Abstract
Purpose
To study the effects of a diet rich in salt and/or saturated fat on atrial natriuretic peptide (ANP)-granules, hypertension, renin expression, and cardiac structure in C57Bl/6 mice.
Methods
Young adult male mice were separated into four groups (n = 12) and fed one of the following for 9 weeks: standard chow/normal salt (SC-NS), high-fat chow/normal salt (HF-NS), standard chow/high salt (SC-HS) and high-fat chow/high salt (HF-HS). Alterations in the serum ANP, ultrastructural analysis of cardiomyocytes that produce ANP, structural analysis of the left ventricle, blood pressure, renin expression, glomerular filtration rate (GFR), feed efficiency, and lipid and glucose parameters were examined.
Results
The HF-NS diet showed a small increase in ANP production and left ventricular hypertrophy, increased food efficiency, and abnormal lipid and glucose parameters. The SC-HS diet showed a large increase in ANP granules in myocytes and corresponding elevation in ANP serum levels, left ventricular hypertrophy, hypertension, decrease in renin levels, and increase in GFR. The combination of the two diets (HF-HS) had an additive effect.
Conclusion
The incorporation of a high-fat high-salt diet induced ultrastructural changes in cardiomyocytes, increased the production of ANP and increased its serum level, and reduced the amount of renin in the kidney.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial natriuretic peptide (ANP) is a protein hormone produced, stored, and released by muscle cells in the upper chambers (atria) of the heart (atrial myocytes) in response to atrial stretch induced by hypervolemia or increases in blood pressure [1]. The overall effect of ANP on the body is to counter increases in blood pressure and volume by increasing the glomerular filtration rate, decreasing sodium reabsorption in the distal convoluted tubule and the cortical collecting duct of the nephron and inhibiting renin secretion [2].
The worldwide increase in obesity leads to an increase in related comorbidities like hypertension [3]. Furthermore, chronic intake of a diet with a high fat content is a major cause of hypertension and altered kidney structure [4, 5]. However, Western diets are high-fat and high-salt diets [6]. In a high-fat diet rat model of obesity, the concomitant intake of a high-salt diet accelerated the development of hypertension, increased oxidative stress, and induced kidney glomerulosclerosis and microalbuminuria with enhanced adipocyte hypertrophy and leptin production [7].
A mice model that mimics the human metabolic syndrome, C57BL/6, was submitted to a chronic intake of a very high-fat diet [8, 9]. Therefore, the present study was undertaken to investigate ANP production and the metabolic and structural consequences of a high-fat diet, a high-salt diet, and the combination of high-fat and high-salt diets in C57BL/6 mice.
Materials and methods
Animals and diets
Eight-week-old male C57BL/6 mice were kept under standard conditions (12-h light/dark cycles, 21 ± 2 °C) and had free access to food and water. The animals were studied for 9 weeks. The experimental protocols were approved by the local Ethics Committee to Care and Use of Laboratory Animals [CEA/254/2008]. The study was performed in accordance with the guidelines of Care and Use of Laboratory Animals (US National Institutes of Health 85-23, revised 1996).
Forty-eight animals were randomly separated into four groups based on the different diets offered: standard chow/normal salt (SC-NS, 76% carbohydrate, 14% protein, 10% fat from soybean oil, 0.25% NaCl, w/w; total energy 16.71 kJ/g, n = 12); high-fat chow/normal salt (HF-NS, 26% carbohydrate, 14% protein, 60% fat—50% from lard and 10% from soybean oil—0.25% NaCl, w/w; total energy 23,38 kJ/g, n = 12); standard chow/high-salt (SC-HS, 76% carbohydrate, 14% protein, 10% fat from soybean oil, 7.25% NaCl, w/w; total energy 16.71 kJ/g, n = 12); and high-fat chow/high-salt (HF-HS, 26% carbohydrate, 14% protein, 60% fat—50% from lard and 10% from soybean oil—7.25% NaCl, w/w; total energy 23,38 kJ/g, n = 12).
Diets were manufactured by PragSolucoes (Jau, SP, Brazil, www.pragsolucoes.com.br). Diet composition is in accordance with the American Institute of Nutrition’s recommendation (AIN-93M) [10]. Food intake was multiplied by chow energy (kilojoules per gram of chow) to obtain the daily energy intake per mice. Body mass and water intake were monitored weekly. The ratio of increased body mass (g)/total daily caloric intake (kJ) was used to determine the food efficiency.
Blood pressure
Systolic blood pressure (BP) was measured weekly in conscious mice with tail-cuff plethysmography (Letica LE 5100; Panlab, Barcelona, Spain). The average of three measurements at each time point was used. Two weeks before the experiment, the animals were put on the plethysmograph to minimize the stress caused by the procedure.
Blood and urine analysis
An oral glucose tolerance test (OGTT) was performed at weeks one and nine. After a 6-h fast, 25% glucose in sterile saline (0.9% NaCl) at 1 g/kg of body weight was administered by orogastric gavage. Blood samples were obtained from the tail tip by a small incision, and the plasma glucose concentration was measured before glucose gavage and later at 15, 30, 60, and 120 min after glucose administration (glucosimeter Accu-Chek Go, Roche Diagnostic, Mannheim, Germany).
In the ninth week, the animals were placed in metabolic cages and urine was collected for 24 h. Urinary and serum creatinine and urea were measured by a colorimetric assay (Bioclin, Belo Horizonte, MG, Brazil). The following parameters were assessed: creatinine clearance = 1,000 × [urine volume (mL)] × [concentration of creatinine in urine (mmol/L)]/[concentration of creatinine in serum (μmol/L)]; BUN (blood urea nitrogen) clearance = [urine volume (mL)] × [concentration of BUN in urine (mmol/L)]/[concentration of BUN in serum (mmol/L)]; and the glomerular filtration rate (GFR) = mean of (creatinine clearance and BUN clearance) [11].
Euthanasia
One day before euthanasia, animals were food deprived for 6 h and then anesthetized (intraperitoneal sodium pentobarbital, 150 mg/kg). A blood sample was collected by cardiac puncture. Plasma was obtained by centrifugation (120 g for 15 min) at room temperature and stored at −20 °C until the assay was performed. Total cholesterol, triacylglycerols, creatinine and urea were measured by a colorimetric assay (Bioclin, Belo Horizonte, MG, Brazil). The heart and kidney were immediately dissected.
Plasma insulin radioimmunoassay
The fasting insulin concentration was measured using an insulin radioimmunoassay kit (insulin ImmuChem-coated tube radioimmunoassay kit, MP Biomedicals, Solon, OH, USA) with an intra-assay coefficient of variation of 1.4%. Insulin resistance (IR) was estimated by the homeostasis model assessment index as HOMA-IR = (insulin × glucose)/22.5 [12]. Total cholesterol and triglycerides were measured by a colorimetric assay (Bioclin, Belo Horizonte, MG, Brazil).
ELISA
ANP was assayed by ELISA (Phoenix Pharmaceuticals, Inc., Belmont, CA, USA). Briefly, 50 μL of plasma was added to 25 μL of rehydrated primary antiserum plus 25 μL of biotinylated peptide. After incubation for 2 h at room temperature, the plate was washed three times, and 100 μL of SA-HRP solution was added to each sample, followed by incubation for 1 h at room temperature. The plate was washed three times, and 100 μL of TMB solution was added to each sample. After 30 min, 100 μL of stop solution was added to each sample, and the absorbance at 450 nm was determined.
Light microscopy and transmission electron microscopy
Left ventricle
The atria were separated from the ventricles. The ventricles were put into freshly prepared 1.27 mol/L formaldehyde (0.1 M phosphate-buffered, pH 7.2) for 48 h. Random fragments from the left ventricle (LV) were embedded in Paraplast plus (Sigma–Aldrich, St. Louis, MO, USA), sectioned (5 μm), and stained with hematoxylin and eosin. Slices were analyzed by video-microscopy (Leica DMRBE microscope, Wetzlar, Germany, videocamera Infinity, Media cybernetics, Silver Spring, MD, USA). Cardiomyocyte (cmy) mean cross-sectional area was estimated as:
The volume density of cardiomyocytes (V v[cmy]) was estimated by point counting:
where P p is the number of points that hit the cardiomyocytes and P T is the total number of test points.
where N is the number of cmy profiles counted inside the test frame (considering the forbidden line and its extensions), and A T is the test frame area [13].
Right auricle
Fragments of the right atrium auricle containing the pectinate muscle were cut and fixed in 2.5% glutaraldehyde, 0.1 M cacodylate buffer, pH 7.2 for 2 h at room temperature and post-fixed in 1% osmium tetroxide in the same buffer for 2 h at room temperature. Then, the fragments were dehydrated through an increasing graded series of acetone and embedded in Epon. Ultrathin sections were obtained using a Leica ultracut ultramicrotome and collected on a copper grid. All fragments were counterstained with uranyl acetate and lead citrate and observed with a Zeiss EM 906 microscope.
The numerical density per area of ANP granules (Q A[ANP]) was estimated as the number of ANP granule profiles within a frame of a known area (expressed as granules/μm2), as mentioned before, on 25 electron micrographs per group.
Confocal laser scanning microscopy
The kidney was analyzed for immunofluorescence of renin. Antigen retrieval was performed using citrate buffer, pH 6.0 at 60 °C, and then blocked with ammonium chloride, 2% glycine, and phosphate buffer, pH 7.4 (PBS). Sections were incubated with a primary antibody specific for mouse renin 1:100 (38 kDa; sc-3806; Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight at 4 °C. Then, the samples were incubated for 1 h at room temperature with the fluorochrome-conjugated secondary antibody donkey anti-mouse IgG-Alexa 488 1:100 (Invitrogen, Molecular Probes, Carlsbad, CA, USA). After rinsing in PBS, the slides were mounted with DAPI Nucleic Acid Stain and SlowFade Antifade Kit (Invitrogen, Molecular Probes, Carlsbad, CA, USA). Indirect immunofluorescence was observed with the Zeiss Confocal Laser Scanning Microscopy - LSM 510 Meta, Germany.
Western blot analysis
Total kidney proteins were extracted in homogenizing buffer with protease inhibitors. The homogenate was centrifuged at 5,000g for 20 min at 4 °C, and the supernatant was collected. The total amount of protein in the sample was quantified using the BCA Assay Kit (Thermo Scientific, #23225, Rockford, IL, USA). Proteins were denatured in SDS-containing buffer (5 min at 100 °C), and 10 μg of protein from each sample was separated by SDS/PAGE. After electrophoresis, proteins were electroblotted onto PVDF transfer membranes (Hybond-P, Amersham Biosciences, Piscataway, NJ, USA), and the membrane was blocked by incubation in 6% (w/v) non-fat dry milk in Tris-buffered saline containing 0.05% Tween 20. Then, the membrane was incubated with a monoclonal antibody against mouse renin (38 kDa; sc-3806; Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight at 4 °C, followed by secondary goat anti-mouse IgG-HRP antibody (sc-2031; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Finally, the membrane was exposed to ECL for 5 min, the signal was visualized by autoradiography and quantified using the software Image Pro plus version 7.0 (Media cybernetics, Silver Spring, MD, USA).
Data analysis
Differences among groups were tested by one-way analysis of variance and post hoc test of Tukey (Statistica version 7.0, Statsoft, Tulsa, OK, USA). A P value ≤ 0.05 was considered statistically significant.
Results
Body mass gain and food behavior (Table 1)
At the start of the experiment, animals had similar body masses (23.8 ± 0.1 g, mean and standard error of the mean). The HF intake induced larger body mass gains in the HF-NS and HF-HS groups, completing the experiment with a BM around three times greater than that of SC-NS and SC-HS groups (P < 0.01).
The HF-NS group took in 14% less food daily than the SC-NS group, but with a higher energy intake (21% more) and feed efficiency (210%) (P < 0.01). Likewise, HF-HS took in 9% less food daily than the SC-NS group, but with a higher energy intake (19% more) and feed efficiency (161%) (P < 0.01). Interestingly, salt intake was accompanied by an increase of 18% in the daily food intake and by 10% in the energy intake, while feed efficiency was reduced by 24%, comparing the SC-NS group to the SC-HS group (P < 0.05). Water intake was increased in the high-salt groups in comparison with the normal-salt counterparts (182% in SC groups, and 105% in HF groups) (P < 0.0001).
Metabolism (Table 1)
High-fat intake was accompanied by a proportional increase in TC and TG. TC was 25% greater in the HF-NS group and 27% greater in the HF-HS group, compared to their SC counterparts (P < 0.05). No difference was observed between SC-NS and SC-HS and between HF-NS and HF-HS. TG was 54% greater in HF-NS and 31% greater in HF-HS than their SC counterparts (P < 0.05). No difference was observed between SC-NS and SC-HF and between HF-NS and HF-HS.
Concerning the OGTT, the area under the curve was 24% greater in HF-NS than in SC-NS and 32% greater in HF-HS than in SC-HS (P < 0.05), indicating glucose intolerance in the HF groups.
HF intake increased fasting insulin. It was 43% greater in the HF-NS group and 66% greater in the HF-HS group than in the SC-NS group, with the HOMA-IR increasing accordingly (P < 0.05). No difference in fasting insulin or HOMA-IR was observed between the SC-NS and SC-HS groups.
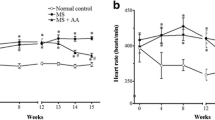
Blood pressure (Fig. 1)
Animals began the experiment with a similar BP (129.9 ± 1.4 mmHg, systolic blood pressure). After 9 weeks of the experiment, no difference was observed between the SC-NS and HF-NS groups or between the SC-HS and HF-HS groups. However, BP was higher by approximately 40% in both the SC-HS and the HF-HS groups than in their NS counterparts (P < 0.05).
Cardiac hypertrophy and blood pressure analysis: a–d Left ventricle cross-sections. The left ventricle wall thickness increased from the SC-NS group to the HF-HS group, indicating cardiac hypertrophy; e blood pressure (BP) evolution. Animals started the experiment with no difference in BP. After a week with SC-HS or HF-HS diet, mice showed elevated BP compared to SC-NS and HF-NS animals. The difference was maintained during the 9 weeks of the experiment. There was no difference between the groups SC-NS and HF-NS, or between the groups SC-HS and HF-HS, so that they were divided into two major groups (indicating into de rectangles). These differences persisted throughout the experiment (*P < 0.05) (one-way ANOVA and post hoc test of Tukey, n = 12 each group). Groups: a SC-NS standard chow-normal salt, b HF-NS high-fat chow-normal salt, c SC-HS standard chow-high-salt, d HF-HS high-fat chow-high-salt
Cardiac hypertrophy (Fig. 1 and Table 1)
Cardiac hypertrophy was analyzed by LV wall thickness and cardiomyocyte cross-sectional area (A[cmy]). Cardiac hypertrophy in HF and HS groups can easily be confirmed, as shown in Fig. 1. Consequently, the A[cmy] shows an increase of 29% in the HF-NS group and an increase of 93% in the HF-HS group, compared to the SC-NS group (P < 0.0001). No difference was observed in A[cmy] between the SC-HS and HF-HS groups (Table 1).
Atrial natriuretic peptide
Serum ANP levels (Table 1)
Salt intake increased serum ANP levels. It was 100% higher in the SC-HS group and 90% higher in the HF-HS group, compared to their NS counterparts (P < 0.01). HF intake also increased serum ANP levels by 70% in the HF-NS group, compared to the SC-NS group (P < 0.03). However, no difference in serum ANP level was observed between the SC-HS and HF-HS groups.
ANP in cardiomyocytes (Fig. 2)
The ultrastructural appearance of ANP granules in each group and the features of cardiac hypertrophy in the HF-HS group are shown in Fig. 2. The numerical density per area of ANP granules in right auricle cardiomyocytes, compared to the SC-NS group, was 124% greater in the HF-NS group, 351% greater in the SC-HS group, and 340% greater in the HF-HS group (P < 0.01).
Electron micrographs of the right auricle cardiomyocytes and estimation of the density of ANP granules: a SC-NS group; b HF-NS group; c and d HF-HS group. An increase in density per area of ANP granules (arrows) was observed from SC-NS to HF-HS. Regular myofilaments and numerous and organized mitochondria were present in SC-NS, but hypertrophied cardiomyocytes with irregular myofilaments (open arrow) and swollen and disorganized mitochondria were present in cardiomyocytes from mice on a HF-HS diet; e numerical density per area of ANP granules (mean and standard error of the mean, n = 5 each group). Differences were analyzed with one-way ANOVA and post hoc test of Tukey. In signaled cases, P < 0.05, † when compared to SC-NS; ‡ or compared to HF-NS. Groups: SC-NS standard chow, normal salt; HF-NS high-fat chow, normal salt; SC-HS standard chow, high-salt; and HF-HS high-fat chow, high-salt. de desmosome, ca capillary, m mitochondria, nu cardiomyocyte nucleus
Renin expression in the kidney (Fig. 3)
No difference in renin expression was observed between the SC-NS and HF-NS groups. However, both the SC-HF group (23% less) and the HF-HS (29% less) group showed decreased renin expression than their counterparts (P < 0.0001) (Fig. 3). Immunofluorescence for renin in the kidney confirmed these results, as observed by confocal laser scanning microscopy (Fig. 3).
Kidney Analysis. a Confocal laser scanning microscopy of kidney sections stained for renin. Glomeruli are marked with arrows. Renin expression (open arrows) was observed near the macula densa. Renin expression decreased in normal salt groups compared to the high-salt groups. b Kidney renin expression. A representative immunoblot is shown above, with the quantification of the bands in a bar graph. Data were standardized to beta-actin expression (bottom bands) (mean and standard error of the mean, n = 5 each group). Differences were analyzed with one-way ANOVA and post hoc test of Tukey. In signaled cases, P < 0.05, a when compared to SC-NS; b compared to HF-NS. Groups: SC-NS standard chow, normal salt; HF-NS high-fat chow, normal salt; SC-HS standard chow, high-salt; and HF-HS high-fat chow, high-salt
Renal function (Table 1)
Major alterations in renal function were due to HS intake. HS diets increased diuresis by 180% in the SC-HS group and by 108% in the HF-HS group than in their NS counterparts (P < 0.01). Urinary creatinine was 38% higher in the SC-HS group and 58% higher in the HF-HS group than in their NS counterparts (P < 0.01). Serum creatinine decreased by around 10% in both the SC-HS and the HF-HS groups in comparison with the SC-NS group (P < 0.05), resulting in a creatinine clearance more than 65% higher in both the SC-HS and HF-HS groups, compared to their counterparts (P < 0.05).
HS diets increased urinary BUN by more than 60% in both the SC-HS and HF-HS groups, compared to their counterparts (P < 0.05). However, serum BUN was 13% lower in the SC-HS group and 9% lower in the HF-HS group than their NS counterparts (P < 0.05). Consequently, the BUN clearance increased more than 90%, and the GFR increased more than 80% in both SC-HS and HF-HS groups in comparison with their counterparts (P < 0.01).
Discussion
In the present study, a HS diet increased GFR and induced cardiac hypertrophy, but it was not aggravated or mitigated by HF intake. A HS diet led to ultrastructural alterations to cardiomyocytes, compatible with cardiac hypertrophy accompanied by increased production of ANP. Simultaneously, a HS diet decreased renin expression in the kidney, indicating that RAS is involved in this alimentary protocol.
The HF diet in the present study led to overweight/obese mice, which agrees with recent studies [14, 15]. Obesity is an import metabolic and cardiovascular risk factor that should not be neglected, even though the HS diet in this study was more directly related to hemodynamic and renal function alterations.
The high-fat diet increased the levels of plasma triacylglycerols and LDL-C, which is an important risk factor for developing atherosclerosis and coronary artery disease, especially in patients suffering from a metabolic syndrome [16, 17]. Moreover, the wide release of fatty acids in portal and systemic circulation due to the high lipolytic activity of visceral fat, with the production of proinflammatory cytokines and pro-atherogenic factors, reduces glucose uptake in the liver, skeletal muscle and other tissues, causing a condition of high cardiometabolic risk [18]. The presence of insulin resistance and compensatory hyperinsulinemia predisposes individuals to several metabolic and hemodynamic disorders [19]. In Dahl rats, a model of BP salt sensitivity, insulin resistance precedes BP elevation and sodium overload that anticipates the emergence of hypertension [20]. In the present study, insulin resistance caused by a HF diet may be associated with cardiac overload and the small increase in ANP synthesis, although BP did not change significantly.
Left ventricular hypertrophy was observed mainly in high salt-fed mice, whereas the high-fat diet induced a slight increase in left ventricular size. Unfortunately, the mechanism that causes heart hypertrophy in animals on a high-salt diet is not fully understood. It has been suggested that cardiac hypertrophy could simply be the consequence of hypertension with increased serum aldosterone or local RAS activation [21, 22]. Moreover, obesity in HF mice is known to produce an increase in total blood volume and cardiac output because of the high metabolic activity of excessive fat. In moderate-to-severe cases of obesity, this may lead to left ventricular dilation, increased left ventricular wall stress, and compensatory left ventricular hypertrophy [23, 24].
We did not observe an enhancement or decrease in cardiac hypertrophy caused by excessive salt on a HF intake, although a previous study has observed the contrary in another animal model. Dahl salt-sensitive rats fed either a low-fat or a HF diet on either low-salt or HS chow for 12 weeks showed that an increased dietary lipid intake reduced cardiac growth, left ventricular remodeling, contractile dysfunction, and alterations in gene expression in response to hypertension [25]. In the present study, the normal compensatory mechanism to control BP increase by ANP secretion was surpassed by HS intake.
The density of ANP granules increased in mice on a HF-HS diet. Previous studies have associated increased ANP synthesis with elevated blood pressure and cardiac hypertrophy [26], consistent with the present data. Moreover, circulating ANP levels increased in correlation with the density of ANP granules in right auricle cardiomyocytes. In the cases of perinatal malnutrition, the numerical density of ANP-granules in the cardiomyocytes is not affected, but a significant reduction in the sizes of granules [27]. Importantly, the use of deep anesthesia with pentobarbital is not reported in the literature that affects the blood levels of renin or ANP.
Renin expression in the kidney decreased in mice on an HS diet. This suggests that hypervolemia induced by a HS diet could induce the kidney to produce less renin. Furthermore, the increase in creatinine clearance, urea, and consequently GFR, suggests glomerular injury from the exposure to HF and HS diets. This subject seems to be complex, as elements of RAS are expressed along the entire nephron, including angiotensinogen secreted by the proximal tubule and renin expressed in the connecting tubule, may participate in the regulation of sodium reabsorption at multiple sites of the nephron. The response of tubular RAS to stepwise changes in dietary sodium has been investigated in two mouse strains (salt-sensitive C57BL/6 and salt-resistant CD1), resulting in no alteration in plasma angiotensinogen by a sodium regimen, whereas plasma renin increased twofold under low sodium. Angiotensinogen and renin excretion were significantly higher under high sodium than under low sodium conditions. C57BL/6 mice exhibited significantly higher urinary excretion of angiotensinogen than did CD1 animals under either condition of sodium intake. The extent to which these urinary parameters reflect systemic or tubular responses to challenges of sodium homeostasis may depend on the relative contribution of sodium restriction and volume depletion [28].
In conclusion, the present findings suggest that the association of HF and HS diets can induce elevated BP and concomitant ultrastructural changes in cardiomyocytes, raising the production of ANP, altering blood lipids and carbohydrate metabolism, and reducing kidney renin expression. Therefore, HF-HS intake by mice mimics Western food consumption nowadays and could be considered a reliable model of a cluster of symptoms of so-called ‘metabolic syndrome’ in humans.
References
Nicholls MG, Espiner EA, Ikram H, Crozier IG, Richards AM (1987) Atrial natriuretic peptide in human hypertension. Eur Heart J 8(Suppl B):123–128
Zhao D, Pandey KN, Navar LG (2010) ANP-mediated inhibition of distal nephron fractional sodium reabsorption in wild-type and mice overexpressing natriuretic peptide receptor. Am J Physiol Renal Physiol 298:F103–F108
Aneja A, El-Atat F, McFarlane SI, Sowers JR (2004) Hypertension and obesity. Recent Prog Horm Res 59:169–205
Aguila MB, Mandarim-de-Lacerda CA (2003) Effects of chronic high fat diets on renal function and cortical structure in rats. Exp Toxicol Pathol 55:187–195
Aguila MB, Mandarim-de-Lacerda CA (2003) Heart and blood pressure adaptations in Wistar rats fed with different high-fat diets for 18 months. Nutrition 19:347–352
Beilin LJ (1999) Lifestyle and hypertension—an overview. Clin Exp Hypertens 21:749–762
Dobrian AD, Schriver SD, Lynch T, Prewitt RL (2003) Effect of salt on hypertension and oxidative stress in a rat model of diet-induced obesity. Am J Physiol Renal Physiol 285:F619–F628
Fraulob JC, Ogg-Diamantino R, Fernandes-Santos C, Aguila MB, Mandarim-de-Lacerda CA (2010) A mouse model of metabolic syndrome: insulin resistance, fatty liver and non-alcoholic fatty pancreas disease (NAFPD) in C57BL/6 mice fed a high fat diet. J Clin Biochem Nutr 46:212–223
Gallou-Kabani C, Vige A, Gross MS, Rabes JP, Boileau C, Larue-Achagiotis C, Tome D, Jais JP, Junien C (2007) C57BL/6J and A/J mice fed a high-fat diet delineate components of metabolic syndrome. Obesity (Silver Spring) 15:1996–2005
Reeves PG, Nielsen FH, Fahey GC Jr (1993) AIN-93 purified diets for laboratory rodents: final report of the American Institute of Nutrition ad hoc writing committee on the reformulation of the AIN-76A rodent diet. J Nutr 123:1939–1951
Pestel S, Krzykalla V, Weckesser G (2007) Measurement of glomerular filtration rate in the conscious rat. J Pharmacol Toxicol Methods 56:277–289
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Mandarim-de-Lacerda CA, Fernandes-Santos C, Aguila MB (2010) Image analysis and quantitative morphology. Methods Mol Biol 611:211–225
Atshaves BP, McIntosh AL, Storey SM, Landrock KK, Kier AB, Schroeder F (2010) High dietary fat exacerbates weight gain and obesity in female liver fatty acid binding protein gene-ablated mice. Lipids 45:97–110
Gregorio BM, Souza-Mello V, Carvalho JJ, Mandarim-de-Lacerda CA, Aguila MB (2010) Maternal high-fat intake predisposes nonalcoholic fatty liver disease in C57BL/6 offspring. Am J Obstet Gynecol 203:495 e491–495 e498
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. Jama 288:2709–2716
McDonald M, Hertz RP, Unger AN, Lustik MB (2009) Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci 64:256–263
Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodes-Cabau J, Bertrand OF, Poirier P (2008) Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol 28:1039–1049
Reaven GM (2005) Insulin resistance, the insulin resistance syndrome, and cardiovascular disease. Panminerva Med 47:201–210
Shehata MF (2008) Genetic and dietary salt contributors to insulin resistance in Dahl salt-sensitive (S) rats. Cardiovasc Diabetol 7:7
Bayorh MA, Ganafa AA, Emmett N, Socci RR, Eatman D, Fridie IL (2005) Alterations in aldosterone and angiotensin II levels in salt-induced hypertension. Clin Exp Hypertens 27:355–367
Le Corvoisier P, Adamy C, Sambin L, Crozatier B, Berdeaux A, Michel JB, Hittinger L, Su J (2010) The cardiac renin-angiotensin system is responsible for high-salt diet-induced left ventricular hypertrophy in mice. Eur J Heart Fail 12:1171–1178
Alpert MA (2001) Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321:225–236
Singh R, Krishan P (2010) Modulation of impact of high fat diet in pathological and physiological left ventricular cardiac hypertrophy by fluvastatin. Biomed Pharmacother 64:147–153
Okere IC, Young ME, McElfresh TA, Chess DJ, Sharov VG, Sabbah HN, Hoit BD, Ernsberger P, Chandler MP, Stanley WC (2006) Low carbohydrate/high-fat diet attenuates cardiac hypertrophy, remodeling, and altered gene expression in hypertension. Hypertension 48:1116–1123
Yuan K, Kim SY, Oh YB, Yu J, Shah A, Park BH, Kim SH (2010) Upregulation of ANP and NPR-C mRNA in the kidney and heart of eNOS knockout mice. Peptides 31:1319–1325
Gama EF, Liberti EA, de Souza RR (2007) Effects of pre- and postnatal protein deprivation on atrial natriuretic peptide- (ANP-) granules of the right auricular cardiocytes. An ultrastructural morphometric study. Eur J Nutr 46:245–250
Lantelme P, Rohrwasser A, Gociman B, Hillas E, Cheng T, Petty G, Thomas J, Xiao S, Ishigami T, Herrmann T, Terreros DA, Ward K, Lalouel JM (2002) Effects of dietary sodium and genetic background on angiotensinogen and Renin in mouse. Hypertension 39:1007–1014
Acknowledgments
The authors thank Mss. Nemesis M. L. S. Monteiro and Mr. Eduardo M. Costa, for their help in the care of the animals. Furthermore, they thank Mrs. Thatiany Marinho and Angelica Figeuiredo for their technical assistance. This research was supported by grants from Brazilian agencies, CNPq (Conselho Nacional de Ciencia e Tecnologia, Ministerio da Ciencia e Tecnologia, Brazil) and FAPERJ (Fundaçao do Amparo a Pesquisa do Estado do Rio de Janeiro).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, M.V., Fernandes-Santos, C., Faria, T.d.S. et al. Diets rich in saturated fat and/or salt differentially modulate atrial natriuretic peptide and renin expression in C57BL/6 mice. Eur J Nutr 51, 89–96 (2012). https://doi.org/10.1007/s00394-011-0196-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-011-0196-1