its pathophysiology is complex [2]. It is a multifactorial disease and the mechanisms involved in its pathophysiology constitute a combination of genetic predisposition and environmental factors.
In addition to established risk factors, such as age, body mass index (BMI) and gender, a polygenic background is believed to confer susceptibility to the onset and progression of NAFLD [3]. In 2008, a large GWAS by Romeo et al. demonstrated the significant role of the PNPLA3 gene in NAFLD pathogenesis [4]. Since then, several other NAFLD-related genes have been identified. To date, there are three genetic variants that have been robustly identified as risk factors for NAFLD: PNPLA3 rs738409 (C>G), TM6SF2 rs58542926 (C>T) and GCKR rs780094 (C>T). PNPLA3 protein (adiponutrin) is believed to act as a triacylglycerol lipase, with its exact role still being under investigation. The steatotic effect of PNPLA3 is independent of the presence of MetS [4]. TM6SF2 protein is believed to participate in the regulation of hepatic triglyceride (TG) secretion and thus impaired function of the protein has been linked to NAFLD [5, 6]. GCKR encodes a glucokinase regulator. Impaired function of GCKR results in uncontrolled glucose influx in the hepatocytes, which up-regulates de-novo lipogenesis and liver steatosis [7].
Lifestyle modifications could counteract the negative effect of genetics [8]. A healthy diet, especially a diet low in fat and saturated fatty acids, low in sugars, high in fibers and antioxidants, has been negatively associated with hepatic steatosis and inflammation. Therefore, patients diagnosed or at high risk for NAFLD should be primarily advised for dietary modifications.
Considering the multifactorial background and the various gene–environment interactions that lead to NAFLD onset and progression, it becomes quite important to explore potential gene–diet interactions. Unravelling gene–diet interactions in NAFLD onset and progression may constitute the key to the application of personalized nutrition and, therefore, provide patients with more efficient therapies [9].
The aims of the present study were to evaluate the effect of PNPLA3, TM6SF2, and GCKR genetic variants on a NAFLD case–control Greek cohort, to assess the impact of dietary habits and to further explore the interaction of these three single nucleotide polymorphisms (SNPs) with dietary factors and their effect on NAFLD.
Materials and methods
Study population
Study participants were consecutively recruited among volunteers visiting the Outpatient Clinics of the First Department of Propaedeutic Medicine, Laiko General Hospital, from June 2012 to February 2015. Adult subjects with (a) no self-declared concomitant liver injury at the time of recruitment (viral, autoimmune, genetic or drug-induced), and (b) no self-declared excessive alcohol intake were screened for the disease. Exclusion criteria included: age > 65 years, the presence of congenital or acquired liver disease, the presence of chronic viral hepatitis, the exposure to hepatotoxic drugs, daily consumption of ethanol more than 20 g for women and more than 30 g for men, the co-presence of a life-threatening disease or psychiatric disorders impairing the patient’s ability to provide written informed consent, pregnant or lactating women. After applying the exclusion criteria, a total of 351 individuals of Caucasian origin were recruited. All study subjects were informed about the aims of the study and signed a written consent. This study was approved by the Ethics Committee of Harokopio University of Athens (38074/13-07-2012), based on the Helsinki Declaration.
NAFLD diagnosis and classification
Participants were screened for NAFLD in the Radiology Department of the hospital. All volunteers underwent an abdominal ultrasound (U/S), performed by the same operator throughout the study period. Diagnosis of NAFLD was based on three parameters: (a) diffused echogenicity of the liver, (b) increased echogenicity compared to the renal cortex, (c) loss of definition of the diaphragm and blurring of the vascular margins [10]. Screened individuals were initially classified as follows: absence of hepatic steatosis (normal echogenicity), mild hepatic steatosis (mildly increased echogenicity, normal diaphragm and vascular margins definition), moderate hepatic steatosis (moderately increased echogenicity, mild loss of diaphragm and vascular margins definition) and severe hepatic steatosis (severely increased echogenicity and loss of diaphragm and vascular margins definition). Due to similar metabolic and clinical profiles, individuals with no and mild hepatic steatosis were further classified as controls, whereas individuals with moderate and severe hepatic steatosis were classified as cases.
Data collection
Demographics, medical history and family medical history
On the recruitment day, participants were interviewed regarding their age, origin, place of residence, education level, marital status, individual and family medical history. Medical history included information about medication and diseases, among others T2DM, hyperlipidemia, hypertension, hepatitis, Wilson disease, hypothyroidism, gastroesophageal reflux disease (GERD) and cardiovascular diseases (CVD).
Clinical and laboratory data
Blood pressure and heart rate were measured using an electronic blood pressure monitor. Three measurements were taken and the recorded value constituted the average of the last two.
Blood samples were collected after a 12-h overnight fast. Blood analysis included lipid profile, liver enzymes, fasting glucose, fasting insulin, glycated haemoglobin (HbA1c), uric acid, alkaline phosphatase (ALP) and albumin (Alb). Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald equation and the degree of insulin resistance was determined by the homeostatic model assessment (HOMA-IR) [11, 12]. Blood was centrifuged and plasma and serum were extracted and stored at − 80 °C for future analysis. Serum leptin levels were determined by an immunometric sandwich enzyme-linked immunosorbent assay (DuoSet ELISA, R&D Systems). Plasma and serum samples were extracted and stored at − 80 °C for future analysis.
Diagnosis of hyperlipidemia, T2DM, impaired fasting glucose (IFG), hypertension, hypothyroidism, CVD, sleep apnea and GERD were based on a combination of the self-declared information derived from the medical history questionnaire, the medication history and the blood tests results. MetS diagnosis was based on the following criteria: waist circumference [102 cm (men) or 88 cm (women)]; fasting blood glucose > 100 mg/dl or previously diagnosed type 2 diabetes; triglycerides > 150 mg/dl or current treatment for this abnormality; blood pressure > 130/85 mmHg or treatment for previously diagnosed hypertension; HDL cholesterol < 40 mg/dl (men) or < 50 mg/dl (women) or specific treatment for this abnormality [13]. Patients meeting three of these criteria were considered to have MetS.
Two predictive scores were calculated to assess the disease progression in our sample. NASH score has been validated to predict non-alcoholic steatohepatitis (NASH) [14]. NASH score calculation included PNPLA3 genotype at rs738409, AST levels and fasting insulin levels [− 3.05 + 0.562 × PNPLA3 genotype (CC = 1/CG = 2/GG = 3) − 0.0092 × fasting insulin (mU/L) + 0.0023 × AST (U/L) + 0.0019 × (fasting insulin × AST)]. NFS (NAFLD Fibrosis Score) constitutes a scoring system validated to separate NAFLD patients with and without advanced fibrosis. It was calculated based on a formula constructed by Angulo et al. [− 1.675 + 0.037 × age (years) + 0.094 × BMI (kg/m2) + 1.13 × IFG/diabetes (yes = 1, no = 0) + 0.99 × AST/ALT ratio − 0.013 × platelet (× 109/l) − 0.66 × albumin (g/dl)] [15].
Anthropometrics
All participants underwent anthropometric measurements. Body weight and body composition were assessed with an electronic scale (TANITA Segmental Body Composition Analyzer BC-418). This instrument estimates the percentage of fat mass, fat-free mass, total body water and bone mass using bioelectrical impedance analysis (BIA). BMI was calculated as weight (in kg) divided by height (in m) squared. Waist and hip circumferences were measured by well-trained dietitians using a stretch-resistant measuring tape. Waist measurements were taken at the point midway between the lower costal margin and the iliac crest and were recorded to the nearest 0.5 cm. Hip measurements were taken at the widest portion of the buttocks, with the tape parallel to the floor. All measurements were repeated twice and the average measurement was recorded.
Lifestyle and dietary habits
Subjects were interviewed about their smoking habits. Questions included their current smoking status (current smoker/nonsmoker/ex-smoker), smoking/abstinence duration and average number of cigarettes smoked daily. Pack-years were calculated for each individual using the formula: number of pack-years = (number of cigarettes smoked per day/20) × number of years smoked. Physical activity information was collected applying the validated short self-reported questionnaire Athens Physical Activity Questionnaire (APAQ) [16]. The APAQ evaluates the physical activity of an individual during work, at home and at leisure time during the past week. Physical activity data were used to calculate physical activity level (PAL) and total energy expenditure for each participant.
Dietary habits were assessed by a semi-quantitative self-reported Food Frequency Questionnaire (FFQ), which provides information about the consumption of 172 food items during the past year [17]. This questionnaire is adapted to the dietary habits of the Greek population; therefore, it reflects more accurately the actual dietary intake of our sample. Nutritionist Pro version 2·2 software (Axxya Systems-Nutritionist Pro, Stafford, TX, USA) was used to analyse nutritional information. All self-reported information was double-checked by well-trained dietitians in order to eliminate under- and over-reporting of dietary intake. Dietary information was summarized into food groups (Supplementary Table I).
DNA extraction and genotyping
DNA was extracted from the peripheral blood lymphocytes of each subject. Individuals were genotyped with a genome-wide SNP assay (Infinium CoreExome-24 BeadChip, Illumina). PNPLA3 rs738409 (C → G) (RefSeq NM_025225.2), TM6SF2 rs58542926 (G → A) (RefSeq NM_001001524.2) and GCKR rs780094 (G → A) (RefSeq NM_001486) genetic information for each individual was extracted from the database. A genetic risk score (GRS) was calculated based on the three loci, to investigate their combined effect on the condition. The GRS sums up the number of risk alleles carried by each individual.
Statistical analysis
Nominal and ordinal variables are given as frequencies (%), while continuous parametric traits as mean values ± SD. Normality of variables was tested using Kolmogorov–Smirnov test. To compare mean differences between the groups, Chi-square test (categorical variables), independent sample t test (parametric continuous variables) and Mann–Whitney test (non parametric continuous variables) were performed. Binary multiple logistic regressions were performed to test the hypothesis of association between various risk factors with the presence of NAFLD. Gene–diet interactions were also tested, assuming an additive model for PNPLA3 and GCKR and a dominant model for TM6SF2. All tests were two-sided and the cut-off level of significance was defined at 0.05. Significance of genetics results was assessed with a Bonferroni correction (p value ≤ 0.017). Statistical analyses were performed using IBM SPSS Statistics v21.0 and Plink v1.07.
Results
The sample consisted of 134 patients with NAFLD and 217 controls (Table 1). Mean age of cases was higher than that of controls (p < 0.001). NAFLD patients were less educated, less active and reported a higher rate of smoking compared to controls (p < 0.05). However, there was no difference regarding annual income, marital status and total sleeping hours. All anthropometric measurements, namely BMI, waist circumference, waist-to-hip ratio, % fat mass and fat free mass (kg), were higher in cases compared to controls (p < 0.001).
The clinical characteristics of the study population are summarized in Table 2. NAFLD patients had a bigger liver size compared to controls (p < 0.001). Systolic and diastolic blood pressure, white blood cells, iron and ferritin levels, as well as C-reactive protein levels were statistically significantly increased compared to controls. Furthermore, all glycemic and lipidemic traits, liver enzymes and biochemical indices were higher in the patients group (p < 0.05). Moreover, leptin levels were lower in the controls compared to the case group. No difference was found regarding platelets and albumin levels. NASH score and NFS were higher in NAFLD patients compared to controls (p < 0.001). Prevalence of most NAFLD-related metabolic diseases was significantly higher in cases than in controls. Specifically, hyperlipidemia was present in 70.9% of the NAFLD group, whereas only 38.2% of controls suffered from hyperlipidemia. Similarly, diabetes mellitus type 2, impaired fasting glucose, hypertension, metabolic syndrome, sleep apnea and gastroesophageal reflux disease were more prevalent in cases than in controls (p < 0.05). However, the prevalence of cardiovascular disease and hypothyroidism was not different between the groups.
PNPLA3 rs738409, TM6SF2 rs58542926 and GCKR rs780094 were genotyped for the whole sample. Genetic frequencies of the polymorphisms are in Hardy–Weinberg equilibrium. Information about the variants is demonstrated in Table 3. Effect allele frequencies in the study sample are 28.95% for the rs738409, 5.56% for the rs58542926 and 57.33% for the rs780094. Figure 1 summarizes the differences of prevalence of the risk alleles between the two groups. Carriers of risk alleles were equally distributed between the groups. Nevertheless, GRS was not equally distributed. There were more NAFLD patients than controls with a GRS = 4 and less cases with a GRS = 1. However, GRS = 0 is more prevalent in the cases group. The latter could be explained by the increased frequency of the rs780094 risk allele (EAF 57.33%).
Energy intake of NAFLD patients and controls was not different (p < 0.05) (Table 4). Moreover, most food groups were equally consumed. However, cases reported a higher intake of refined starchy foods than controls (2.52 ± 2.09 vs 2.08 ± 1.95, p = 0.046), as well as a lower consumption of fresh fruit juice (0.15 ± 0.26 vs 0.22 ± 0.29, p = 0.003).
Age, male gender, BMI, waist circumference, WHR and body composition were positively associated with NAFLD risk (p < 0.001). Regarding blood tests, most indices were positively associated with the condition, apart from HDL levels and AST/ALT ratio, which were negatively associated, after adjusting for the main confounding factors. The association of HDL with NAFLD was lost after further adjustment for pack-years and PAL. Moreover, the presence of the metabolic syndrome and its coexistent diseases statistically significantly increased the risk for NAFLD.
Among the three studied SNPs, only PNPLA3 rs738409 reached the Bonferroni-corrected level of association. Carrying one copy of the G allele was found to increase the risk of NAFLD by 78% compared to non-carriers (p = 0.013). After correcting the model for number of pack-years and PAL, the association remained statistically significant (p = 0.015). On the other hand, TM6SF2 and GCKR variants were not associated with the disease risk (OR 1.521, 95% CI 0.621–3.725, p = 0.359 and OR 0.82, 95% CI 0.521–1.292, p = 0.393, respectively) (Supplementary Table II).
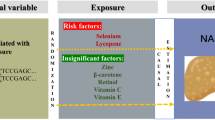
Adjustment for the aforementioned factors, uncovered more associations of food groups with the condition. Refined starchy foods, full fat cheese, fast food, sweet spreads and sugar, sauces and fried food were positively associated with NAFLD risk, whereas fish, fatty fish and nuts were reversely associated with the possibility of developing the condition (p < 0.05).
Table 5 summarizes the main contributors to NAFLD, which were revealed after adjusting for the main confounding factors (age, gender, BMI/energy intake) and other lifestyle factors (physical activity, smoking).
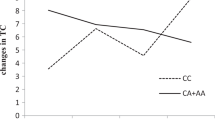
Moreover, some gene–diet interactions were detected. It was demonstrated that an increase of fish intake by one portion/week, increases the risk of developing NAFLD by 51.3% in those who carry at least one copy of the risk allele of TM6SF2 variant, compared to non-carriers (p = 0.012), taking into account age, gender, energy intake, PAL, pack-years, fish intake and TM6SF2 genotype (Fig. 2). Similarly, fatty fish was found to interact with TM6SF2 variant but this association was only nominally significant and did not reach the corrected level of statistical significance (OR 1.693, 95% CI 1.006–2.847, p = 0.047) (Fig. 3).
Interaction of fish consumption with TM6SF2 rs58542926 and NAFLD risk. Box plot describes fish consumption of NAFLD cases and controls, according to their TM6SF2 genotype (dominant model). NAFLD patients who are carriers of A allele of rs58542926 consume more fish than non-carriers (p value = 0.001). On the other hand, mean fish intake is not different between NAFLD controls (p value = 0.807). Interaction analysis showed that an increase of fish intake by 1 portion/week increases by 50.3% the risk of NAFLD for carriers of the risk allele compared to non-carriers (p value for interaction = 0.012). p value t test p value, p value interaction logistic regression p value
Interaction of fatty fish consumption with TM6SF2 rs58542926 and NAFLD risk. Box plot describes fatty fish consumption of NAFLD cases and controls, according to their TM6SF2 genotype (dominant model). NAFLD patients who are carriers of A allele of rs58542926 consume more fatty fish than non-carriers (p value = 0.001). On the other hand, mean fatty fish intake is not different between NAFLD controls (p value = 0.726). Interaction analysis showed that an increase of fatty fish intake by 1 portion/week increases by 69.3% the risk of NAFLD for carriers of the risk allele compared to non-carriers (p value for interaction = 0.047). However, the latter was only nominally significant. p value t test p value, p value interaction logistic regression p value
Discussion
Our study evaluated the effect of various clinical and lifestyle factors on NAFLD in a sample of Greek population. Moreover, we assessed the effect of selected loci on the disease, as well as their interaction with dietary habits in NAFLD.
We successfully replicated some previously reported risk factors for the disease, including age, BMI, body composition, glycemic and lipidemic profile, as well as the presence of other metabolic disturbances. Male gender was positively associated with NAFLD in our study, which is in accordance with most studies indicating males and post-menopausal women to be at high risk of developing the disease [18]. Furthermore, predictive scores indicated that our sample mainly consists of simple steatosis patients and not NASH patients, since mean values of NASH score and NFS did not exceed the estimated cut-off points (− 1.054 and − 1.455, respectively).
Regarding dietary habits, energy intake was not different between the two groups, despite the significant difference in BMI and clinical profile. Moreover, fish, fatty fish and nuts intakes were associated with decreased odds of developing NAFLD, whereas refined starchy foods, fast food, sweet spreads and sugar, sauces and fried food were found to increase the odds of NAFLD. The protective effect of fish and especially fish oil on NAFLD has been previously described by several studies [19, 20]. Fish and fatty fish, due to their exclusively high content of the omega-3 fatty acids, exert their beneficial effect on NAFLD by improving the lipidemic and glycemic control, as well as by attenuating inflammation. Nuts constitute a rich source of antioxidants, especially monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids (PUFAs), but also vitamin E, polyphenols and phytosterols. Both fish and nuts show a therapeutic potential in NAFLD [21]. On the other hand, foods rich in simple sugars, such as refined starchy foods, sweet spreads and sugar, and foods high in fat and saturated fat, such as fast food, sauces, fried food and full-fat cheese, aggravate the metabolic profile of NAFLD patients and increase hepatic steatosis. It seems that the type of fat and carbohydrates is more important that their actual amount.
Regarding the genetic background of the disease, we replicated the harmful effect of the PNPLA3 G allele on NAFLD. However, we failed to show an association of the GCKR and TM6SF2 risk alleles with the disease. Interestingly enough, the glucose-lowering allele of the GCKR rs780094 (A) was more prevalent in our sample (EAF 57.3%) compared to the European population (EAF 39.4%) (HapMap—CEU) [22]. In 2014, Petta et al. reported an increased risk allele frequency for rs780094 in an Italian population [23]. We could hypothesize that there are genetic mixtures in the Mediterranean populations, probably with Asian populations in which the reported rs780094 EAF was similar to the one reported herein [22].
We failed to demonstrate any additive effect of these three SNPs on disease development, after adjusting for the main confounding factors. However, a combined effect of rs738409 G and rs58542926 A alleles was found for individuals who carried 2 or 3 risk alleles, compared to non-carriers (OR 3.051, 95% CI 1.252–7.436, p = 0.014) (data now shown). This finding is in accordance with the results of Wang et al., who reported an additive effect of PNPLA3 and TM6SF2 on NAFLD Chinese patients [24]. Furthermore, a study by Krawczyk et al. showed higher ALT and AST levels in carriers of the two variants [25].
Our study also reported some gene–diet interactions in NAFLD. Increase of fish and fatty fish intake by rs58542926 A allele carriers further increased the odds of NAFLD (p = 0.012 and p = 0.047, respectively). This finding further supports the hypothesis that the TM6SF2 protein constitutes a novel key regulator of postprandial lipaemia. Recently, Luukkonen et al. demonstrated both in vitro and in vivo that rs58542926 A allele carriers experience impaired PUFAs integration into TG compared to non-carriers [26]. This resulted in higher intrahepatic TG and cholesteryl ester (CE) content, but lower phosphatidylcholine (PC) and serum TG levels. Furthermore, O’Hare et al. studied the effect of TM6SF2 deficiency in cultured human hepatocytes and in a zebrafish model [27]. Following dietary lipids stimulation, both systems developed impaired lipid homeostasis in the small intestine and in the liver. Deficiency of TM6SF2 resulted in increased lipid accumulation and decreased lipid export. The exact role of the encoded protein in lipid metabolism remains unclear. However, Ruhanen et al. have suggested that TM6SF2 affects the hepatocellular membrane lipid synthesis and dynamics [28]. Taking this into account, it seems that in response to high PUFAs intake, carriers of the TM6SF2 variant experience increased intrahepatic accumulation of TG and, therefore, hepatic steatosis. PUFAs supplementation in TM6SF2 variant carriers and non-carriers would shed light on this gene–diet interaction. So far, there is only one randomized clinical trial (RCT) which involves DHA (docosahexaenoic acid) + EPA (eicosapentaenoic acid) supplementation of NAFLD patients and the effect of TM6SF2 genotype [29]. The authors found no effect of the genotype on the results of the intervention. More RCTs are needed to clarify this potential interaction.
Some limitations of our study should be considered in interpreting the results. First of all, the diagnosis of NAFLD was based on U/S. U/S has 60–94% sensitivity and 84–95% specificity for detecting liver steatosis. Furthermore, results are highly dependent on the operator. The size of our sample is modestly small, which limits the possibility to detect genetic associations and gene–diet interactions. Last but not least, misclassification and recall bias of lifestyle and dietary information may still exist, despite all actions taken to eliminate this possibility.
Conclusion
This is the first study to report an interaction of TM6SF2 with food intake and its effect on NAFLD risk. Our results indicate an increased risk of developing the disease for GA and AA vs GG individuals when fish intake is increased by one portion per week. Even though replication by larger studies and RCTs is needed, the results of this case–control study show that PUFAs intake is not beneficial regardless of the genetic background. Unravelling gene–diet interactions in NAFLD would shed light on the personalized nutritional therapy of each individual.
Abbreviations
- Alb:
-
Albumin
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- APAQ:
-
Athens physical activity questionnaire
- AST:
-
Aspartate transaminase
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- Fe:
-
Iron
- Fer:
-
Ferritin
- FGlu:
-
Fasting glucose
- FIns:
-
Fasting insulin
- GERD:
-
Gastroesophageal reflux disease
- GRS:
-
Genetic risk score
- HbA1c:
-
Glycated haemoglobin
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostatic model assessment
- IFG:
-
Impaired fasting glucose
- LDL:
-
Low-density lipoprotein
- MetS:
-
Metabolic syndrome
- MUFAs:
-
Monounsaturated fatty acids
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- NFS:
-
NAFLD fibrosis score
- PLT:
-
Platelets
- PUFAs:
-
Polyunsaturated fatty acids
- SBP:
-
Systolic blood pressure
- SNPs:
-
Single nucleotide polymorphisms
- T2DM:
-
Type 2 diabetes mellitus
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- WBC:
-
White blood cells
- γ-GT:
-
Gamma-glutamyltransferase
References
Loomba R, Sanyal AJ (2013) The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol 10:686–690
Buzzetti E, Pinzani M, Tsochatzis EA (2016) The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 65:1038–1048
Anstee QM, Day CP (2013) The genetics of NAFLD. Nat Rev Gastroenterol Hepatol 10:645–655
Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, Boerwinkle E, Cohen JC, Hobbs HH (2008) Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 40:1461–1465
Kozlitina J, Smagris E, Stender S, Nordestgaard BG, Zhou HH, Tybjaerg-Hansen A, Vogt TF, Hobbs HH, Cohen JC (2014) Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 46:352–356
Mahdessian H, Taxiarchis A, Popov S, Silveira A, Franco-Cereceda A, Hamsten A, Eriksson P, van’t Hooft F (2014) TM6SF2 is a regulator of liver fat metabolism influencing triglyceride secretion and hepatic lipid droplet content. Proc Natl Acad Sci USA 111:8913–8918
Tan HL, Zain SM, Mohamed R, Rampal S, Chin KF, Basu RC, Cheah PL, Mahadeva S, Mohamed Z (2014) Association of glucokinase regulatory gene polymorphisms with risk and severity of non-alcoholic fatty liver disease: an interaction study with adiponutrin gene. J Gastroenterol 49:1056–1064
AISF (Italian Association for the Study of the Liver) (2017) AISF position paper on nonalcoholic fatty liver disease (NAFLD): updates and future directions. Dig Liver Dis, 49, 471–483
Ravi Kanth VV, Sasikala M, Sharma M, Rao PN, Reddy DN (2016) Genetics of non-alcoholic fatty liver disease: From susceptibility and nutrient interactions to management. World J Hepatol 8:827–837
Singh D, Das CJ, Baruah MP (2013) Imaging of non alcoholic fatty liver disease: a road less travelled. Indian J Endocrinol Metab 17:990–995
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Hyysalo J, Männistö VT, Zhou Y, Arola J, Karja V, Leivonen M, Juuti A, Jaser N, Lallukka S, Kakela P et al (2014) A population-based study on the prevalence of NASH using scores validated against liver histology. J Hepatol 60:839–846
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP et al. (2007) The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45:846–854
Kavouras SA, Maraki MI, Kollia M, Gioxari A, Jansena LT, Sidossis LS (2016) Development, reliability and validity of a physical activity questionnaire for estimating energy expenditure in Greek adults. Sci Sports 31:e47–e53
Dimitriou M, Rallidis LS, Theodoraki EV, Kalafati IP, Kolovou G, Dedoussis GV (2016) Exclusive olive oil consumption has a protective effect on coronary artery disease; overview of the THISEAS study. Public Health Nutr 19:1081–1087
Pan JJ, Fallon MB (2014) Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol 6:274–283
Mouzaki M, Allard JP (2012) The role of nutrients in the development, progression, and treatment of nonalcoholic fatty liver disease. J Clin Gastroenterol 46:457–467
Parker HM, Johnson NA, Burdon CA, Cohn JS, O’Connor HT, George J (2012) Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol, 56, 944–951
Gupta V, Mah XJ, Garcia MC, Antonypillai C, van der Poorten D (2015) Oily fish, coffee and walnuts: Dietary treatment for nonalcoholic fatty liver disease. World J Gastroenterol 21:10621–10635
International HapMap Consortium (2003) The international HapMap project. Nature, 426, 789–796
Petta S, Miele L, Bugianesi E, Camma C, Rosso C, Boccia S, Cabibi D, Di Marco V, Grimaudo S, Grieco A et al (2014) Glucokinase regulatory protein gene polymorphism affects liver fibrosis in non-alcoholic fatty liver disease. PLoS One 9:e87523
Wang X, Liu Z, Wang K, Wang Z, Sun X, Zhong L, Deng G, Song G, Sun B, Peng Z et al (2016) Additive effects of the risk alleles of PNPLA3 and TM6SF2 on non-alcoholic fatty liver disease (NAFLD) in a Chinese population. Front Genet 7:140
Krawczyk M, Rau M, Schattenberg JM, Bantel H, Pathil A, Demir M, Kluwe J, Boettler T, Lammert F, Geier A; NAFLD Clinical Study Group (2017) Combined effects of the PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 variants on NAFLD severity: a multicenter biopsy-based study. J Lipid Res 58:247–255
Luukkonen PK, Zhou Y, Nidhina Haridas PA, Dwivedi OP, Hyötyläinen T, Ali A, Juuti A, Leivonen M, Tukiainen T, Ahonen L et al (2017) Impaired hepatic lipid synthesis from polyunsaturated fatty acids in TM6SF2 E167K variant carriers with NAFLD. J Hepatol 67:128–136
O’Hare EA, Yang R, Yerges-Armstrong LM, Sreenivasan U, McFarland R, Leitch CC, Wilson MH, Narina S, Gorden A, Ryan KA et al (2017) TM6SF2 rs58542926 impacts lipid processing in liver and small intestine. Hepatology 65:1526–1542
Ruhanen H, Nidhina Haridas PA, Eskelinen EL, Eriksson O, Olkkonen VM, Käkelä R (2017) Depletion of TM6SF2 disturbs membrane lipid composition and dynamics in HuH7 hepatoma cells. Biochim Biophys Acta 1862:676–685
Scorletti E, West AL, Bhatia L, Hoile SP, McCormick KG, Burdge GC, Lillycrop KA, Clough GF, Calder PC, Byrne CD (2015) Treating liver fat and serum triglyceride levels in NAFLD, effects of PNPLA3 and TM6SF2 genotypes: results from the WELCOME trial. J Hepatol 63:1476–1483
Acknowledgements
This study was funded by the project “Obesity and metabolic syndrome: dietary intervention with Greek raisins in NAFLD/NASH. Investigation of molecular mechanisms” reviewed and approved by the Greek Secretariat for Research and Technology (Cooperation 890/2009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest relevant to this article were reported.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kalafati, I.P., Dimitriou, M., Borsa, D. et al. Fish intake interacts with TM6SF2 gene variant to affect NAFLD risk: results of a case–control study. Eur J Nutr 58, 1463–1473 (2019). https://doi.org/10.1007/s00394-018-1675-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1675-4