Abstract
Purpose
To provide evidence of the relationship of Mediterranean diet (MD) on incidence/mortality for cardiovascular disease (CVD), coronary/ischemic heart disease (CHD)/acute myocardial infarction (AMI) and stroke (ischemic/hemorrhagic) by sex, geographic region, study design and type of MD score (MDS).
Methods
We performed a systematic review and meta-analysis of observational studies. Pooled relative risks (RRs) were calculated using random-effects models.
Results
We identified 29 articles. The RR for the highest versus the lowest category of the MDS was 0.81 (95% CI 0.74–0.88) for the 11 studies that considered unspecified CVD, consistent across all strata. The corresponding pooled RR for CHD/AMI risk was 0.70 (95% CI 0.62–0.80), based on 11 studies. The inverse relationship was consistent across strata of study design, end point (incidence and mortality), sex, geographic area, and the MDS used. The overall RR for the six studies that considered unspecified stroke was 0.73 (95% CI 0.59–0.91) for the highest versus the lowest category of the MDS. The corresponding values were 0.82 (95% CI 0.73–0.92) for ischemic (five studies) and 1.01 (95% CI 0.74–1.37) for hemorrhagic stroke (four studies).
Conclusions
Our findings indicate and further quantify that MD exerts a protective effect on the risk of CVD. This inverse association includes CHD and ischemic stroke, but apparently not hemorrhagic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Mediterranean diet (MD) is the traditional dietary style of several countries around the Mediterranean Sea. Although the MD varies from one country to another, its key traditional features are: high consumption of grains and cereals (traditionally mainly whole grains), legumes, fruits, nuts, vegetables, and fish; use of olive oil as the main fat, with the consequent high monounsaturated/saturated fat ratio; moderate consumption of milk and dairy products; a low-to-moderate wine consumption (mainly at meals); and low consumption of meat and meat products. An a priori score to estimate the adherence to MD has been developed by Trichopoulou et al. [1] (TS), and is now commonly used together with some variants developed to better estimate MD adherence in non-Mediterranean countries [2, 3].
The MD has been associated with several benefits [4] such as reduced total mortality [5] and reduced risk of several diseases, including selected cancers [5, 6], cognitive impairment [7, 8], and the metabolic syndrome and its components, such as obesity, hypertension, hyperglycemia and hyperlipidemia [9].
Many observational studies have examined the relationship between MD and cardiovascular disease (CVD) incidence and mortality [10,11,12]. Their risk estimates have been summarized in a few meta-analyses [5, 7, 8, 12,13,14], which overall showed an inverse relationship. However, most meta-analyses have methodological limitations [15], including the lack of a complete literature search, the inclusion of duplicate studies, the lack of sensitivity analyses, and the lack of stratification by geographic area where the study was conducted (Mediterranean/non-Mediterranean country). Other notable limitations of previous meta-analyses are the omission of case–control studies and a failure to analyze studies in terms of different types of CVD (particularly stroke subtypes). This systematic review and meta-analysis provides quantitative evidence of the relationship of MD on incidence/mortality for CVD, coronary/ischemic heart disease (CHD)/acute myocardial infarction (AMI) and stroke (ischemic/hemorrhagic), by sex, geographic region, study design and type of MD score (MDS).
Materials and methods
Search strategy
We conducted a systematic literature search in the Medline database of studies published up to August 2016. The following search string was used: “Cardiovascular Diseases [Mesh] AND Mediterranean AND diet” without restrictions on language or publication date. Two authors (VG and AT) independently assessed the retrieved articles for inclusion/exclusion criteria. They also checked the reference list of pertinent papers to identify further studies. Abstracts and unpublished studies were not included. No studies were excluded a priori for weakness of design or data quality.
Eligibility criteria
We used eligibility criteria based on the PICOS (participants/population, intervention/exposure(s), comparator(s)/control, outcome(s), and study design) approach as follows: (1) participants: free of previous cardiovascular events, living in either Mediterranean or non-Mediterranean areas; (2) exposure: adherence to MD, assessed by an a priori MDS (TS or other); (3) comparators: population with a lower MD adherence, adjusted relative risk (RR) estimates with their confidence intervals (CIs); (4) outcomes: CHD, AMI, stroke (ischemic, hemorrhagic, or unspecified), and unspecified CVD; and (5) study design: case–control or cohort study.
Data extraction
Data extraction was undertaken independently by two authors (VG and VR). Any disagreement was resolved by discussion. We extracted the following information: last name of the first author, year of publication, location, study design (case–control or cohort study), number of subjects (cases and controls/non-cases/cohort size), sex, period of enrolment and follow-up, age, outcome (CHD/AMI, stroke, CVD), mortality or incidence study, type of MDS (TS or other) and range of score, effect estimator used, i.e., odds ratio (OR), RR, hazard ratio (HR), risk estimate (both categorically and continuously), and covariates adjusted for.
Statistical analysis
To assess the relationship between adherence to MD and CVD, summary estimates of the RR were calculated using DerSimonian and Laird random-effects models, that consider both within- and between-study variability [16]. We combined the risk estimates (RR, HR or OR) for the highest compared with the lowest category of the MDS from each cohort or case–control study. Studies were grouped according to the different clinical outcomes (CHD/AMI, ischemic or hemorrhagic stroke, unspecified CVD). We pooled together studies reporting incidence or mortality estimates, since by fitting meta-regression models we found no heterogeneity across strata of incidence or mortality for all the outcomes. When a study reported both incidence and mortality estimates separately, the incidence estimate was considered [17,18,19]. When a study [18, 20, 21] reported various estimates for various outcomes, we pooled these estimates using Hamling’s method to manipulate non-independent risk ratio [22]. The RRs adjusted for the largest number of confounding factors were included in all the analyses. For a study [23] reporting third quintile as reference category, we computed the RR for the fifth versus the first quintile and, to obtain the 95% CI, we calculated the approximate covariance matrix using generalized least squares [24, 25]. We included risk estimates for men and women combined, and if a study reported separate risk estimates [26, 27], we pooled them using the fixed effect models. We present the main combined estimates using forest plots.
We assessed heterogeneity among studies using the χ2 test (defined as significant for a p value < 0.10) [28] and quantified the inconsistencies using the I2 statistic [29, 30]. Subgroup analyses were performed by study design (case–control or cohort studies), end point (i.e., mortality or incidence), sex, geographic area of the study population (Mediterranean or non-Mediterranean countries), and type of MDS (TS or others). The overall RR for an increment of 1 point in the MDS was computed only for studies using the TS, by pooling the corresponding study-specific RRs with random-effects models [16]. When studies reported RRs for an increment of 2 points, the increment for 1 point was obtained by dividing the natural logarithm estimate by 2. When the increment was not reported in the original study, we computed it for studies reporting three or more categories of MDS [26, 31] using the method proposed by Greenland and Longnecker [24, 25].
To investigate the influence of single studies on the overall results, we conducted a sensitivity analysis in which one study at a time was removed. Publication bias was assessed by Begg’s and Mazumdar’s and Egger’s tests [32, 33]. All the analyses were performed using the STATA statistical package (version 13; StataCorp, College Station, TX, USA).
Results
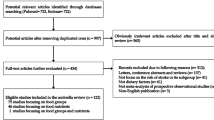
A total of 1264 publications was obtained up to August 2016 (Fig. 1). On the basis of the titles and abstracts we excluded 1041 of them. We retrieved the full text of 223 publications and then excluded 178 of them because they did not report data on the association between the adherence to the MD and the outcomes of interest. We identified two additional publications by scanning the reference lists of the retrieved publications [26, 34]. Of the remaining 47 publications, we further excluded 18 of them: 4 because of their cross-sectional design [35,36,37], 6 because they evaluated the relationship between adherence to the MD and secondary prevention of CVD [1, 38,39,40,41,42], 2 because they had been conducted on patients at high risk of CVD [43, 44], and 1 because it did not report the adjusted estimates [45]. When multiple reports were published on the same study population and they did not provide further information for stratified analyses [18, 23, 27, 46,47,48,49,50,51,52,53,54], we included only the most informative one [23, 27, 47, 48, 50, 52]; this resulted in the exclusion of five additional publications.
We identified 29 articles (based on 5 case–control and 21 cohort studies, as some studies considered various outcomes in different articles and some articles considered two cohorts), published from 1995 to 2016, that reported a quantitative relationship between MD adherence and CVD. The main characteristics and findings of these studies (from now we use the word study as a synonym of article) are reported in Table 1. The TS was used to assess the adherence to the MD in 12 studies, while 16 studies used alternative MDSs. The components included in the MDS in each study are listed in supplementary Table S1.
The pooled RR for CHD/AMI risk for the highest versus the lowest category of the MDS was 0.70 (95% CI 0.62–0.80), based on 11 studies (Fig. 2). The inverse relationship was consistent across strata of study design (RR 0.74 for cohort and 0.41 for case–control studies), end point (RR 0.62 for incident and 0.59 for fatal CHD/AMI), sex (RR 0.70 for women and 0.67 for men), geographic area (RR 0.61 for Mediterranean and 0.79 for non-Mediterranean countries), and the MDS used (RR 0.68 for TS and 0.72 for alternative scores) (Table 2).
The pooled RR for the six studies that considered unspecified stroke was 0.73 (95% CI 0.59–0.91) for the highest versus the lowest category of the MDS (Fig. 3), with a significant inverse relationship across strata of study design (RR 0.77 for cohort studies and 0.12 for the single case–control study, p for heterogeneity = 0.05), sex (RR 0.83 for women and 0.70 for men), and geographic area (RR 0.76 for Mediterranean and 0.66 for non-Mediterranean countries), and the MDS used (RR 0.74, 95% CI 0.62–0.89, for TS, and 0.36, 95% CI 0.05–2.41, for the two studies using alternative scores, p for heterogeneity = 0.85) (Table 2). The inverse association was significant for the two studies evaluating mortality (RR 0.73, 95% CI 0.53–0.99), but not for the two studies evaluating incidence (RR 0.37, 95% CI 0.05–2.62), in the absence of a significant heterogeneity across the strata (p for heterogeneity = 0.63). The relationship of the MD with ischemic and hemorrhagic stroke was considered in five and four studies, respectively, resulting in a pooled RR for the highest versus the lowest MDS of 0.82 (95% CI 0.73–0.92) for ischemic and 1.01 (95% CI 0.74–1.37) for hemorrhagic stroke (p for heterogeneity = 0.31, Fig. 3; Table 2).
The pooled RR for the highest versus the lowest category of the MDS was 0.81 (95% CI 0.74–0.88) based on the 11 studies that considered unspecified CVD (Fig. 4). The inverse relationship was consistent across strata of sex and MDS used. The inverse relationship was also consistent among strata of the other considered covariates with an overall RR of 0.61 (95% CI 0.44–0.86) for the two studies conducted in Mediterranean areas and 0.84 (95% CI 0.77–0.92) for the eight conducted in non-Mediterranean areas (p for heterogeneity = 0.11).
The Begg’s and Egger’s tests were, respectively, 0.087 and 0.034 for CHD/AMI, 0.13 and 0.008 for unspecified stroke, and 0.44 and 0.27 for unspecified CVD, showing a potential for publication bias for CHD/AMI and unspecified stroke.
In the sensitivity analysis, excluding one study at a time, the RRs for the highest versus the lowest category of MDS ranged from 0.68 (95% CI 0.60–0.77) to 0.72 (95% CI 0.64–0.82) for CHD/AMI, from 0.69 (95% CI 0.52–0.90) to 0.77 (95% CI 0.67–0.90) for unspecified stroke, and from 0.79 (95% CI 0.72–0.87) to 0.82 (95% CI 0.75–0.89) for unspecified CVD.
In the studies using the TS, we estimated the effect of an increment of one point of the MDS, which approximately corresponds to the addition of one favorable dietary habit. The RRs were 0.95 (95% CI 0.92–0.99) for CHD/AMI (six studies), 0.95 (95% CI 0.92–0.98) for unspecified stroke (five studies), and 0.97 (95% CI 0.96–0.99) for unspecified CVD (four studies).
Discussion
This meta-analysis, based on 29 publications (corresponding to 26 studies), shows a favorable role of the MD on CVD, with a decreased risk of about 20–25% for subjects with the highest adherence compared to those with the lowest one. The inverse relationship was consistent across strata of sex, study design, and type of the MDS used, and for different types of CVD (CHD/AMI, ischemic stroke), but no association was found with hemorrhagic stroke. The risk of CVD was 3% lower for an increment of one component of the MD when studies using the TS were pooled, indicating a dose–risk relationship. The existence of a real inverse association is further supported by the consistent results across studies, as the exclusion of any study from the analysis did not materially change the summary estimates.
Although based on a few studies, the finding of a lack of association for hemorrhagic stroke has no clear explanation. Both ischemic and hemorrhagic stroke have been associated with an unhealthy diet, but the relationship of cholesterol and lipoprotein profiles with ischemic and hemorrhagic stroke are different [70] and deserves further investigations.
We found stronger associations in case–control studies than in cohort ones, which reflects an exposure assessment closer to the disease onset in the former. However, the number of case–controls studies included is small. Although not significant, stronger associations were found for CHD/AMI in studies conducted in countries with a tradition of MD than in those without such tradition. This likely depends, at least in part, on the definition of the a priori MDS and of the prevalence of Mediterranean diet habits in various populations [1, 2, 67]. The cut points for components of the MD used for assessing a subject’s adherence to the MD are study specific, as they are defined on the basis of the distribution of consumption of each selected food in the population of controls and not in absolute terms (i.e., actual quantity of each food). Consequently, subjects with a higher MDS who live in Mediterranean countries generally have a higher absolute intake of Mediterranean food components than do populations living elsewhere.
The consistent relationship across sex and other subgroup analyses further support a real inverse association. Moreover, our findings are broadly consistent with those from other meta-analyses, including the two most recent ones [5, 13], but add information, mainly regarding the different effect of MD on ischemic and hemorrhagic stroke. There is only weak supporting evidence from randomized controlled trials, as none has compared CVD risk between subjects who follow a MD and those who do not. The PREDIMED trial studied the addition of either olive oil or nuts to the diet of a Spanish population, which presumably has a diet close to the MD, and demonstrated that CVD can be reduced by approximately 30% by an increased intake of either olive oil, especially extra-virgin olive oil, or nuts [71]. For unspecified stroke and unspecified CVD, only two studies were conducted in Mediterranean countries, thus the estimates are only indicative and the issue requires further investigation.
Our analyses have several strengths. First, compared with previous meta-analyses we included case–control studies and more cohort studies. Second, we stratified for many variables, including outcome (CHD/AMI or ischemic/hemorrhagic stroke), end point, sex, geographic region (Mediterranean/non-Mediterranean countries), study design and type of MDS. Third, we used a priori criteria for the inclusion of original studies. In addition, we excluded cross-sectional studies and randomized clinical trials [15]. Moreover, we have performed a meta-regression analysis to compare results taking incidence and mortality as end points, and when a paper reported both we have used only the wider category of incidence to avoid overlapping (inclusion of cases twice).
As for limitations, with reference to confounding, all original papers included in this meta-analysis, except one [67] were published after 2000, and the risk estimates had been adjusted for main confounding factors for CVD and diet. A limitation is the use of different definitions of MD in terms of different categorizations of the scores, inclusion of different foods and/or with different cut points. As an example, much research indicates that some foods that are highly consumed in the MD provide significant protection against CVD, whereas other components provide little or no protection. In particular, there is strong evidence that the following components of the MD provide significant protection against CVD: olive oil [72, 73], fruit, vegetables, legumes, nuts, and a higher consumption of fish compared with meat and meat products [74]. Alcoholic beverages, including wine, are also protective against CVD when consumed in moderation [75, 76]. A problematic component of the MD is a high consumption of grains and cereals, which are the main source of energy. However, while much evidence indicates that whole grains are protective against CVD, refined grains are not protective and may actually induce an increased risk [74]. Compounding this problem, some cohort studies have based their scoring system on the total intake of grains whereas others have only considered whole grains. Similarly, some studies included potatoes among vegetables while others did not.
Another limitation is that the asymmetry in the funnel plot and significant p values from Begg’s and Egger’s tests indicate that our results for CHD/AMI and strokes can be influenced by publication bias. However, when we stratified studies by the number of cases of CHD/AMI, we found a RR for the highest versus the lowest MDS of 0.71 (95% CI 0.64–0.79) and 0.60 (95% CI 0.48–0.76), respectively, for studies including more than 600 cases compared with smaller studies. Similarly, for unspecified stroke, the RRs were 0.82 (95% CI 0.72–0.94) and 0.52 (95% CI 0.26–1.03) for studies including more than 300 cases compared with smaller studies. This lack of material difference by study size further indicates that publication bias should not materially influence our findings. Moreover, the sensitivity analysis shows that the exclusion in turn of each paper did not materially change the pooled risk estimate, suggesting that no one paper is materially responsible for the inverse association.
The protective effect of the Mediterranean diet on vascular disease is plausible. In terms of nutrients, the MD is low in saturated fatty acids, rich in monounsaturated fatty acids, especially oleic acid, (mainly from olive oil), high in complex carbohydrates (from cereals and legumes) and high in fiber (from vegetables, fruit, cereals and legumes). Moreover, the high content of vegetables, fresh fruits, cereals and olive oil implies a high consumption of folate, flavonoids, polyphenols, vitamins C and E, and of various minerals, such as potassium and magnesium. These nutrients have favorable effects on cardiovascular health [74]. However, most of the beneficial effect is evident mostly when considering the whole MD rather than single components. This may depend on several factors, such as that the benefit of each component is too small to be detected, or that the effect of each component is synergistic with that of the others.
MD causes small favorable changes in most risk factors, including metabolic syndrome [9, 77,78,79], and its components, such as total blood cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglyceride, blood pressure [80], blood glucose [81], and waist circumference. Moreover, the MD has been related to many biochemical parameters related to CV health. Observational studies have shown that MD is related to lower endothelial dysfunction and favorable plasma concentrations of biomarkers [82], less carotid atherosclerosis [83], elevated non-enzymatic total antioxidant capacity and low oxidized LDL-cholesterol concentrations [84], lower insulin resistance [85], and selective measures of cardioprotective lipid profiles, glucose metabolism, and inflammation and coagulation levels [86].
In conclusion, compared with previously available analyses, our findings reinforce and more precisely quantify the protective association between consumption of the MD and the risk of CVD. Our findings add significant new information by demonstrating that this protective effect includes CHD and ischemic stroke but not hemorrhagic stroke.
Abbreviations
- MD:
-
Mediterranean diet
- CVD:
-
Cardiovascular disease
- CHD:
-
Coronary heart disease
- AMI:
-
Acute myocardial infarction
- MDS:
-
Mediterranean diet score
- RR:
-
Relative risk
- TS:
-
Trichopoulou score
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
References
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348(26):2599–2608. https://doi.org/10.1056/NEJMoa025039
Bach A, Serra-Majem L, Carrasco JL, Roman B, Ngo J, Bertomeu I, Obrador B (2006) The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: a review. Public Health Nutr 9(1A):132–146
Mila-Villarroel R, Bach-Faig A, Puig J, Puchal A, Farran A, Serra-Majem L, Carrasco JL (2011) Comparison and evaluation of the reliability of indexes of adherence to the Mediterranean diet. Public Health Nutr 14(12A):2338–2345. https://doi.org/10.1017/S1368980011002606
Dernini S, Berry EM, Serra-Majem L, La Vecchia C, Capone R, Medina FX, Aranceta-Bartrina J, Belahsen R, Burlingame B, Calabrese G, Corella D, Donini LM, Lairon D, Meybeck A, Pekcan AG, Piscopo S, Yngve A, Trichopoulou A (2016) Med Diet 4.0: the Mediterranean diet with four sustainable benefits. Public Health Nutr https://doi.org/10.1017/S1368980016003177
Sofi F, Macchi C, Abbate R, Gensini GF, Casini A (2014) Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17(12):2769–2782. https://doi.org/10.1017/s1368980013003169
Schwingshackl L, Hoffmann G (2014) Adherence to Mediterranean diet and risk of cancer: a systematic review and meta-analysis of observational studies. Int J Cancer 135(8):1884–1897. https://doi.org/10.1002/ijc.28824
Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N (2013) Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol 74(4):580–591. https://doi.org/10.1002/ana.23944
Sofi F, Macchi C, Abbate R, Gensini GF, Casini A (2010) Effectiveness of the Mediterranean diet: can it help delay or prevent Alzheimer’s disease? J Alzheimers Dis 20(3):795–801. https://doi.org/10.3233/JAD-2010-1418
Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB (2011) The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol 57(11):1299–1313. https://doi.org/10.1016/j.jacc.2010.09.073
D’Alessandro A, De Pergola G (2015) Mediterranean diet and cardiovascular disease: a critical evaluation of a priori dietary indexes. Nutrients 7(9):7863–7888. https://doi.org/10.3390/nu7095367
Liyanage T, Ninomiya T, Wang A, Neal B, Jun M, Wong MG, Jardine M, Hillis GS, Perkovic V (2016) Effects of the Mediterranean diet on cardiovascular outcomes-a systematic review and meta-analysis. PLoS One 11(8):e0159252. https://doi.org/10.1371/journal.pone.0159252
Mente A, de Koning L, Shannon HS, Anand SS (2009) A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 169(7):659–669. https://doi.org/10.1001/archinternmed.2009.38
Grosso G, Marventano S, Yang J, Micek A, Pajak A, Scalfi L, Galvano F, Kales SN (2015) A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: are individual components equal?. Crit Rev Food Sci Nutr. https://doi.org/10.1080/10408398.2015.1107021
Sofi F, Cesari F, Abbate R, Gensini GF, Casini A (2008) Adherence to Mediterranean diet and health status: meta-analysis. BMJ 337:a1344. https://doi.org/10.1136/bmj.a1344
Huedo-Medina TB, Garcia M, Bihuniak JD, Kenny A, Kerstetter J (2016) Methodologic quality of meta-analyses and systematic reviews on the Mediterranean diet and cardiovascular disease outcomes: a review. Am J Clin Nutr 103(3):841–850. https://doi.org/10.3945/ajcn.115.112771
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Dilis V, Katsoulis M, Lagiou P, Trichopoulos D, Naska A, Trichopoulou A (2012) Mediterranean diet and CHD: the Greek European prospective investigation into cancer and nutrition cohort. Br J Nutr 108(4):699–709. https://doi.org/10.1017/s0007114512001821
Hoevenaar-Blom MP, Nooyens AC, Kromhout D, Spijkerman AM, Beulens JW, van der Schouw YT, Bueno-de-Mesquita B, Verschuren WM (2012) Mediterranean style diet and 12-year incidence of cardiovascular diseases: the EPIC-NL cohort study. PLoS One 7(9):e45458. https://doi.org/10.1371/journal.pone.0045458
Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A (2012) Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol 176(12):1185–1192. https://doi.org/10.1093/aje/kws205
Tsivgoulis G, Psaltopoulou T, Wadley VG, Alexandrov AV, Howard G, Unverzagt FW, Moy C, Howard VJ, Kissela B, Judd SE (2015) Adherence to a Mediterranean diet and prediction of incident stroke. Stroke 46(3):780–785. https://doi.org/10.1161/strokeaha.114.007894
Tektonidis TG, Akesson A, Gigante B, Wolk A, Larsson SC (2015) A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: a population-based cohort study. Atherosclerosis 243(1):93–98. https://doi.org/10.1016/j.atherosclerosis.2015.08.039
Hamling J, Lee P, Weitkunat R, Ambuhl M (2008) Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med 27(7):954–970. https://doi.org/10.1002/sim.3013
Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB (2015) Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 132(23):2212–2219. https://doi.org/10.1161/circulationaha.115.017158
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309
Orsini NBR, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6(1):40–57
Chan R, Chan D, Woo J (2013) The association of a priori and a posterior dietary patterns with the risk of incident stroke in Chinese older people in Hong Kong. J Nutr Health Aging 17(10):866–874. https://doi.org/10.1007/s12603-013-0334-y
Reedy J, Krebs-Smith SM, Miller PE, Liese AD, Kahle LL, Park Y, Subar AF (2014) Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr 144(6):881–889. https://doi.org/10.3945/jn.113.189407
Greenland S (1987) Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 9:1–30
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Agnoli C, Krogh V, Grioni S, Sieri S, Palli D, Masala G, Sacerdote C, Vineis P, Tumino R, Frasca G, Pala V, Berrino F, Chiodini P, Mattiello A, Panico S (2011) A priori-defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J Nutr 141(8):1552–1558. https://doi.org/10.3945/jn.111.140061
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Thornton A, Lee P (2000) Publication bias in meta-analysis: its causes and consequences. J Clin Epidemiol 53(2):207–216
Yau WY, Hankey GJ (2011) Which dietary and lifestyle behaviours may be important in the aetiology (and prevention) of stroke? J Clin Neurosci 18(1):76–80. https://doi.org/10.1016/j.jocn.2010.05.014
Bilenko N, Fraser D, Vardi H, Shai I, Shahar DR (2005) Mediterranean diet and cardiovascular diseases in an Israeli population. Prev Med 40(3):299–305. https://doi.org/10.1016/j.ypmed.2004.06.004
Chrysohoou C, Panagiotakos DB, Aggelopoulos P, Kastorini CM, Kehagia I, Pitsavos C, Stefanadis C (2010) The Mediterranean diet contributes to the preservation of left ventricular systolic function and to the long-term favorable prognosis of patients who have had an acute coronary event. Am J Clin Nutr 92(1):47–54. https://doi.org/10.3945/ajcn.2009.28982
Hoscan Y, Yigit F, Muderrisoglu H (2015) Adherence to Mediterranean diet and its relation with cardiovascular diseases in Turkish population. Int J Clin Exp Med 8(2):2860–2866
de Lorgeril M, Salen P (2011) Mediterranean diet in secondary prevention of CHD. Public Health Nutr 14(12A):2333–2337. https://doi.org/10.1017/s136898001100259x
Lopez-Garcia E, Rodriguez-Artalejo F, Li TY, Fung TT, Li S, Willett WC, Rimm EB, Hu FB (2014) The Mediterranean-style dietary pattern and mortality among men and women with cardiovascular disease. Am J Clin Nutr 99(1):172–180. https://doi.org/10.3945/ajcn.113.068106
Trichopoulou A, Bamia C, Norat T, Overvad K, Schmidt EB, Tjonneland A, Halkjaer J, Clavel-Chapelon F, Vercambre MN, Boutron-Ruault MC, Linseisen J, Rohrmann S, Boeing H, Weikert C, Benetou V, Psaltopoulou T, Orfanos P, Boffetta P, Masala G, Pala V, Panico S, Tumino R, Sacerdote C, Bueno-de-Mesquita HB, Ocke MC, Peeters PH, Van der Schouw YT, Gonzalez C, Sanchez MJ, Chirlaque MD, Moreno C, Larranaga N, Van Guelpen B, Jansson JH, Bingham S, Khaw KT, Spencer EA, Key T, Riboli E, Trichopoulos D (2007) Modified Mediterranean diet and survival after myocardial infarction: the EPIC-Elderly study. Eur J Epidemiol 22(12):871–881. https://doi.org/10.1007/s10654-007-9190-6
Trichopoulou A, Bamia C, Trichopoulos D (2005) Mediterranean diet and survival among patients with coronary heart disease in Greece. Arch Intern Med 165(8):929–935. https://doi.org/10.1001/archinte.165.8.929
Panagiotakos DB, Arapi S, Pitsavos C, Antonoulas A, Mantas Y, Zombolos S, Stefanadis C (2006) The relationship between adherence to the Mediterranean diet and the severity and short-term prognosis of acute coronary syndromes (ACS): the Greek study of ACS (The GREECS). Nutrition 22(7–8):722–730. https://doi.org/10.1016/j.nut.2006.04.005
Pitsavos C, Panagiotakos DB, Chrysohoou C, Skoumas J, Papaioannou I, Stefanadis C, Toutouzas PK (2002) The effect of Mediterranean diet on the risk of the development of acute coronary syndromes in hypercholesterolemic people: a case–control study (CARDIO2000). Coron Artery Dis 13(5):295–300
Pitsavos C, Panagiotakos DB, Chrysohoou C, Papaioannou I, Papadimitriou L, Tousoulis D, Stefanadis C, Toutouzas P (2003) The adoption of Mediterranean diet attenuates the development of acute coronary syndromes in people with the metabolic syndrome. Nutr J 2:1
Konidari Z, Kastorini CM, Milionis HJ, Bika E, Nikolaou V, Vemmos KN, Goudevenos JA, Panagiotakos DB (2014) Eating behaviors and their relationship with cardiovascular disease. A case/case-control study. Appetite 80:89–95. https://doi.org/10.1016/j.appet.2014.05.005
Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB (2009) Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation 119(8):1093–1100. https://doi.org/10.1161/circulationaha.108.816736
Georgousopoulou EN, Kastorini CM, Milionis HJ, Ntziou E, Kostapanos MS, Nikolaou V, Vemmos KN, Goudevenos JA, Panagiotakos DB (2014) Association between mediterranean diet and non-fatal cardiovascular events, in the context of anxiety and depression disorders: a case/case-control study. Hellenic J Cardiol 55(1):24–31
Hoevenaar-Blom MP, Spijkerman AM, Boshuizen HC, Boer JM, Kromhout D, Verschuren WM (2014) Effect of using repeated measurements of a Mediterranean style diet on the strength of the association with cardiovascular disease during 12 years: the Doetinchem Cohort Study. Eur J Nutr 53(5):1209–1215. https://doi.org/10.1007/s00394-013-0621-8
Kastorini CM, Milionis HJ, Ioannidi A, Kalantzi K, Nikolaou V, Vemmos KN, Goudevenos JA, Panagiotakos DB (2011) Adherence to the Mediterranean diet in relation to acute coronary syndrome or stroke nonfatal events: a comparative analysis of a case/case-control study. Am Heart J 162(4):717–724. https://doi.org/10.1016/j.ahj.2011.07.012
Martinez-Gonzalez MA, Fernandez-Jarne E, Serrano-Martinez M, Marti A, Martinez JA, Martin-Moreno JM (2002) Mediterranean diet and reduction in the risk of a first acute myocardial infarction: an operational healthy dietary score. Eur J Nutr 41(4):153–160. https://doi.org/10.1007/s00394-002-0370-6
Martinez-Gonzalez MA, Fernandez-Jarne E, Serrano-Martinez M, Wright M, Gomez-Gracia E (2004) Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur J Clin Nutr 58(11):1550–1552. https://doi.org/10.1038/sj.ejcn.1602004
Martinez-Gonzalez MA, Garcia-Lopez M, Bes-Rastrollo M, Toledo E, Martinez-Lapiscina EH, Delgado-Rodriguez M, Vazquez Z, Benito S, Beunza JJ (2011) Mediterranean diet and the incidence of cardiovascular disease: a Spanish cohort. Nutr Metab Cardiovasc Dis 21(4):237–244. https://doi.org/10.1016/j.numecd.2009.10.005
Martinez-Gonzalez MA, Guillen-Grima F, De Irala J, Ruiz-Canela M, Bes-Rastrollo M, Beunza JJ, Lopez del Burgo C, Toledo E, Carlos S, Sanchez-Villegas A (2012) The Mediterranean diet is associated with a reduction in premature mortality among middle-aged adults. J Nutr 142(9):1672–1678. https://doi.org/10.3945/jn.112.162891
Mitrou PN, Kipnis V, Thiebaut AC, Reedy J, Subar AF, Wirfalt E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A (2007) Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med 167(22):2461–2468. https://doi.org/10.1001/archinte.167.22.2461
Bellavia A, Tektonidis TG, Orsini N, Wolk A, Larsson SC (2016) Quantifying the benefits of Mediterranean diet in terms of survival. Eur J Epidemiol 31(5):527–530. https://doi.org/10.1007/s10654-016-0127-9
Bertoia ML, Triche EW, Michaud DS, Baylin A, Hogan JW, Neuhouser ML, Tinker LF, Van Horn L, Waring ME, Li W, Shikany JM, Eaton CB (2014) Mediterranean and dietary approaches to stop hypertension dietary patterns and risk of sudden cardiac death in postmenopausal women. Am J Clin Nutr 99(2):344–351. https://doi.org/10.3945/ajcn.112.056135
Buckland G, Gonzalez CA, Agudo A, Vilardell M, Berenguer A, Amiano P, Ardanaz E, Arriola L, Barricarte A, Basterretxea M, Chirlaque MD, Cirera L, Dorronsoro M, Egues N, Huerta JM, Larranaga N, Marin P, Martinez C, Molina E, Navarro C, Quiros JR, Rodriguez L, Sanchez MJ, Tormo MJ, Moreno-Iribas C (2009) Adherence to the Mediterranean diet and risk of coronary heart disease in the Spanish EPIC Cohort Study. Am J Epidemiol 170(12):1518–1529. doi:https://doi.org/10.1093/aje/kwp282
Buckland G, Agudo A, Travier N, Huerta JM, Cirera L, Tormo MJ, Navarro C, Chirlaque MD, Moreno-Iribas C, Ardanaz E, Barricarte A, Etxeberria J, Marin P, Quiros JR, Redondo ML, Larranaga N, Amiano P, Dorronsoro M, Arriola L, Basterretxea M, Sanchez MJ, Molina E, Gonzalez CA (2011) Adherence to the Mediterranean diet reduces mortality in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Br J Nutr 106(10):1581–1591. https://doi.org/10.1017/S0007114511002078
Gardener H, Wright CB, Gu Y, Demmer RT, Boden-Albala B, Elkind MS, Sacco RL, Scarmeas N (2011) Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: the Northern Manhattan Study. Am J Clin Nutr 94(6):1458–1464. https://doi.org/10.3945/ajcn.111.012799
George SM, Ballard-Barbash R, Manson JE, Reedy J, Shikany JM, Subar AF, Tinker LF, Vitolins M, Neuhouser ML (2014) Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol 180(6):616–625. https://doi.org/10.1093/aje/kwu173
Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA (2004) Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA 292(12):1433–1439. https://doi.org/10.1001/jama.292.12.1433
Panagiotakos DB, Georgousopoulou EN, Pitsavos C, Chrysohoou C, Skoumas I, Pitaraki E, Georgiopoulos GA, Ntertimani M, Christou A, Stefanadis C (2015) Exploring the path of Mediterranean diet on 10-year incidence of cardiovascular disease: the ATTICA study (2002–2012). Nutr Metab Cardiovasc Dis 25(3):327–335. https://doi.org/10.1016/j.numecd.2014.09.006
Sjogren P, Becker W, Warensjo E, Olsson E, Byberg L, Gustafsson IB, Karlstrom B, Cederholm T (2010) Mediterranean and carbohydrate-restricted diets and mortality among elderly men: a cohort study in Sweden. Am J Clin Nutr 92(4):967–974. https://doi.org/10.3945/ajcn.2010.29345
Tognon G, Nilsson LM, Lissner L, Johansson I, Hallmans G, Lindahl B, Winkvist A (2012) The Mediterranean diet score and mortality are inversely associated in adults living in the subarctic region. J Nutr 142(8):1547–1553. https://doi.org/10.3945/jn.112.160499
Tognon G, Lissner L, Saebye D, Walker KZ, Heitmann BL (2014) The Mediterranean diet in relation to mortality and CVD: a Danish cohort study. Br J Nutr 111(1):151–159. https://doi.org/10.1017/s0007114513001931
Tong TY, Wareham NJ, Khaw KT, Imamura F, Forouhi NG (2016) Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study. BMC Med 14(1):135. https://doi.org/10.1186/s12916-016-0677-4
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D (1995) Diet and overall survival in elderly people. BMJ 311(7018):1457–1460
Panagiotakos DB, Pitsavos C, Matalas AL, Chrysohoou C, Stefanadis C (2005) Geographical influences on the association between adherence to the Mediterranean diet and the prevalence of acute coronary syndromes, in Greece: the CARDIO2000 study. Int J Cardiol 100(1):135–142. https://doi.org/10.1016/j.ijcard.2004.12.004
Turati F, Pelucchi C, Galeone C, Praud D, Tavani A, La Vecchia C (2015) Mediterranean diet and non-fatal acute myocardial infarction: a case-control study from Italy. Public Health Nutr 18(4):713–720. https://doi.org/10.1017/s1368980014000858
O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, Rangarajan S, Islam S, Pais P, McQueen MJ, Mondo C, Damasceno A, Lopez-Jaramillo P, Hankey GJ, Dans AL, Yusoff K, Truelsen T, Diener HC, Sacco RL, Ryglewicz D, Czlonkowska A, Weimar C, Wang X, Yusuf S, investigators I (2010) Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376(9735):112–123. https://doi.org/10.1016/S0140-6736(10)60834-3
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pinto X, Basora J, Munoz MA, Sorli JV, Martinez JA, Martinez-Gonzalez MA, Investigators PS (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368(14):1279–1290. https://doi.org/10.1056/NEJMoa1200303
Buckland G, Gonzalez CA (2015) The role of olive oil in disease prevention: a focus on the recent epidemiological evidence from cohort studies and dietary intervention trials. Br J Nutr 113(Suppl 2):S94–S101. https://doi.org/10.1017/S0007114514003936
Martinez-Gonzalez MA, Salas-Salvado J, Estruch R, Corella D, Fito M, Ros E, Predimed I (2015) Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis 58(1):50–60. https://doi.org/10.1016/j.pcad.2015.04.003
Mozaffarian D (2016) Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133(2):187–225. https://doi.org/10.1161/CIRCULATIONAHA.115.018585
Klatsky AL (2015) Alcohol and cardiovascular diseases: where do we stand today? J Intern Med 278(3):238–250. https://doi.org/10.1111/joim.12390
Roerecke M, Rehm J (2014) Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med 12:182. https://doi.org/10.1186/s12916-014-0182-6
Garcia M, Bihuniak JD, Shook J, Kenny A, Kerstetter J, Huedo-Medina TB (2016) The effect of the traditional Mediterranean-style diet on metabolic risk factors: a meta-analysis. Nutrients 8(3):168. https://doi.org/10.3390/nu8030168
Kesse-Guyot E, Ahluwalia N, Lassale C, Hercberg S, Fezeu L, Lairon D (2013) Adherence to Mediterranean diet reduces the risk of metabolic syndrome: a 6-year prospective study. Nutr Metab Cardiovasc Dis 23(7):677–683. https://doi.org/10.1016/j.numecd.2012.02.005
Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nunez-Cordoba JM, Martinez-Gonzalez MA (2007) Mediterranean diet inversely associated with the incidence of metabolic syndrome: the SUN prospective cohort. Diabetes Care 30(11):2957–2959. https://doi.org/10.2337/dc07-1231
Kokkinos P, Panagiotakos DB, Polychronopoulos E (2005) Dietary influences on blood pressure: the effect of the Mediterranean diet on the prevalence of hypertension. J Clin Hypertens (Greenwich) 7(3):165–170 (quiz 171–162)
Hodge AM, English DR, Itsiopoulos C, O’Dea K, Giles GG (2011) Does a Mediterranean diet reduce the mortality risk associated with diabetes: evidence from the Melbourne collaborative cohort study. Nutr Metab Cardiovasc Dis 21(9):733–739. https://doi.org/10.1016/j.numecd.2010.10.014
Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N, Willett WC, Hu FB (2005) Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr 82(1):163–173
Gardener H, Wright CB, Cabral D, Scarmeas N, Gu Y, Cheung K, Elkind MS, Sacco RL, Rundek T (2014) Mediterranean diet and carotid atherosclerosis in the Northern Manhattan Study. Atherosclerosis 234(2):303–310. https://doi.org/10.1016/j.atherosclerosis.2014.03.011
Pitsavos C, Panagiotakos DB, Tzima N, Chrysohoou C, Economou M, Zampelas A, Stefanadis C (2005) Adherence to the Mediterranean diet is associated with total antioxidant capacity in healthy adults: the ATTICA study. Am J Clin Nutr 82(3):694–699
Buscemi S, Nicolucci A, Mattina A, Rosafio G, Massenti FM, Lucisano G, Galvano F, Amodio E, Pellegrini F, Barile AM, Maniaci V, Grosso G, Verga S, Sprini D, Rini GB (2013) Association of dietary patterns with insulin resistance and clinically silent carotid atherosclerosis in apparently healthy people. Eur J Clin Nutr 67(12):1284–1290. https://doi.org/10.1038/ejcn.2013.172
Carter SJ, Roberts MB, Salter J, Eaton CB (2010) Relationship between Mediterranean diet score and atherothrombotic risk: findings from the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Atherosclerosis 210(2):630–636. https://doi.org/10.1016/j.atherosclerosis.2009.12.035
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
For this systematic review and meta-analysis there were no funding sources.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rosato, V., Temple, N.J., La Vecchia, C. et al. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr 58, 173–191 (2019). https://doi.org/10.1007/s00394-017-1582-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1582-0