Abstract
Background/aim
Obesity is characterized by a low-grade inflammation in white adipose tissue (WAT), which promotes insulin resistance. Low serum levels of 1α,25-dihydroxycholecalciferol (DHCC) associate with insulin resistance and higher body mass index although it is unclear whether vitamin D supplementation improves insulin sensitivity. We investigated the effects of DHCC on adipokine gene expression and secretion in adipocytes focusing on two key factors with pro-inflammatory [monocyte chemoattractant protein-1 (MCP-1/CCL2)] and anti-inflammatory [adiponectin (ADIPOQ)] effects.
Methods
Pre-adipocytes were isolated from human subcutaneous WAT and cultured until full differentiation. Differentiated adipocytes were either pre-treated with DHCC (10−7 M) and subsequently incubated with tumor necrosis factor-α (TNFα, 100 ng/mL) or concomitantly incubated with TNFα/DHCC. MCP1 and adiponectin mRNA expression was measured by RT–PCR and protein release by ELISA.
Results
DHCC was not toxic and did not affect adipocyte morphology or the mRNA levels of adipocyte-specific genes. TNFα induced a significant increase in CCL2 mRNA and protein secretion, while DHCC alone reduced CCL2 mRNA expression (~25%, p < 0.05). DHCC attenuated TNFα-induced CCL2 mRNA expression in both pre-incubation (~15%, p < 0.05) and concomitant (~60%, p < 0.01) treatments. TNFα reduced ADIPOQ mRNA (~80%) and secretion (~35%). DHCC alone decreased adiponectin secretion to a similar degree (~35%, p < 0.05). Concomitant treatment with DHCC/TNFα for 48 h had an additive effect, resulting in a pronounced reduction in adiponectin secretion (~70%).
Conclusions
DHCC attenuates MCP-1 and adiponectin production in human adipocytes, thereby reducing the expression of both pro- and anti-inflammatory factors. These effects may explain the difficulties so far in determining the role of DHCC in insulin sensitivity and obesity in humans.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insulin resistance in obesity is associated with a chronic low-grade inflammation in white adipose tissue (WAT). This is characterized by an increased infiltration of macrophages, which results in a disturbed production of cyto- and chemokines [1]. Among the pro-inflammatory regulators, TNFα is considered to be a key factor, which links increased fat mass with insulin resistance and inflammation [2]. In man, TNFα acts in an auto-/paracrine manner [3] and induces several effects including stimulation of lipolysis [4], apoptosis [5], and inhibition of adipocyte differentiation [6]. TNFα also regulates the production of both pro- and anti-inflammatory adipokines in human adipocytes [7].
The primary factors initiating macrophage recruitment into WAT have been elucidated in recent years. One of the most interesting candidates is the chemokine monocyte chemoattractant protein-1 (MCP-1) [8]. The expression of this factor is believed to be up-regulated in adipocytes early in the development of obesity, which results in an increased recruitment of macrophages [9, 10]. The infiltrating macrophages also produce MCP-1, thereby stimulating further macrophage migration. Among factors that could potentially attenuate this process is adiponectin, an insulin-sensitizing hormone produced by adipocytes [11], whose levels are dramatically decreased in obesity and insulin resistance [12, 13]. TNFα plays an integrative role in the regulation of the expression of these adipokines since it stimulates MCP-1 and inhibits adiponectin secretion/expression [14].
An interesting factor that could play a role in promoting an inflammatory response in human adipose tissue is hypoxia. It has been proposed that the growth in size and possibly number of adipocytes in obesity result in an increased distance to the microvasculature and a reduced oxygen tension in WAT. In cultures of human adipocytes, hypoxia stimulates the expression of several pro-inflammatory adipokines and inhibits the secretion of anti-inflammatory factors such as adiponectin (reviewed in [15]).
Vitamin D is either taken up by the diet or produced in the skin under UV radiation. The circulating form of vitamin D is 25-hydroxycholecalciferol, which is further converted to the biologically active form 1α,25-dihydroxycholecalciferol (DHCC). Emerging evidence in the last few years has suggested a link between vitamin D and insulin sensitivity, as low serum 25-hydroxycholecalciferol levels have been associated with insulin resistance [16] and higher body mass index [17]. It was recently proposed that DHCC plays an important role in the regulation of adipocyte metabolism and thereby in the control of energy homeostasis [18]. DHCC modulates human adipocyte metabolism via several mechanisms. These include post-transcriptional effects (i.e., stimulation of Ca2+ influx) that affect lipogenesis and lipolysis [19] but also direct transcriptional regulation. The latter is mediated by activation of the nuclear vitamin D receptor (VDR) [20]. Upon ligand binding, VDR forms heterodimers with the retinoid X receptor (RXR) and binds to genomic sites termed vitamin D response elements (VDREs) in the proximity of its target genes [21].
A number of studies have suggested a potential role for DHCC in adipose tissue inflammation. Microarray data from human adipocytes suggest that DHCC up-regulates genes involved in inflammation but also genes controlling cell proliferation, angiogenesis, and oxidative stress [22]. In another study, conducted in human adipocytes, DHCC was reported to stimulate the expression of inflammatory cytokines while inhibiting the production of anti-inflammatory cytokines [23, 24]. However, the role of DHCC as a pro-inflammatory compound is controversial since some studies have also described anti-inflammatory effects [23–25]. To our knowledge, there are no publically available data regarding the crosstalk between DHCC and TNFα in human adipocytes. In this study, we aimed to define possible reasons for the divergent findings regarding DHCC’s effects in adipose inflammation. We therefore investigated the effects of DHCC in the regulation of MCP-1 and adiponectin production both alone or in combination with TNFα in in vitro differentiated adipocytes obtained from human subcutaneous WAT.
Materials and methods
Patient samples
This study was conducted in accordance with the guidelines in the Declaration of Helsinki and approved by the ethics committee at Karolinska University Hospital. The study was explained in detail to each subject, and written informed consent was obtained. Subcutaneous WAT was obtained from healthy women undergoing elective surgical procedures of fat removal for esthetic purposes (age 39.5 ± 10.3 years; BMI 31.9 ± 8.5 kg/m2).
Cell culture
Cell culture experiments were performed on in vitro differentiated adipocytes isolated from subcutaneous WAT. Isolation, culture, and in vitro differentiation of human pre-adipocytes were performed as previously described [26]. Experiments were performed in 12-well plates after 10–12 days of differentiation. At the end of the differentiation, the adipocytes displayed similar functional and morphological characteristics as mature fat cells. Most importantly, we have previously shown that the expression of adipocyte-specific genes and proteins, lipolytic responses, and GPDH activity (a marker of adipocyte differentiation) at day 12 in culture was in the same range as in mature primary fat cells [27].
Treatments
After 10–12 days of differentiation, adipocytes were treated with or without DHCC (10−7 M; Sigma–Aldrich, St. Louis MO) and/or TNFα (100 ng/mL, Sigma–Aldrich) for 24 or 48 h. The concentration of DHCC was determined in separate titration experiments, and the lowest concentration giving significant effects without affecting morphology or expression of adipocyte-specific genes of the cells was used throughout the study (data not shown). In pre-incubation wells, adipocytes were initially pre-treated with DHCC for 24 h after which DHCC was removed by washing and adipocytes were further incubated with TNFα for an additional time period of 24 h. In concomitant wells, adipocytes were treated with DHCC and TNFα (both agents added at the same time) for a total time of 48 h including a medium change after 24 h. DHCC and TNFα were dissolved in ethanol and water, respectively, according to the instructions of the manufacturer. Control cells were treated with the same amount of corresponding vehicle.
Quantitative real-time PCR
Cells were treated as described earlier, and total RNA was extracted using the NucleoSpin RNA II (Macherey–Nagel, Düren, Germany). RNA concentration and purity were assessed spectrophotometrically with a NanoDrop ND-1000 (Thermo Scientific, Wilmington, DE). One microgram of total RNA was reverse-transcribed to cDNA using Omniscript reverse transcription kit (QIAGEN, Hilden, Germany) and random hexamer primers (Invitrogen, Carlsbad, CA). For SYBR Green assays (ADIPOQ coding for adiponectin; LIPE coding for hormone-sensitive lipase; PNPLA2 coding for adipose triglyceride lipase; PLIN1 coding for perilipin-1; PPARG coding for peroxisome proliferator-activated receptor gamma), 5 ng of cDNA was mixed with 2x iQ SYBR Green Supermix (Eurogentec SA, Ougre’e, Belgium) and primers (Invitrogen,) in a final volume of 25 μL as previously described [28–30]. For TaqMan assays, cDNA (10 ng) was mixed with 2x TaqMan Universal PCR Master Mix (Applied Biosystems, Foster City, CA) and TaqMan primers (CCL2 coding for MCP-1; SLC2A1 coding for glucose transporter 1, GLUT-1; Applied Biosystems) in a final volume of 20 μL [14, 30]. Quantitative real-time PCR was performed in an iCycler IQ (Bio-Rad Laboratories, Hercules, CA). mRNA levels were determined by a comparative threshold cycle (Ct) method. Ct values were normalized to the reference gene LDL receptor-related protein 10 (LRP10), according to the formula 2ΔCt target gene/2ΔCt reference gene = Arbitrary Units (AU). The PCR efficiency in all runs was close to 100%, and all samples were run in duplicate.
Adipokine measurements
Human MCP-1 and adiponectin protein levels were measured in medium aliquots using a Quantikine Immunoassay (R&D Systems, Minneapolis, MN), according to the manufacturer’s instructions.
Statistical analysis
Results are means ± SEM. Statistical analyses were performed by paired or unpaired Student’s t test (two tailed) unless otherwise stated. Similar statistically significant results were obtained when using non-parametric tests (data not shown). Differences were considered as statistically significant at p < 0.05. The statistical analyses were performed using Statview software (version 5.01; SAS Institute, Cary, NC).
Results
Effects of DHCC on morphology and expression of adipocyte-specific genes
In initial experiments, we determined the effects of different concentrations of DHCC on adipocyte morphology. Concentrations from 10−8 to 10−6 M did not affect adipocyte morphology in our cell culture model at any stage of differentiation (data not shown). These concentrations are considered to be within the physiological and pharmacological range of DHCC as reported elsewhere [31]. The effect of different concentrations of DHCC on the expression of genes characteristic of fat cells [hormone-sensitive lipase (LIPE), adipose triglyceride lipase (PNPLA2), perilipin (PLIN1), and peroxisome proliferator-activated receptor γ (PPARG)] was assessed in fully differentiated adipocytes treated for 24 or 48 h. Incubation with DHCC did not affect gene expression at either time point or concentration (data not shown). As expected, treatment with 100 ng/mL TNFα down-regulated the mRNA levels of LIPE, PNPLA2, PLIN1, and PPARG (by approximately 90%). However, the addition of DHCC either prior to or concomitant with TNFα treatment did not affect the mRNA levels of any of these genes at any concentration tested (for 10−7 M, Fig. 1a). This demonstrates that in differentiated human adipocytes, DHCC, in the range between 10−8 and 10−6 M, is not toxic and does not affect adipocyte morphology or the expression of genes typical for fat cells. For all subsequent experiments, results are presented for 10−7 M DHCC.
Effects of TNFα and 1α,25-dihydroxycholecalciferol (DHCC) on the mRNA expression of adipocyte-specific genes and the hypoxia-responsive gene SLC2A1. Human adipocytes were treated with 100 ng/mL TNFα for 48 h with or without 10−7 M DHCC (Ccmt DHCC + TNFα and TNFα, respectively). In addition, cells were preincubated with DHCC for 24 h followed by a 24-h incubation with TNFα (Preinc DHCC + TNFα). Messenger RNA levels of LIPE, PNPLA2, PLIN1, PPARG (a), and SLC2A1 (b) are displayed. *p < 0.05, ***p < 0.001 as compared to control adipocytes. Results are shown as a mean of up to six independent experiments. Data are expressed as mean ± SEM
Effects of DHCC on the mRNA levels of the hypoxia-responsive gene SLC2A1
Previous studies have demonstrated that hypoxia affects the expression and secretion of inflammation-related adipokines in human adipocytes [32]. To assess whether DHCC could affect the expression of hypoxia-responsive genes, we determined the mRNA expression levels of SLC2A1 (coding for the protein GLUT-1), a gene previously shown to be highly up-regulated under hypoxic conditions in human adipocytes [33]. The presence of DHCC alone, prior to or concomitantly with TNFα, did not alter SLC2A1 levels (Fig. 1b). In addition, although TNFα up-regulated (p < 0.05) SLC2A1 mRNA expression, this effect was not modified by DHCC. This suggests that the effects of DHCC on adipokine expression are not secondary to changes in hypoxia-related genes.
Effects of DHCC on MCP-1 production in human adipocytes
DHCC induced a ~30% decrease in CCL2 mRNA expression after both 24 h (p < 0.01) and 48 h (p < 0.05) of treatment compared to control adipocytes (Fig. 2a). As expected, TNFα induced a pronounced (30–40-fold) induction of CCL2 mRNA expression (Fig. 2b). Pre-incubation with DHCC for 24 h attenuated the increase in CCL2 mRNA induced by TNFα by ~15% (p < 0.05). This effect was even more marked following concomitant treatment with DHCC and TNFα for 48 h (~60%, p < 0.01). DHCC alone (Fig. 2c) or a 24-h incubation prior to TNFα treatment (Fig. 2d) did not modify MCP-1 protein secretion. However, there was a trend (p = 0.056, two-tailed; p = 0.028 one-tailed test) toward decreased TNFα-induced MCP-1 protein release in cells concomitantly incubated with DHCC and TNFα (Fig. 2d). In adipocytes incubated with 10−6 M DHCC, the attenuating effect on MCP-1 secretion was significant (p < 0.01, graph not shown). Thus, in our experimental settings, DHCC reduces CCL2 mRNA expression although the effects at the protein level are less pronounced.
Effects of 1α,25-dihydroxycholecalciferol (DHCC) and TNFα on CCL2 mRNA expression and MCP-1 secretion. Human adipocytes were incubated as described in Fig. 1 (b, d) or with DHCC alone for 24 h or 48 h (a, c). Concentrations of DHCC and TNFα were the same as in the experiments described in Fig. 1. The effects of DHCC on MCP-1 secretion were only statistically significant in cells treated concomitantly with TNFα and DHCC when using a one-sided t test (d). *p < 0.05, **p < 0.01 as compared to control or TNFα-treated adipocytes. *§ p < 0.05 compared to TNFα-stimulated adipocytes using one-tailed t test. Results are shown as a mean of up to six independent experiments. Data are expressed as mean ± SEM
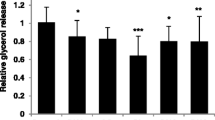
Effects of DHCC on adiponectin secretion in human adipocytes
Incubation with DHCC did not affect ADIPOQ mRNA expression (Fig. 3a). However, DHCC alone induced a ~35% decrease in adiponectin secretion after treatment for both 24 and 48 h (p < 0.05; Fig. 3c). TNFα markedly reduced ADIPOQ production at both the mRNA (~80%, p < 0.001 Fig. 3b) and protein level (~35–40%, p = 0.01, Fig. 3d). Concomitant treatment with DHCC and TNFα decreased adiponectin protein secretion in an additive manner (~75%, p < 0.01 Fig. 3d). In contrast, DHCC either prior to or concomitantly with TNFα did not significantly modify ADIPOQ mRNA levels (Fig. 3b). This suggests that DHCC mainly affects adiponectin secretion/release at the post-transcriptional level.
Effects of 1α,25-dihydroxycholecalciferol (DHCC) and TNFα on ADIPOQ expression and adiponectin secretion. Human adipocytes were incubated as described in Fig. 2. Effects on ADIPOQ mRNA levels (a, b) and adiponectin secretion (c, d) are displayed. *p < 0.05, **p < 0.01, ***p < 0.001 as compared to control or TNFα-treated adipocytes. Results are shown as a mean of up to six independent experiments. Data are expressed as mean ± SEM
Discussion
Several studies have demonstrated the ability of DHCC to modulate energy metabolism by regulating lipogenesis and lipolysis [19] as well as adipokine expression in human adipocytes [34]. However, its interaction with inflammatory factors has not been elucidated before in human fat cells. In this work, we demonstrate that DHCC has differential effects on TNFα regulation of MCP-1 and adiponectin, two important adipokines with opposite effects on insulin sensitivity and inflammation. DHCC reduces the mRNA levels of CCL2 and to a lesser extent also protein secretion. Therefore, DHCC might attenuate adipose tissue inflammation by reducing MCP-1. On the other hand, DHCC inhibited adiponectin secretion, an adipokine that improves insulin sensitivity and inflammation [35, 36]. These novel data suggest a dual role of vitamin D in the adipose inflammation.
DHCC appears to regulate the expression of these two factors via different mechanisms. Thus, adiponectin secretion seems to be controlled at the post-transcriptional level. It has previously been demonstrated that TNFα inhibits adiponectin production via down-regulation of pro-adipogenic factors, such as PPARγ [37]. However, it is not likely that DHCC attenuates adiponectin secretion via reduced adipocyte differentiation since DHCC did not affect the morphology or the expression of fat cell-specific genes. Therefore, the mechanism(s) through which DHCC affects adiponectin secretion remain to be defined.
In contrast to ADIPOQ, CCL2 is most probably a direct VDR target gene. The latter is supported by an in silico promoter analysis we have performed. We identified several VDREs in the human CCL2 gene promoter using the MatInspector software (www.genomatix.de/). Admittedly, there was only a trend regarding the effect of DHCC on MCP-1 secretion, but it is possible that longer incubation times would have resulted in more prominent changes. In any case, our results are in agreement with the previous studies, showing that DHCC down-regulates CCL2 expression in primary kidney cells [38] and renal epithelial cells [39]. In the latter study, the authors reported that DHCC suppressed TNFα-induced MCP-1 mRNA expression and suggested a possible role for DHCC as a modulator of renal inflammation, an effect proposed to be mediated via nuclear factor κB. However, our findings are in contrast to the results published by Sun and Zemel [40] who reported that 10−8 M DHCC up-regulated MCP-1 mRNA expression in differentiated 3T3-L1 adipocytes after 48 h of treatment. Differences in concentrations but more probably cell systems (murine 3T3-L1 adipocytes vs. human adipocytes) could explain these discrepancies.
We also show that DHCC did not affect the expression of the hypoxia-responsive gene SLC2A1, suggesting that the effects of DHCC on adipokine expression are not secondary to changes in hypoxia-responsive genes. This, however, does not preclude that DHCC could regulate hypoxia-sensitive genes in other cell types within adipose tissue, a question that will be addressed in future experiments.
The use of human adipocytes in this study constitutes an advantage when interpreting the results in a physiological context. We have recently shown that these cells express genes and phenotypical traits comparable to those of mature primary fat cells freshly isolated from adipose tissue [27]. In contrast, murine adipocytes and other available fat cell lines are qualitatively different in many important aspects [41].
The concentration of DHCC used in the present study might be a point for potential controversies, since Sun and Zemel reported a pro-apoptotic role for DHCC at high (pharmacological) concentrations of the hormone (≥ to 10−7 M) in human adipocytes in vitro [42]. However, under the conditions used in our experiments, we did not observe any toxic effects at concentrations up to 10−6 M and no effects on the mRNA expression of adipocyte-specific genes, such as LIPE, PNPLA2, PLIN1 and PPARG. This is in agreement with a study in porcine adipocytes [43], where 10−6 M DHCC had no effects on cell viability. In any case, it should be stressed that it is difficult to compare concentrations used in vitro with the levels of DHCC in plasma or adipose tissue in vivo.
The effect of vitamin D supplementation on insulin sensitivity in clinical trials is not clear (reviewed in [44]). While some authors have reported improvements in parameters of insulin secretion and/or resistance, others have not observed any changes. A caveat in most of these studies is that they were rather small and neither randomized nor placebo-controlled, which therefore warrants further research. This study sheds new light on the complex role of DHCC in human inflammation. It could be speculated that the dual effects of DHCC on adipokine secretion could to some extent explain the lack of clear effects on insulin sensitivity of vitamin D supplementation in humans. Clinical studies are underway in order to elucidate the role of DHCC in obesity and insulin resistance.
References
Hotamisligil GS, Shargill NS, Spiegelman BM (1993) Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259(5091):87–91
Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM (1995) Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest 95(5):2409–2415
Lofgren P, van Harmelen V, Reynisdottir S, Naslund E, Ryden M, Rossner S, Arner P (2000) Secretion of tumor necrosis factor-alpha shows a strong relationship to insulin-stimulated glucose transport in human adipose tissue. Diabetes 49(5):688–692
Ryden M, Dicker A, van Harmelen V, Hauner H, Brunnberg M, Perbeck L, Lonnqvist F, Arner P (2002) Mapping of early signaling events in tumor necrosis factor-alpha-mediated lipolysis in human fat cells. J Biol Chem 277(2):1085–1091
Prins JB, Niesler CU, Winterford CM, Bright NA, Siddle K, O’Rahilly S, Walker NI, Cameron DP (1997) Tumor necrosis factor-alpha induces apoptosis of human adipose cells. Diabetes 46(12):1939–1944
Ruan H, Hacohen N, Golub TR, Van Parijs L, Lodish HF (2002) Tumor necrosis factor-alpha suppresses adipocyte-specific genes and activates expression of preadipocyte genes in 3T3–L1 adipocytes: nuclear factor-kappaB activation by TNF-alpha is obligatory. Diabetes 51(5):1319–1336
Wang B, Trayhurn P (2006) Acute and prolonged effects of TNF-alpha on the expression and secretion of inflammation-related adipokines by human adipocytes differentiated in culture. Pflugers Arch 452(4):418–427
Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, Kitazawa S, Miyachi H, Maeda S, Egashira K, Kasuga M (2006) MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Invest 116(6):1494–1505
Kim CS, Park HS, Kawada T, Kim JH, Lim D, Hubbard NE, Kwon BS, Erickson KL, Yu R (2006) Circulating levels of MCP-1 and IL-8 are elevated in human obese subjects and associated with obesity-related parameters. Int J Obes (Lond) 30(9):1347–1355
Sartipy P, Loskutoff DJ (2003) Monocyte chemoattractant protein 1 in obesity and insulin resistance. Proc Natl Acad Sci USA 100(12):7265–7270
Trujillo ME, Scherer PE (2005) Adiponectin—journey from an adipocyte secretory protein to biomarker of the metabolic syndrome. J Intern Med 257(2):167–175
Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, Tataranni PA (2001) Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 86(5):1930–1935
Kern PA, Di Gregorio GB, Lu T, Rassouli N, Ranganathan G (2003) Adiponectin expression from human adipose tissue: relation to obesity, insulin resistance, and tumor necrosis factor-alpha expression. Diabetes 52(7):1779–1785
Wang B, Jenkins JR, Trayhurn P (2005) Expression and secretion of inflammation-related adipokines by human adipocytes differentiated in culture: integrated response to TNF-alpha. Am J Physiol Endocrinol Metab 288(4):E731–E740
Trayhurn P, Wang B, Wood IS (2008) Hypoxia and the endocrine and signalling role of white adipose tissue. Arch Physiol Biochem 114(4):267–276
Chiu KC, Chu A, Go VL, Saad MF (2004) Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 79(5):820–825
Bischof MG, Heinze G, Vierhapper H (2006) Vitamin D status and its relation to age and body mass index. Horm Res 66(5):211–215
Zemel MB, Sun X (2008) Calcitriol and energy metabolism. Nutr Rev 66(10 Suppl 2):S139–S146
Shi H, Norman AW, Okamura WH, Sen A, Zemel MB (2001) 1alpha, 25-Dihydroxyvitamin D3 modulates human adipocyte metabolism via nongenomic action. Faseb J 15(14):2751–2753
Shi H, Norman AW, Okamura WH, Sen A, Zemel MB (2002) 1alpha, 25-dihydroxyvitamin D3 inhibits uncoupling protein 2 expression in human adipocytes. Faseb J 16(13):1808–1810
Carlberg C, Seuter S (2009) A genomic perspective on vitamin D signaling. Anticancer Res 29(9):3485–3493
Sun X, Zemel MB (2007) 1Alpha, 25-dihydroxyvitamin D3 modulation of adipocyte reactive oxygen species production. Obesity (Silver Spring) 15(8):1944–1953
Zhang Z, Yuan W, Sun L, Szeto FL, Wong KE, Li X, Kong J, Li YC (2007) 1,25-Dihydroxyvitamin D3 targeting of NF-kappaB suppresses high glucose-induced MCP-1 expression in mesangial cells. Kidney Int 72(2):193–201. doi:10.1038/sj.ki.5002296
Giulietti A, van Etten E, Overbergh L, Stoffels K, Bouillon R, Mathieu C (2007) Monocytes from type 2 diabetic patients have a pro-inflammatory profile. 1,25-Dihydroxyvitamin D(3) works as anti-inflammatory. Diabetes Res Clin Pract 77(1):47–57
Chen Y, Kong J, Sun T, Li G, Szeto FL, Liu W, Deb DK, Wang Y, Zhao Q, Thadhani R, Li YC (2011) 1,25-Dihydroxyvitamin D suppresses inflammation-induced expression of plasminogen activator inhibitor-1 by blocking nuclear factor-kappaB activation. Arch Biochem Biophys 507(2):241–247
van Harmelen V, Skurk T, Hauner H (2005) Primary culture and differentiation of human adipocyte precursor cells. Methods Mol Med 107:125–135. doi:1-59259-861-7:125
Dicker A, Astrom G, Sjolin E, Hauner H, Arner P, van Harmelen V (2007) The influence of preadipocyte differentiation capacity on lipolysis in human mature adipocytes. Horm Metab Res 39(4):282–287
Dicker A, Kaaman M, van Harmelen V, Astrom G, Blanc KL, Ryden M (2005) Differential function of the alpha2A-adrenoceptor and Phosphodiesterase-3B in human adipocytes of different origin. Int J Obes (Lond) 29(12):1413–1421. doi:10.1038/sj.ijo.0803042
Mairal A, Langin D, Arner P, Hoffstedt J (2006) Human adipose triglyceride lipase (PNPLA2) is not regulated by obesity and exhibits low in vitro triglyceride hydrolase activity. Diabetologia 49(7):1629–1636. doi:10.1007/s00125-006-0272-x
Pettersson AT, Mejhert N, Jernas M, Carlsson LM, Dahlman I, Laurencikiene J, Arner P, Ryden M Twist1 in human white adipose tissue and obesity. J Clin Endocrinol Metab 96(1):133–141. doi:10.1210/jc.2010-0929
Sun X, Morris KL, Zemel MB (2008) Role of calcitriol and cortisol on human adipocyte proliferation and oxidative and inflammatory stress: a microarray study. J Nutrigenet Nutrigenomics 1(1–2):30–48
Wang B, Wood IS, Trayhurn P (2007) Dysregulation of the expression and secretion of inflammation-related adipokines by hypoxia in human adipocytes. Pflugers Arch 455(3):479–492
Wood IS, Wang B, Lorente-Cebrian S, Trayhurn P (2007) Hypoxia increases expression of selective facilitative glucose transporters (GLUT) and 2-deoxy-d-glucose uptake in human adipocytes. Biochem Biophys Res Commun 361(2):468–473. doi:10.1016/j.bbrc.2007.07.032
Sun X, Zemel MB (2007) Calcium and 1,25-dihydroxyvitamin D3 regulation of adipokine expression. Obesity (Silver Spring) 15(2):340–348
Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, Hotta K, Nishida M, Takahashi M, Muraguchi M, Ohmoto Y, Nakamura T, Yamashita S, Funahashi T, Matsuzawa Y (2000) Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation 102(11):1296–1301
Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, Mori Y, Ide T, Murakami K, Tsuboyama-Kasaoka N, Ezaki O, Akanuma Y, Gavrilova O, Vinson C, Reitman ML, Kagechika H, Shudo K, Yoda M, Nakano Y, Tobe K, Nagai R, Kimura S, Tomita M, Froguel P, Kadowaki T (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7(8):941–946
Zhang B, Berger J, Hu E, Szalkowski D, White-Carrington S, Spiegelman BM, Moller DE (1996) Negative regulation of peroxisome proliferator-activated receptor-gamma gene expression contributes to the antiadipogenic effects of tumor necrosis factor-alpha. Mol Endocrinol 10(11):1457–1466
Kruger S, Kreft B (2001) 1,25-dihydroxyvitamin D3 differentially regulates IL-1alpha-stimulated IL-8 and MCP-1 mRNA expression and chemokine secretion by human primary proximal tubular epithelial cells. Exp Nephrol 9(3):223–228
Zehnder D, Quinkler M, Eardley KS, Bland R, Lepenies J, Hughes SV, Raymond NT, Howie AJ, Cockwell P, Stewart PM, Hewison M (2008) Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation. Kidney Int 74(10):1343–1353. doi:10.1038/ki.2008.453
Sun X, Zemel MB (2008) Calcitriol and calcium regulate cytokine production and adipocyte-macrophage cross-talk. J Nutr Biochem 19(6):392–399
Ailhaud G (1997) Molecular mechanisms of adipocyte differentiation. J Endocrinol 155(2):201–202
Sun X, Zemel MB (2004) Role of uncoupling protein 2 (UCP2) expression and 1alpha, 25-dihydroxyvitamin D3 in modulating adipocyte apoptosis. FASEB J 18(12):1430–1432. doi:10.1096/fj.04-1971fje
Mahajan A, Stahl CH (2009) Dihydroxy-cholecalciferol stimulates adipocytic differentiation of porcine mesenchymal stem cells. J Nutr Biochem 20(7):512–520
Alvarez JA, Ashraf A (2010) Role of vitamin d in insulin secretion and insulin sensitivity for glucose homeostasis. Int J Endocrinol 351–385. doi:10.1155/2010/351385
Acknowledgments
This work has been supported by Nordic Centre of Excellence on “Systems biology in controlled dietary interventions and cohort studies, SYSDIET (No. 070014)”. MR, PA, and ID are supported by grants from the Swedish Research Council. MR and PA are also supported by grants from the NovoNordisk Foundation and the Swedish Diabetes Fund.
Conflict of interest
All the authors have read and approved submission of the manuscript and declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
S. Lorente-Cebrián and A. Eriksson contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lorente-Cebrián, S., Eriksson, A., Dunlop, T. et al. Differential effects of 1α,25-dihydroxycholecalciferol on MCP-1 and adiponectin production in human white adipocytes. Eur J Nutr 51, 335–342 (2012). https://doi.org/10.1007/s00394-011-0218-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-011-0218-z