Abstract
Aim
Evidence of a possible connection between gut microbiota and several physiological processes linked to type 2 diabetes is increasing. However, the effect of multi-strain probiotics in people with type 2 diabetes remains unclear. This study investigated the effect of multi-strain microbial cell preparation—also refers to multi-strain probiotics—on glycemic control and other diabetes-related outcomes in people with type 2 diabetes.
Design
A randomized, double-blind, parallel-group, controlled clinical trial.
Setting
Diabetes clinic of a teaching hospital in Kuala Lumpur, Malaysia.
Participants
A total of 136 participants with type 2 diabetes, aged 30–70 years, were recruited and randomly assigned to receive either probiotics (n = 68) or placebo (n = 68) for 12 weeks.
Outcomes
Primary outcomes were glycemic control-related parameters, and secondary outcomes were anthropomorphic variables, lipid profile, blood pressure and high-sensitivity C-reactive protein. The Lactobacillus and Bifidobacterium quantities were measured before and after intervention as an indicator of successful passage of the supplement through gastrointestinal tract.
Statistical analysis
Intention-to-treat (ITT) analysis was performed on all participants, while per-protocol (PP) analysis was performed on those participants who had successfully completed the trial with good compliance rate.
Results
With respect to primary outcomes, glycated hemoglobin decreased by 0.14 % in the probiotics and increased by 0.02 % in the placebo group in PP analysis (p < 0.05, small effect size of 0.050), while these changes were not significant in ITT analysis. Fasting insulin increased by 1.8 µU/mL in placebo group and decreased by 2.9 µU/mL in probiotics group in PP analysis. These changes were significant between groups at both analyses (p < 0.05, medium effect size of 0.062 in PP analysis and small effect size of 0.033 in ITT analysis). Secondary outcomes did not change significantly. Probiotics successfully passed through the gastrointestinal tract.
Conclusion
Probiotics modestly improved HbA1c and fasting insulin in people with type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Asia, type 2 diabetes (T2D) occurrence has been on the rise since the past 15 years [1] with the rate of increase showing no sign of slowing [1]. On a more local front, the prevalence of T2D in Malaysian adults aged 30 years and above was 22.9 % in 2013 [2] with majority of them being poorly controlled [3]. Medical nutrition therapy is the cornerstone of diabetes management; however, nutritional status and dietary adherence seemed to be far from the target treatment goal [3].
Diet is considered a primary determinant of a gut microbiota [4]. This is important in the current context because there are emerging evidences that gut microbiota can possibly influence several physiological functions that are linked to T2D [5]. Studies have shown some differences in the gut microbiota composition between people with and without T2D [6]. People with T2D are at risk to be in a low-grade chronic inflammation state, a condition that can be caused and/or aggravated by a compromised gut barrier function usually due to unhealthy gut microflora [7]. Hence, these findings suggest the possibility that modulating gut microbiota by probiotics supplementation may lead to favorable outcomes in people with T2D.
Probiotics are microbial cell preparations (MCP) or components of microbes that confer a health benefit on the host when administered in adequate amounts [8]. The beneficial role of probiotics in improving glycemic control has been discussed in the literature [9], and few numbers of clinical trials investigated the effect of probiotics in people with T2D. In three of the Iranian studies [10–12], two studies [10, 11] found positive effects on glycemic-related parameters after probiotics supplementation. The major limitations of these studies, however, were small sample size and inconsistent results. Besides, they were conducted among Iranian only and their results may not be extrapolated to Malaysian population due to the genetic differences, food consumption pattern, as well as environmental and cultural differences.
Probiotics have also demonstrated beneficial effects in other diabetes-related conditions including body weight, inflammatory markers and blood pressure. Study has shown that diversity of gut microbiota composition was strongly associated with body weight and fat mass [13]. In contrast, the meta-analysis of randomized controlled trials did not unravel any significant effect of probiotics on weight loss [14]. However, the total number of the studies included in the meta-analysis, total sample size and quality of the studies warranted future investigation [14].
The positive effect of probiotics on inflammatory markers has been demonstrated in animal models of T2D [15, 16]. Nevertheless, similar observation in human trials is limited and inconclusive due to the very small sample size [10–12]. Although two clinical trials have demonstrated promising improvements in blood pressure after being supplemented with probiotics among hypertensive participants [17] as well as healthy individuals [18], there are limited data regarding the blood pressure-lowering effect of probiotics among type 2 diabetics. With respect to potential lipid-lowering effect of probiotics, a meta-analysis by Guo et al. [19] demonstrated a positive effect of probiotics on lipid profile. However, the included studies had small sample size (32–78 participants) and small duration of intervention (4–10 weeks). Overall, the beneficial effects of probiotics on other diabetes-related parameters are inconclusive and scarce especially in the context of T2D.
To address the research gap, this randomized clinical trial was performed to investigate the effect of multi-strain probiotics supplementation on glycemic control and other diabetes-related outcomes in people with T2D. This study tested the hypotheses that supplementation with multi-strain probiotics will improve glycemic control as a primary outcome and other clinically important diabetes-related measures which include inflammatory marker, blood pressure, lipid profile and anthropometry status as secondary outcomes.
Methodology
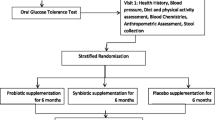
This 12-week randomized, double-blind, parallel-group, placebo-controlled trial was conducted at the diabetes clinic of a teaching hospital in Kuala Lumpur, Malaysia. The protocol was approved by the Clinical Research and Ethics Committee of the Universiti Kebangsaan Malaysia Medical Center, conformed to the contents of the 1975 Declaration of Helsinki as revised in 1983, and was registered at the US National Institutes of Health Web site (http://www.clinicaltrials.gov) #NCT01752803.
Participants selection
All the patients attended the diabetes clinic from February 2012 to December 2013 were screened for the study. Potential participants were approached by three trained research assistants at the hospital or by making phone calls to briefly explain the study. Then, the main researcher described the study (procedure, risks/benefits/voluntary participation, no compensation) to those willing to join while they were given adequate time to consult with their doctors and families. Those participants who agreed to join the study signed a consent form. Eligible participants include those with established T2D for at least 6 months prior to the commencement of the study, not on insulin and antibiotics, aged 30–70 years, had glycated hemoglobin A1c (HbA1c) between 6.5 and 12 %, had fasting blood glucose (FBG) <15 mmol/L, had BMI between 18.5 and 40 kg/m2, and on a stabilized dose of medication for at least 3 months before the study. The initial proposed range of age and HbA1c was extended due to the difficulties in fulfilling the sample size. The exclusion criteria were pregnancy, lactation, advanced diabetes complications (except for hyperlipidemia and blood pressure) and having other chronic illnesses. The sample size calculation was based on effect of probiotics among T2D [10] in which a 0.4 % difference in HbA1c and a common standard deviation of 0.7 % were required to detect a significant improvement in primary outcomes with 80 % power. Anticipating 40 % dropout, withdrawal and non-compliance, a total of 68 participants were needed in each group.
Intervention procedure
The random allocation sequence was generated by the main researcher with blocks of four and eight using a computer model (www.randomization.com). Using blocks of four and eight allowed having exact number of 68 participants in each group. The main researcher was in possession of allocation sequence and allocated the recruited participants accordingly. Sachets containing either probiotics—the term used throughout this study to refer to microbial cell preparations (MCP)—or a placebo were given to the participants according to their group assignment. Sachets were identical in terms of nutritional value, appearance, texture, weight and smell and were only differentiated by a code (“A” or “B”) placed on them. All the procedures were performed by the main researcher. The main researcher and participants remain blinded to the contents of the sachets throughout the study procedure and the statistical analysis. An independent person who was not related to the study and the study product held the blinding codes. Code breaking was performed after analysis was completed and database was locked.
All the participants have received standard medical nutrition therapy according to the guidelines for T2D [20] as a standard clinical procedure in this hospital. They were also again received the same recommendation at baseline aiming to homogenize their food intake regardless of the assigned group. Energy requirement was prescribed based on quick method formula as follows: Energy requirement = weight (kg) × quick method factor. Values of the quick method factor were determined based on the participant’s BMI and physical activity level [21]. The proportion of macronutrients was calculated accordingly with 45–60 % energy coming from carbohydrate, 15–20 % protein and 25–30 % fat [20]. The food exchange list was provided to all participants to allow a variety of food choices within each food group. Participants were asked to cease consumption of all foods and products known to contain probiotics bacteria 2 weeks before the study and throughout the study period. They were also informed not to change their routine intake of fiber content of their diet as an indication of prebiotic intake. The dietary advice was given by the main researcher.
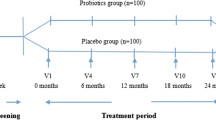
Participants were asked to fast for at least 10–12 h prior to each time point of assessment. A fasting blood sample was taken and processed for further analysis. The measurements were taken at baseline and week 12 with an interim analysis at week 6.
Participants were also asked to report any adverse effect through phone calls or during follow-up visits. Adverse effects were also assessed in follow-up visits through face-to-face interviews and recorded in the case report form. In the case of minor and tolerable adverse effects, participants were given the option either to continue or to stop taking the supplement. However, they were still asked to complete the follow-up visits even after they stopped taking the supplements. An expected common adverse effect includes minor gastrointestinal disturbances. Nevertheless, participants who experienced unexpected serious events were asked to stop taking the supplements and were encouraged completing the study.
Supplementation and compliance
Supplementation was provided by Hexbio® B-Crobes Laboratory Sdn. Bhd. (Ipoh, Malaysia). Each sachet provided a 3 × 1010 dose of six viable microbial cell preparation strains: three strains from the genus Lactobacillus, Firmicutes phyla (Lactobacillus acidophilus, Lactobacillus casei, Lactobacillus lactis) and three strains from the genus Bifidobacterium and Actinobacteria phyla (Bifidobacterium bifidum, Bifidobacterium longum and Bifidobacterium infantis). The daily dose of each strain was 1010 CFUs. Participants were asked to keep the sachets at a dry place below 25 °C and away from direct sunlight. They were also asked to mix the contents of the sachets with one glass of water (approximately 250 mL) and drink twice per day (morning and evening) before or after meal. Participants were asked to bring the remaining sachets to determine the compliance to supplementation with acceptable means of compliance between 85 and 100 % [22]. The acute toxicity test of supplement showed that this supplement was not considered as hazardous, and compatibility test of the products showed that all six strains are compatible with each other.
Outcome measurements
All the measurements were taken at baseline, week 6 and week 12. Primary outcome was glycemic control, and secondary outcomes include other diabetes-related variables including anthropometry and BMI, lipid profile, blood pressure and high-sensitivity C-reactive protein (hs-CRP). Fecal sample was analyzed in order to quantify the amount of Lactobacillus and Bifidobacterium subspecies plural (spp.) before and after the supplementation.
Body weight was measured using a digital scale (SECA; London British Indicators, London, UK) to the nearest 0.1 kg. Height was measured using the height attachment on the same scale to the nearest 0.1 cm. Body mass index (BMI) was calculated and categorized according to the World Health Organization classification [23]. Waist circumference was measured to the nearest 0.1 cm using a flexible tape. Blood pressure was measured with the use of an automatic blood pressure monitor (Omron M4-I; Omron Healthcare Europe BV, Hoofdorp, Netherlands) with participants resting in a sitting position for 5–10 min prior to measurement.
Blood samples were collected after 10–12 h overnight fasting. Blood was centrifuged for 15 min at 2555×g, and serum was stored frozen at −20 °C until they were analyzed except for FBG and HbA1c which were analyzed within 2 h after blood collection. FBG were measured using the enzymatic method and hs-CRP using particle-enhanced immunoturbidimetric assay. Triglycerides (TG) and total cholesterol (TC) were measured by specific enzymatic assay. The high-density lipoprotein (HDL) level was detected by homogeneous assay. The Cobas® 8000 modular analyzer, series 702 (Roche Diagnostics, Mannheim, Germany) was used for analysis of hs-CRP, FBG, TG, HDL and TC. HbA1c was measured by ion-exchange high-performance liquid chromatography using the Adams A1c HA-8160 automated HbA1c analyzer (Arkray, Inc., Kyoto, Japan) in the diabetes mode. Serum insulin was determined using solid-phase, two-site chemiluminescent enzyme-labeled immunometric assay using the Immulite (R) 2000 Analyser (Siemens, Gwynedd, UK). The homeostasis model assessment-estimated insulin resistance (HOMA-IR) was calculated using Matthews et al.’s equation [24]. The quantitative insulin sensitivity check index (QUICKI) was calculated using Katz et al.’s equation [25]. The levels of low-density lipoprotein (LDL) were calculated using the Friedewald et al.’s equation [26].
Dietary intake assessment was carried out using 3-day food records in which participants were asked to record their daily intake (2 weekdays and 1 weekend) before each visit to ensure that their food intakes were homogenous throughout the study period. The accuracy of the recorded foods including portion size, preparation, cooking method and food brand were checked and reviewed with the participants at each visit by main researcher. Nutrient analysis was performed using a computerized dietary analysis program (Nutritionist Pro, version 2.0; First Data Bank, Hearst Corp., NY, USA) by a trained dietitian. The results were presented as mean daily intakes of energy, macronutrients, fiber, sodium and cholesterol. Physical activity level was assessed by short form of the Malay version of the International Physical Activity Questionnaire (IPAQ), whose validity has been previously verified [27].
Fecal analysis
The quantities of Lactobacillus and Bifidobacterium spp. in fecal samples were measured at baseline and week 12 to demonstrate the successful passage of the supplements from gastrointestinal tract. In accordance with similar previous studies [6, 28], a subsample of participants (the last 20 participants from each group) was selected for determination of the number of colony-forming units (CFUs) of the Lactobacillus and Bifidobacterium spp. before and after the intervention using plate-counting method. Fecal samples were transformed to the laboratory in ice box within 3 h upon collection. De Man Rogosa and Sharpe agar (Difco, USA) supplemented with L-Cystein was opted as a selective media for culturing Bifidobacterium subspecies plural (spp.) [29]. Rogosa S/L agar was chosen as a selective media for Lactobacillus spp. [30]. Media were prepared according to the manufacturers’ instructions.
After performing serial dilution of fecal samples, 0.1 mL of dilutions of 10−3–10−6 were cultured under anaerobic conditions produced by gas pack (Oxoid Ltd, Basingstoke, UK) and placed in an incubator for 48 h. The number of colonies was then counted under a colony-counting machine (Stuart Scientific, Staffordshire, UK). Before colony counting, several colonies from each subject were selected for morphology and gram staining. The accuracy of the counted colonies was confirmed using polymerase chain reaction (PCR) (See supplementary materials).
Statistical analysis
Statistical analyses were performed using SPSS software version 22 (SPSS Inc., Chicago, USA). The significance level for the differences between and within groups was set at p < 0.05. Data were normally distributed unless otherwise stated. In this case, data were log-transformed to improve the skewness of the data into a normalized distribution. Baseline characteristics between the two groups were analyzed using independent sample t test or Chi-square test where necessary.
Sensitivity analyses included intention to treat (ITT) and per protocol (PP). ITT analysis was performed on a complete set of data with those missing data imputed according to the last observation carried forward (LOCF) method. On the other hand, PP analysis was performed on those participants who had successfully completed the 12-week intervention with more than 85 % compliance rate. In this article, the results presented are related to PP analysis unless otherwise stated, while the results of ITT analysis are reflected by the p values.
General linear model analysis of variance (GLM ANOVA) was performed separately for each group to obtain the results of within-group analysis. Changes between the groups as an indicator of interaction were analyzed using the same test considering grouping as the between-factor level. The partial eta-squared was calculated to determine the magnitude of change, with an effect size of 0.01–0.05 considered small, 0.06–0.13 medium and ≥0.14 large. Variables with significant changes were further analyzed using within-subject contrast test to determine at which time point the changes were significant. Subanalysis was also performed to determine the effect of probiotics in normal weight and overweight and obese (OW/OB) participants using the GLM ANOVA.
Results
Recruitment and subject flow
A total of 6976 patients were screened, of which 456 were identified eligible and have an updated contact in the hospital system. A total of 136 (29.8 %) patients were then agreed to participate. The attrition rate at the end of the 12-week intervention was 20.6 % without consideration of non-compliance and 25.7 % with their consideration. The compliance rate was comparable between groups (placebo = 89.05 %, probiotics = 86.15 %, p = 0.319). For the purpose of PP analyses, 48 participants in probiotics and 53 participants in placebo group completed the intervention successfully with compliance rate of >85 % (Fig. 1). None of the participants routinely consumed probiotics supplements or food sources that are rich in probiotics.
Demographic characteristics, compliance and adverse effects
A total of 136 participants (52.2 % male) were randomly allocated to the probiotics (n = 68) or placebo (n = 68) group. The two groups were comparable at baseline (Table 1). Majority of the participants were treated with oral anti-diabetic (OAD) agents. Only one (1.5 %) from the placebo and 6 (8.8 %) from Probiotic group were on diet alone. The proportion of participants on OAD was comparable between the groups (p = 0.144). The proportion of participants on lipid-lowering drugs and antihypertensive drugs were also comparable between groups. Majority of the participants were OW/OB [placebo 14 (21 %), probiotics 18 (26 %)], and the BMI of the participants was comparable between groups (p = 0.419).
The supplement was generally acceptable by the participants, and they were satisfied with the taste and smell of it. In terms of the adverse effects, few of them had minor gastric disturbances while two unexpected events were observed in the probiotic group that was unlikely due to the intervention (sexual impotency and carbuncle). The incidence of adverse effects was comparable between groups (p = 0.284).
Changes in dietary intake and physical activity levels
Dietary intake and physical activity levels did not change significantly between the groups over the course of the study (Table 2). Fiber intake as a source of prebiotic was also comparable between two groups throughout the study (6.9 ± 4.8 in probiotic group and 6.6 ± 3.8 in placebo group at baseline vs. 6.4 ± 4.4 in probiotic group and 7.0 ± 5.0 in placebo group at week 12, p = 0.874). As these variables were comparable between the groups at baseline and throughout the study period, they did not require adjustment in the analysis of the data.
Changes in primary outcomes
The HbA1c has marginally increased in placebo group, while it decreased 0.14 ± 0.41 % in probiotics group. These changes was significant between groups (p < 0.05, effect size 0.050; Table 3), but not significantly different within each group. According to within-subject contrast test, these changes were significant between baseline and week 6 and between baseline and week 12 (p < 0.05) (Fig. 2). ITT analysis revealed that HbA1c remained unchanged in the placebo group while marginally decreased in the probiotics group, although not to a statistically significant extent.
Fasting insulin decreased significantly between the groups (p < 0.05, effect size 0.062) (Table 3). Within-subject contrast test of PP analysis indicated that these changes were only significant between baseline and week 12 (p < 0.05) (Fig. 2). In ITT analysis, they were significant between baseline and both week 6 and week 12 (p < 0.05, effect size: 0.033). Other glycemic control parameters did not change significantly between groups throughout the study. It was also noted that the HOMA-IR value significantly increased by 23 % in the placebo group (0.4 ± 2.0, p < 0.05, paired t test between baseline values and week 12) and significantly decreased by 13 % in the probiotics group (0.4 ± 1.7, p < 0.05, paired t test between baseline values and week 12).
Changes in secondary outcomes
In both ITT and PP analyses, anthropometric parameters, BMI, hs-CRP, lipid profile and blood pressure did not change significantly between groups (Table 3). The TG levels improved in probiotics group as compared to placebo group, but not significant.
Changes in quantities of Lactobacillus and Bifidobacterium in fecal sample
For the fecal subsampling analyses, there were two participants from each group withdrew from the study. Hence, in total 18 participants in each group completed the fecal sampling procedures. While the colony-forming units (CFUs) of Bifidobacterium spp. increased marginally (almost twofold) in the placebo group, the CFUs have increased significantly (up to 4.5-fold) in the probiotic group (Table 3). The quantities of Lactobacillus spp. increased in both groups. The increment was not significant in placebo group, but the twofold increase in probiotics group was significant in PP analysis.
Changes in subgroups
In the subgroup PP analyses, participants were classified according to the BMI categories [normal weight (n = 28) and OW/OB (n = 73)]. Analysis of glycemic control parameters among normal weight and OW/OB revealed that normal weight participants had better improvements in terms of glycemic control parameters compared to OW/OB as indicated by the effect size (Table 4). However, this significant difference was only observed in HbA1c levels (Fig. 3). TG level was also improved significantly in normal weight participants in ITT analysis (marginally significant in PP analysis) while did not changed significantly among OW/OB participants (Fig. 4). Other diabetes-related parameters, however, did not show any trend of differences among normal weight or OW/OB participants between the two groups.
Discussion
This study found that probiotics supplementation significantly improved HbA1c in PP analysis and fasting insulin in both ITT and PP analyses in the probiotic group compared to those in the placebo group. In a subsequent analysis based on the BMI category, participants in the normal weight category from the probiotic group have significantly decreased HbA1c levels in both ITT and PP analyses and TG levels in ITT analysis. However, it does not significantly affect FBG, insulin resistance, insulin sensitivity, weight, waist circumference, BMI, hs-CRP, TC, HDL or LDL profile or blood pressure.
Effect of probiotic on glycemic control as a primary outcome measure
Improvements in glycemic control as seen in this study were in accordance with several studies reported previously [10, 12, 31, 32]. However, there were also 3 studies [11, 33, 34] that did not find any improvement in glycemic control after probiotics supplementation. Two of these studies were conducted among OW/OB participants [33, 34]. This could partly be explained by our observation among OW/OB participants that have less impact following probiotics supplementation [33, 34]. Lack of improvement in the study conducted by Mazlom et al. [11] could be due to the small sample size. The discrepancy of the results from different studies may also be partly attributed to the medications used by the participants. Different studies imposed different inclusion criteria with regard to the medications. Pharmacodynamics may have been affected by probiotics, especially gliclazide [35].
In this study, probiotics supplementation significantly improved HbA1c, while it has no effect on FBG. A notable fact is that in fairly controlled diabetes, FBG contributes approximately 30 % and postprandial blood glucose contributes approximately 70 % to HbA1c [36]. Thus, it can be assumed that improvements in postprandial blood glucose led to decreasing HbA1c in the probiotics group. Indeed, FBG is also influenced by several factors including physical activity [37], duration since the last meal [38] and a range of other neuroendocrine factors [39]. Hence, any change in the FBG levels due to intervention is difficult to be assessed.
Probiotics supplementation improved fasting insulin in this study which contradicts the results of the previous studies [10–12]. One of the possible reasons for this discrepancy could be the short duration of intervention in these studies which was 6 [10, 11] and 8 weeks [12] on the basis of PP analyses. We observed no significant changes within the first 6 week, yet the improvement in fasting insulin appeared significant after 12 week of intervention. Insulin resistance showed some improvements in this study, while insulin sensitivity did not change in this and previous studies [10–12].
Recent evidences showed that intestinal microbiota may play an important role in the early development of metabolic disease [40]. In this context, the effect of probiotics supplementation on HbA1c and fasting insulin was important as it triggered the underlying cause of impaired metabolism rather than treating the consequences.
Effect of probiotics on other diabetes-related parameters as secondary outcomes
We did not observe significant changes in body weight. In general, losing weight is more challenging in people with diabetes than healthy individuals, especially when the reduction was accompanied with the improvement in glycemic control [41]. In people with poorly controlled diabetes, the improvements in glycemic control will also lead to a reduction in energy expenditure, which prevents further weight loss [41].
The current study noted non-significant improvements in TG levels, while other lipid parameters did not show any improvements. Numerous studies have shown controversial results, of which some reported that probiotics supplementation significantly reduces blood lipids [42, 43], while other studies did not report any improvements after probiotics supplementation [44, 45]. A study showed that insulin acts as anti-lipolysis agent in adipose tissue and stimulates lipoprotein lipase [45]. Thus, with the abnormal level of insulin in people with type 2 diabetes, improving lipid profile after probiotics supplementation might be more difficult compared to people without diabetes. Suboptimal lipid profiles may attribute to the poor glycemic management of Malaysians with type 2 diabetes [46].
Not achieving the significant outcomes in lipid profiles and blood pressure may be caused by the type of the supplements. Studies have proven that the cholesterol-lowering effects of probiotics were only seen when they were combined with dairy products [47]. Similarly, in terms of blood pressure, the angiotensin-converting enzyme inhibitors exist in the form of proteins in some fermentable foods and can be converted into active form through fermentation process by probiotics bacteria [48]. Therefore, consuming probiotics in the current form without any substrate might explain the non-significant improvement in blood pressure in this study.
Overall, the impact of probiotics supplementation on hs-CRP remains controversial. This is in line with other human studies [11] which found no significant improvements in hs-CRP after probiotics supplementation. The levels of hs-CRP were in the normal range at baseline in both the groups. It is possible that probiotics were unable to modulate the hs-CRP because the levels were already substantially low. Another possible explanation is that majority of the participants were on statins. Studies have shown that statins affect hs-CRP levels [49, 50].
Effect of probiotics on the quantities of Lactobacillus and Bifidobacterium spp.
Probiotics supplementation significantly increased Lactobacillus and Bifidobacterium load in this study, thus proving successful passage of the supplement through the gastrointestinal tract. In the current study, the amount of Lactobacillus spp. and Bifidobacterium spp. increased in placebo group at week 12 though they were not statistically significant. Retrospective assessment of dietary intake to locate any increase in prebiotic and probiotics sources did not discover any foods that contributed to it.
Effect of probiotics in subgroup analyses among normal weight and OW/OB participants
After classification of BMI [51], we found probiotics supplementation has different outcomes in normal weight participants compared with OW/OB counterparts. While this subgroup was unplanned analysis in a small sample of size, the larger improvement observed in normal weight participants in terms of glycemic control and TG compared to OW/OB participants deserved further discussion. Even though it can be argued that we have more participants (n = 78) falling within OW/OB than the normal weight category (n = 28), the larger improvement documented within normal weight participants was unlikely related to sample size. The reason may be the fact that the Bacteroidetes-to-Firmicutes (B/F) ratio is lower in obese than in normal weight counterparts [52, 53], with Actinobacteria comprising a bigger proportion of the microbiota structure [52]. Since the quantity of Firmicutes is stable in both groups, the proportion is likely modulated by changes in Bacteroidetes [52]. The three phyla constitute more than 90 % of gut microbiota population [52, 53]. Considering the gut ecosystem as a competent ecosystem [50], supplementation with Lactobacillus and Bifidobacterium, which belong to the Firmicutes and Actinobacteria phyla, respectively [54], will change the ecology of gut microbiota. The B/F ratio, which has been found to be correlated with insulin resistance [55], appears to become much lowered in OW/OB compared with normal weight participants after supplementation with these phyla. The difference in this ratio between normal weight and OW/OB participants might explain differences in their response to probiotics. Indeed, there is a possibility that the dosage of probiotics may not be sufficient enough to allow any significant improvements in OW/OB participants, hence requiring the use of weight-based dosage regimens for significant changes.
Changes in TG levels after probiotics supplementation can be explained by the role of insulin in anti-lipolysis in adipose tissue and as a stimulant for lipoprotein lipase [56]. It can be hypothesized that a decrease in insulin levels in the current study leads to a reduction in the level or activity of lipoprotein lipase in adipose tissue. Therefore, less free fatty acids and TG are produced by the body. This hypothesis gains ground in the analysis of subgroups whereby the decrease in TG levels was more profound and significant among normal weight participants within probiotics group who had also better reduction in insulin levels compared with OW/OB participants in the same group.
This study was unable to explain the possible mechanism behind the effect of probiotics on glycemic and lipid control as presented in the result. We have hypothesized several mechanisms of action according to the previous literature. The effect of multi-strain probiotics in improving glycemic control can be firstly explained through the action of primary bile acids on the farnesoid X receptor (FXR). Certain strains of Lactobacillus and Bifidobacterium are known to possess the bile salt hydrolase enzyme (BSH). This enzyme can directly increase the levels of primary bile acid which in turn binds and activates the FXR, leading to increased storage of glucose, decreased production of glucose from non-glucose nutrients, increases synthesis of insulin and increases the secretion of insulin [57, 58]. Secondly, probiotics are also known to increase glucagon-like peptide (GLP) 1 and GLP 2 which are able to decrease low-grade inflammation associated with diabetes, decrease insulin resistance which in turn decreases ß-cell toxicity and improves glycemic control. Furthermore, GLP 1 and GLP 2 also decrease hunger and increase satiety, thus decreasing energy intake which collectively improved glycemic control [59]. Another possible mechanism is the increased production of short-chain fatty acids (SCFAs) by mainly Bifidobacterium in the colon via its action through insoluble dietary fibers. These SCFAs especially butyrate can decrease insulin resistance by promoting pancreatic ß-cells differentiation, proliferation and development, increase the secretion of GLP-1, thus increasing secretion of insulin, and decrease the release of proinflammatory cytokines by adipose tissue [60, 61]. A compromised gut barrier function can aggravate the pre-existing low-grade inflammatory state associated with T2D. Probiotics are known for their activity in restoring the gut barrier function. When the gut barrier function is not intact, there is an onset of metabolic endotoxemia. This condition increases the expression of selected proteins that suppresses the insulin signaling pathways. As a result, the body becomes less responsive to insulin and results in insulin resistance [7].
This study has several strengths that contributed to the reliability and validity of the findings. Possible confounding factors (dietary intake, particularly fiber intake and physical activity level) were well controlled. The participants were also asked to refrain from any prebiotics supplement or probiotics consumption 2 weeks before commencement of study and throughout the study. The significant increases in the quantities of Lactobacillus and Bifidobacterium species from stool samples enabled determination that the results could be attributed to probiotics supplementation.
The limitations of this study should be considered. Main researcher was in charge of randomization, while it would have had an added advantage if disclosing randomization sequence had been performed by a third person. Indeed, stool analysis was performed on a subsample of the last recruited participants which by right they should be randomly selected. Although this subsample was enough to draw a significant difference in the Lactobacillus and Bifidobacterium load before and after the intervention, the results would be more precise if a stool sample had been taken from all participants. Measuring the detailed microbial profile of the stool before and after intervention would have provided assurance in demonstrating that the observed improvements were probiotics mediated. Another area of concern is the length of the study. Diabetes-related complications usually occur over a long period of time and 12-week intervention might not be enough to reverse the condition.
Conclusion
Probiotics supplementation was associated with improvements in HbA1c and fasting insulin. Normal weight participants experience significant improvement in HbA1c and TG with probiotics supplementation compared to OW/OB participants. The multi-strain probiotics in the study also proved viable through gut transit. This study conducted among type 2 diabetics who were moderately well controlled, but caution should be taken for those who are uncontrolled and those on insulin, as current research only specially investigated in this group. Future research should focus on identifying the role of and the complex interaction among probiotics and the proportion of the various phyla in the gut in normal weight and OW/OB individuals. Besides, the effect of this multi-strain probiotics supplement should be investigated in large cohorts and the possible pathways involved in its beneficial glycemic- or lipid-lowering effects should be uncovered.
References
Guariguata L, Whiting DR, Hambleton I et al (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103:137–149. doi:10.1016/j.diabres.2013.11.002
Wan Nazaimoon WM, Md Isa SH, Wan Mohamad WB et al (2013) Prevalence of diabetes in Malaysia and usefulness of HbA1c as a diagnostic criterion. Diabet Med 30:825–828. doi:10.1111/dme.12161
Firouzi S, Barakatun-Nisak MY, Azmi KN (2015) Nutritional status, glycemic control and its associated risk factors among a sample of type 2 diabetic individuals, a pilot study. J Res Med Sci 20:40–46
Scott KP, Gratz SW, Sheridan PO, Flint HJ, Duncan SH (2013) The influence of diet on the gut microbiota. Pharmacol Res 69(1):52–60. doi:10.1016/j.phrs.2012.10.020
Musso G, Gambino R, Cassader M (2010) Obesity, diabetes, and gut microbiota. The hygiene hypothesis expanded? Diabetes Care 33:2277–2284
Larsen N, Vogensen FK, van den Berg FWJ et al (2010) Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS ONE 5:e9085
de Kort S, Keszthelyi D, Masclee AAM (2011) Leaky gut and diabetes mellitus: What is the link? Obes Rev 12:449–458. doi:10.1111/j.1467-789X.2010.00845.x
FAO/WHO (2002) WHO|guidelines for the evaluation of probiotics in food: joint FAO/WHO working group meeting, London Ontario, Canada, 30 April–1 May 2002. World Health Organization, London Ontario, Canada
Firouzi S, Barakatun-Nisak MY, Ismail A et al (2013) Role of probiotics in modulating glucose homeostasis: evidence from animal and human studies. Int J Food Sci Nutr 64:780–786. doi:10.3109/09637486.2013.775227
Ejtahed HS, Mohtadi Nia J, Homayouni Rad A et al (2011) The effects of probiotic and conventional yoghurt on diabetes markers and insulin resistance in type 2 diabetic patients: a randomized controlled clinical trial. Iran J Endocrinol Metab 13:1–8
Mazloom Z, Yousefinejad A, Dabbaghmanesh MH (2013) Effect of probiotics on lipid profile, glycemic control, insulin action, oxidative stress, and inflammatory markers in patients with type 2 diabetes: a clinical trial. Iran J Med Sci 38:38–43
Asemi Z, Zare Z, Shakeri H et al (2013) Effect of multispecies probiotic supplements on metabolic profiles, hs-CRP, and oxidative stress in patients with type 2 diabetes. Ann Nutr Metab 63:1–9
Le Chatelier E, Nielsen T, Qin J et al (2013) Richness of human gut microbiome correlates with metabolic markers. Nature 500:541–546. doi:10.1038/nature12506
Park S, Bae J-H (2015) Probiotics for weight loss: a systematic review and meta-analysis. Nutr Res 35:566–575. doi:10.1016/j.nutres.2015.05.008
Naito E, Yoshida Y, Makino K et al (2011) Beneficial effect of oral administration of Lactobacillus casei strain Shirota on insulin resistance in diet-induced obesity mice. J Appl Microbiol 110:650–657
Chen JJ, Wang R, Li X (2011) Bifidobacterium longum supplementation improved high-fat-fed-induced metabolic syndrome and promoted intestinal Reg I gene expression. Exp Biol Med 236:823–831
Jauhiainen T, Collin M, Narva M et al (2005) Effect of long-term intake of milk peptides and minerals on blood pressure and arterial function in spontaneously hypertensive rats. Milchwissenschaft-Milk Sci Int 60:358–362
Agerholm-Larsen L, Raben A, Haulrik N et al (2000) Effect of 8 week intake of probiotic milk products on risk factors for cardiovascular diseases. Eur J Clin Nutr 54:288–297
Guo Z, Liu XM, Zhang QX et al (2011) Influence of consumption of probiotics on the plasma lipid profile: a meta-analysis of randomised controlled trials. Nutr Metab Cardiovasc Dis 21:844–850
Malaysian Dietitians’ Association (2013) Clinical Practice Guideline, Medical nutrition therapy guideline for type 2 diabetes Mellitus. Ministry of Health, Kuala Lumpur, Malaysia
Cole HS, Camerini-Davalos RA (1970) Diet therapy of diabetes mellitus. Med Clin North Am 54:1577–1587
Krueger KP, Felkey BG, Berger BA (2003) Improving adherence and persistence: a review and assessment of interventions and description of steps toward a national adherence initiative. J Am Pharm Assoc 43:668–679
WHO expert consultation (2000) Obesity: preventing and managing the global epidemic Report of a WHO Consultation (WHO Technical Report Series 894). Geneva
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Katz A, Nambi SS, Mather K et al (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85:2402–2410
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Chu AHY, Moy FM (2012) Reliability and validity of the malay international physical activity questionnaire (IPAQ-M) among a malay population in Malaysia. Asia Pac J Public Health 27:NP2381–NP2389
De Vrese M, Winkler P, Rautenberg P et al (2005) Effect of Lactobacillus gasseri PA 16/8, Bifidobacterium longum SP 07/3, B. bifidum MF 20/5 on common cold episodes: a double blind, randomized, controlled trial. Clin Nutr 24:481–491. doi:10.1016/j.clnu.2005.02.006
Albertini B, Vitali B, Passerini N et al (2010) Development of microparticulate systems for intestinal delivery of Lactobacillus acidophilus and Bifidobacterium lactis. Eur J Pharm Sci 40:359–366. doi:10.1016/j.ejps.2010.04.011
Haarman M, Knol J (2006) Quantitative real-time PCR analysis of fecal Lactobacillus species in infants receiving a prebiotic infant formula. Appl Environ Microbiol 72:2359–2365. doi:10.1128/AEM.72.4.2359
Andreasen AS, Larsen N, Pedersen-Skovsgaard T et al (2010) Effects of Lactobacillus acidophilus NCFM on insulin sensitivity and the systemic inflammatory response in human subjects. Br J Nutr 104:1831–1838
Laitinen K, Poussa T, Isolauri E (2009) Probiotics and dietary counselling contribute to glucose regulation during and after pregnancy: a randomised controlled trial. Br J Nutr 101:1679–1687
Ivey KL, Hodgson JM, Kerr DA et al (2014) The effects of probiotic bacteria on glycaemic control in overweight men and women: a randomised controlled trial. Eur J Clin Nutr 68:447–452. doi:10.1038/ejcn.2013.294
Gobel RJ, Larsen N, Jakobsen M et al (2012) Probiotics to obese adolescents; RCT examining the effects on inflammation and metabolic syndrome. J Pediatr Gastroenterol Nutr 5:673–678
Al-Salami H, Butt G, Fawcett JP et al (2008) Probiotic treatment reduces blood glucose levels and increases systemic absorption of gliclazide in diabetic rats. Eur J Drug Metab Pharmacokinet 33:101–106
Zhou J, Martin RJ, Tulley RT et al (2008) Dietary resistant starch upregulates total GLP-1 and PYY in a sustained day-long manner through fermentation in rodents. Am J Physiol Metab 295:E1160–E1166
Jensen TE, Richter EA (2012) Regulation of glucose and glycogen metabolism during and after exercise. J Physiol 590:1069–1076. doi:10.1113/jphysiol.2011.224972
Munsters MJM, Saris WHM (2012) Effects of meal frequency on metabolic profiles and substrate partitioning in lean healthy males. PLoS ONE 7:e38632. doi:10.1371/journal.pone.0038632
Morton GJ, Schwartz MW (2011) Leptin and the central nervous system control of glucose metabolism. Physiol Rev 91:389–411. doi:10.1152/physrev.00007.2010
Burcelin R, Serino M, Chabo C et al (2011) Gut microbiota and diabetes: from pathogenesis to therapeutic perspective. Acta Diabetol 48(4):257–273
Pi-Sunyer FX (2005) Weight loss in type 2 diabetic patients. Diabetes Care 28:1526–1527
Pereira DIA, Gibson GR (2002) Effects of consumption of probiotics and prebiotics on serum lipid levels in humans. Crit Rev Biochem Mol Biol 37:259–281. doi:10.1080/10409230290771519
Ejtahed HS, Mohtadi Nia J, Homayouni Rad A et al (2011) Effect of probiotic yogurt containing Lactobacillus acidophilus and Bifidobacterium lactis on lipid profile in individuals with type 2 diabetes mellitus. J Dairy Sci 94:3288–3294
Sadrzadeh-Yeganeh H, Elmadfa I, Djazayery A et al (2010) The effects of probiotic and conventional yoghurt on lipid profile in women. Br J Nutr 103:1778–1783. doi:10.1017/S0007114509993801
Laakso M, Sarlund H, Salonen R et al (1991) Asymptomatic atherosclerosis and insulin resistance. Arterioscler Thromb Vasc Biol 11:1068–1076. doi:10.1161/01.ATV.11.4.1068
Chew BH, Ismail M, Lee PY et al (2012) Determinants of uncontrolled dyslipidaemia among adult type 2 diabetes in Malaysia: the Malaysian Diabetes Registry 2009. Diabetes Res Clin Pract 96:339–347. doi:10.1016/j.diabres.2012.01.017
Ooi LG, Liong MT (2010) Cholesterol-lowering effects of probiotics and prebiotics: a review of in vivo and in vitro findings. Int J Mol Sci 11:2499–2522. doi:10.3390/ijms11062499
Seppo L, Jauhiainen T, Poussa T, Korpela R (2003) A fermented milk high in bioactive peptides has a blood pressure–lowering effect in hypertensive subjects. Am J Clin Nutr 77:326
Ansell BJ, Watson KE, Weiss RE, Fonarow GC (2003) hsCRP and HDL effects of statins trial (CHEST): rapid effect of statin therapy on C-reactive protein and high-density lipoprotein levels A clinical investigation. Heart Dis 5:2–7. doi:10.1097/01.HDX.0000050407.62572.DE
Ridker PM, Danielson E, Fonseca FA et al (2009) Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet 373:1175–1182. doi:10.1016/S0140-6736(09)60447-5
WHO expert consultation (2004) BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
Turnbaugh PJ, Hamady M, Yatsunenko T et al (2009) A core gut microbiome in obese and lean twins. Nature 457:480–484. doi:10.1038/nature07540
Million M, Angelakis E, Maraninchi M et al (2013) Correlation between body mass index and gut concentrations of Lactobacillus reuteri, Bifidobacterium animalis, Methanobrevibacter smithii and Escherichia coli. Int J Obes 37:1460–1466. doi:10.1038/ijo.2013.20
Tremaroli V, Bäckhed F (2012) Functional interactions between the gut microbiota and host metabolism. Nature 489:242–249. doi:10.1038/nature11552
Caricilli AM, Picardi PK, de Abreu LL et al (2011) Gut microbiota is a key modulator of insulin resistance in TLR 2 knockout mice. PLoS Biol 9:e1001212. doi:10.1371/journal.pbio.1001212
Singh B, Saxena A (2010) Surrogate markers of insulin resistance: a review. World J Diabetes 1:36–47
Renga B, Mencarelli A, Vavassori P et al (2010) The bile acid sensor FXR regulates insulin transcription and secretion. Biochim Biophys Acta 1802:363–372. doi:10.1016/j.bbadis.2010.01.002
Ding L, Yang L, Wang Z, Huang W (2015) Bile acid nuclear receptor FXR and digestive system diseases. Acta Pharm Sin B 5:135–144. doi:10.1016/j.apsb.2015.01.004
Shyangdan DS, Royle P, Clar C et al (2011) Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev. doi:10.1002/14651858.CD006423.pub2
Tilg H, Moschen AR (2014) Microbiota and diabetes: an evolving relationship. Gut 63:1513–1521. doi:10.1136/gutjnl-2014-306928
Puddu A, Sanguineti R, Montecucco F, Viviani GL (2014) Evidence for the gut microbiota short-chain fatty acids as key pathophysiological molecules improving diabetes. Mediators Inflamm 2014:162021. doi:10.1155/2014/162021
Acknowledgments
We gratefully acknowledge the participants and project partners for their enthusiastic support of the study. We thank Universiti Putra Malaysia and B-Crobes Laboratory Sdn. Bhd. for funding this project.
Financial support
This study was funded by internal grant of Universiti Putra Malaysia and research grant of B-Crobes Laboratory Sdn. Bhd. The supplements were provided by “B-Crobes Laboratory Sdn. Bhd.”
Author’s contribution
The authors’ responsibilities were as follows: SF (PhD student) was involved in study conception, study coordination, study conduct, laboratory testing and analysis, statistical analysis and manuscript writing; HAM critically reviewed the manuscript; AI reviewed the manuscript; NAK was involved in administrative coordination; MY B-N served as principle investigator, was involved in study conception and study coordination and reviewed the manuscript. All authors were responsible for the study design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Ethical approval
The protocol was approved by the Clinical Research and Ethics Committee of the Universiti Kebangsaan Malaysia Medical Center, conformed to the contents of the 1975 Declaration of Helsinki as revised in 1983, and was registered at the US National Institutes of Health Web site (http://www.clinicaltrials.gov) #NCT01752803.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Firouzi, S., Majid, H.A., Ismail, A. et al. Effect of multi-strain probiotics (multi-strain microbial cell preparation) on glycemic control and other diabetes-related outcomes in people with type 2 diabetes: a randomized controlled trial. Eur J Nutr 56, 1535–1550 (2017). https://doi.org/10.1007/s00394-016-1199-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1199-8