Abstract
Background
A long-term vegetarian diet is generally poor in vitamin B group. The lack of vitamin B12 together with vitamin B6 and folate deficiency is closely related to homocysteine metabolism. Hyperhomocysteinemia was found to be associated with increased bone turnover markers and increased fracture risk. Thus, hyperhomocysteinemia, vitamin B12 and folate deficiency may be regarded as novel risk factors for micronutrient deficiency-related osteoporosis.
Aim of the study
To assess the possible impact of a vegetarian diet on bone mineral density in cohort of Slovak vegetarian women.
Methods
Fasting serum glucose, albumin, calcium, phosphorous and creatinine as well as bone markers, serum vitamin B12, folate and plasma levels of total homocysteine were assessed in two nutritional groups (vegetarians vs. nonvegetarians) of apparently healthy women (age range 20–70 years). Bone mineral density of the femoral neck, trochanter, total femur and lumbar spine was measured in all subjects.
Results
Vegetarians had a significantly lower weight (p < 0.05), higher PTH (p < 0.01) and homocysteine (p < 0.001). Vitamin B12 was significantly higher in nonvegetarians (p < 0.001). No differences were observed in folate levels. Univariate analysis showed significant association between homocysteine and B12 (p < 0.01), folate (p < 0.001), creatinine (p < 0.001), total proteins (p < 0.049), age (p < 0.001) and vegetarian food intake (p < 0.001). Vegetarians had a significantly lower TrFBMD (p < 0.05) and ToFBMD (p < 0.05). Age and CTx were significant predictors in all sites of measured BMD and PTH. A strong correlation between homocysteine and FNBMD (r = −0.2009, p < 0.002), TrFBMD (r = −0.1810, p < 0.004) and ToFBMD (r = −0.2225, p < 0.001) was found in all subjects.
Conclusion
Homocysteine is one of the predictors of bone mineral density, and hyperhomocysteinemia is associated with lower bone mineral density. In healthy adults, homocysteine levels are dependent on age as well as on nutritional habits. Thus, elderly women on a vegetarian diet seem to be at higher risk of osteoporosis development than nonvegetarian women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoporosis is a complex multi-factorial condition characterized by reduced bone mass and impaired micro-architectural structure, leading to an increased susceptibility to fractures. Several factors are thought to influence bone mass. These can be broadly grouped into factors that cannot be modified, such as gender, age, body (frame) size, genetics, and ethnicity; and those factors that can be modified, such as hormonal status (especially sex and calciotropic hormone status), lifestyle factors including physical activity levels, smoking and alcohol consumption patterns, and diet. Nutrition plays an important role in the acquisition and maintenance of skeletal integrity. The vegetarian lifestyle has become very popular in recent years. There is some evidence that a well-balanced vegetarian diet may be consistent with good health and can potentially reduce the risk of cardiovascular disease, hypertension, diabetes, cancer and some other chronic diseases [28, 30]. On the other hand, people following a long-term vegetarian diet very often suffer from nutrient shortage like calcium, phosphorous, iron, zinc, vitamin D or vitamin B12 [9, 31]. The lack of vitamin B12 together with vitamin B6 and folate deficiency is closely related to homocysteine (Hcy) metabolism. Hyperhomocysteinemia was found to be associated with increased bone turnover markers [6] and increased fracture risk [17, 20, 25, 32]. Thus, homocysteine, vitamin B12 and folate may be regarded as novel risk factors for micronutrient deficiency-related osteoporosis [14]. Most of the individuals examined in these studies were postmenopausal women. High Hcy plasma levels in elderly people are due to age-related decline of renal function as well as low vitamin B status. In the elderly, high prevalence of atrophic gastritis results in less absorption of vitamin B12 with consequent vitamin B12 deficiency [33]. Unlike them, vegetarians suffer from deficiency of vitamin B and increasing plasma Hcy independent of age as a result of low intake of animal food.
In contrast to fracture risk, the association between Hcy and BMD is still in doubt [5–7, 20, 21, 32]. In addition, we did not find any work in the literature, where the relationship between Hcy and BMD is evaluated directly in vegetarians. The majority of authors dealing with the questions of bone metabolism in vegetarians focus mostly on possible insufficiency of several nutrients such as vitamin D, Ca or animal proteins.
The aim of our study was to assess the possible impact of a vegetarian diet on bone mass density in a cohort of Slovak vegetarian women. We hypothesized that increased concentrations of homocysteine in vegetarian women can significantly increase the risk of decreased BMD, especially in older women, compared with nonvegetarian women.
Methods
The study was performed on a group of 141 women on long-term ovo-lacto-vegetarian diet and a control group of 131 women on standard western diet. All women were apparently healthy non-smokers with normal weight, similar physical load and living standard. Both groups were age matched. The study was carried out during spring. No supplementation of vitamins, mineral and trace elements was allowed. The Regional Ethics Committee approved the study, and all participants gave their written informed consent.
Fasting blood samples were taken for the measurements of serum biochemical parameters. Serum glucose (Glu), albumin (Alb), calcium (Ca), phosphorous (P) and creatinine (Cr) concentrations were assessed by a standard laboratory method on Vitros 250 autoanalyzer (Johnson & Johnson, NY, USA). Parathormone (PTH; Immunotech, France) was determined by RIA method with intra-assay variability 7.5% and interassay variability 11%. The detection limit was 2 pg/ml. Measurement of osteocalcin (OC) was performed by sandwich immunoradioassay (OSTEO-RIACT, Cis bio international, France) with intra-assay variability 1.2–2.8%, inter-assay variability 3.6–5.2% and detection limit 0.4 ng/ml. C-terminal telopeptides of type-I collagen (CTx) were determined by using commercial competitive enzyme immunoassay (Serum CrossLaps ELISA, Nordic Bioscience Diagnostic A/S, Denmark). The intra-assay and inter-assay variability of CTx were 6.5–8.1 and 5.0–5.4%, respectively. The detection limit was 0.02 ng/ml. Serum vitamin B12 and folate were determined using Elecsys 2010 System (Roche Diagnostics, Switzerland). The intra-assay and inter-assay variability of vitamin B12 were 3.0–8.7 and 3.7–9.4%, respectively. The detection limit was 22 pmol/l. The intra-assay variability of folate was 3.0–7.0% and inter-assay variability was 5.0–13.3%. The detection limit was 1.45 nmol/l. Plasma levels of total homocysteine (Hcy) was measured by HPLC method [15]. The intra-assay and inter-assay variability were <3 and <4%, respectively with detection limit 1.0 μmol/l.
Bone mineral density (BMD) of the femoral neck (NFBMD), trochanter (TrFBMD), total femur (ToFBMD) and lumbar spine (L1–4BMD) was measured in all probands by dual-energy X-ray absorptiometry (DEXA) using a Lunar DPX-L bone densitometer (Lunar Co., Madison, WI, USA). BMD was expressed in absolute values (g/cm2).
Data analysis
The statistical evaluation was performed using Statistical Package for the Social Sciences software (SPSS 12.0, Chicago, IL, USA). The distribution of investigated variables were estimated using Kolgomorov–Smirnov test. For descriptive purposes, the quantitative data is presented as mean ± SD. The significance of differences was determined by unpaired Student’s t test, two tailed. The univariate linear model was used to calculate the predictors of Hcy concentrations. The stepwise multiple regression model was applied to evaluate the relationship between BMD in all measured sites and various variables. The relationship between serum values of Hcy concentrations and BMD were investigated by linear regression analysis and Pearson’s correlation coefficient (p). p values < 0.05 were considered to indicate statistical significance.
Results
Demographics and clinical characteristics of studied women are summarized in Table 1. Probands were divided into two groups according to nutritional habits. Vegetarians did not differ from nonvegetarians in age, height and BMI, but their weight was found to be significantly lower (p < 0.05). Basic biochemical parameters were in normal range in all study probands with no differences between separate groups. CTx and OC levels were similar in both groups. Vegetarian women had a significantly higher PTH (p < 0.01).
Homocysteine concentrations were beyond the normal range in both groups (<12.0 μmol/l) but significantly higher in vegetarians (p < 0.001). Hyperhomocysteinemia was found in 78% of vegetarians and in 48% of nonvegetarians. The mean vitamin B12 levels were in normal range in both groups (>220 pmol/l) with significantly higher concentrations in nonvegetarians (p < 0.001). Up to 48% of vegetarians and 28% of nonvegetarians did not reach a normal value of plasma vitamin B12. Folate concentrations were in normal range with no significant differences between groups. Results from univariate analysis show the variables associated with plasma homocysteine (Table 2). Homocysteine was significantly associated with vitamin B12 (p < 0.01), folate (p < 0.001), creatinine (p < 0.001), total proteins (p < 0.049), age (p < 0.001) and a vegetarian diet (p < 0.001).
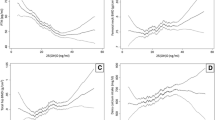
The mean BMD values of the femoral neck (NFBMD), femoral trochanter (TrFBMD), total femur (ToFBMD) and lumbar spine (L1–4BMD) are given in Table 3. Vegetarians had a significantly lower TrFBMD (p < 0.05) and ToFBMD (p < 0.05) and did not differ in NFBMD and L1–4BMD. A stepwise multiple regression analysis was performed to determine the main predictors of the femur and lumbar spine BMD. (Table 4). Age and CTx were significant predictors in all sites of measured BMD, PTH in TrFBMD and ToFBMD, Hcy in TrFBMD and ToFBMD and serum creatinine in L1-4BMD. Homocysteine significantly correlated with FNBMD (r = −0.2009, p < 0.002), TrFBMD (r = −0.1810, p < 0.004) and ToFBMD (r = −0.2225, p < 0.001) in all groups, after the selection of vegetarians and nonvegetarians, significant correlations were confirmed only in nonvegetarian women (Table 5). No significant correlations were found between vitamin B12 and BMD as well as between folate and BMD.
Discussion
Hyperhomocysteinemia (HHcy) is a condition of elevated plasma Hcy concentration. It is a sensitive functional marker of inadequate cellular folate and vitamin B12 concentrations. In the general population, mild HHcy is a common condition. Higher levels of plasma homocysteine are caused either by genetic defects in the enzymes involved in homocysteine metabolism (cystathionine β-synthase, MTHFR) or by nutritional deficiencies in vitamin cofactors. It has been speculated that deficiencies of B-group vitamins contribute to approximately two-thirds of all cases of HHcy [27]. In our study, 45% of controls and up to 78% of vegetarian women were found to attain homocysteine concentrations above the 12 μmol/l cutoff [29]. Twenty-eight percent of controls and 47% of vegetarian women suffered from vitamin B12 deficiency. This data is similar to those of Majchrzak et al. [18] and Koebnick et al. [16]. HHcy is age dependent and in elderly people is also related to age-dependent decline in renal function [24]. Our results confirmed a strong association between Hcy and variables including vitamin B12, folate, age, creatinine and vegetarian diet.
HHcy is recognised as an important marker for cardiovascular risk [19] as well as for cognitive impairment [30]. Recently, homocysteine has been linked to be a potential risk factor for osteoporosis. This hypothesis was suggested from the observation of a high prevalence of osteoporosis in patients with homocystinuria [8, 22]. Most of published data is concerned with the relationship between elevated Hcy values and higher prevalence of fracture risk, even though some of them are contradictory [17, 20, 23, 32]. In an Iranian study with 271 postmenopausal women, Golbahar et al. [7] found a significant negative association of plasma Hcy with BMD at both femoral neck and lumbar spine and a positive association of plasma folate with BMD at the femoral neck. These associations remained significant when adjusted for age, BMI and creatinine. Gerdhem et al. [5] reported significant associations between high Hcy, high bone marker levels and low BMD at the femoral neck and trochanter in 996 women 75 years old. The negative association of Hcy with BMD was also confirmed in the study of Elshorbagy et al. [4] on 5,238 men and women in two groups aged 40–42 and 65–67 years as well as in the study of Bozkurt et al.[2] in Turkish postmenopausal women. These results are inconsistent with those of van Meurs et al. [32] and Herrmann et al. [10]. They reported that neither hip nor lumbar spine DXA results were associated with Hcy levels. An association between low vitamin B12 and low BMD was also reported [3, 7, 21]. Our study showed that Hcy, together with age, CTx and PTH, is the main predictor of BMD in both trochanter and total femur. Comparing all measured sites, vegetarians had a significantly lower TrFBMD and ToFBMD. Linear regression analysis confirmed the negative correlation between Hcy and FNBMD, TrFBMD and ToFBMD in vegetarians, but not in nonvegetarians. To our knowledge, there is a lack of data confined to the direct relation of Hcy and BMD in vegetarians. There is only one study on the relationship of vitamin B12 and BMD in adolescents formerly fed a macrobiotic diet [3]. In those probands, signs of an impaired cobalamin status, as judged by elevated concentrations of methylmalonic acid, were associated with low BMD.
It is not clear whether homocysteine influences the bone directly or if it only reflects the action of its cofounders like B vitamins. Herrmann et al. [11] found a strong accumulation of Hcy in bone tissue of hyperhomocysteinemic rats that was accompanied by significant bone loss and reduction of bone strength. This confirms the hypothesis that HHcy has direct detrimental effects on the bone. The majority of Hcy in bone tissue was bound to extracellular collagen. Hcy is known to disturb enzymatic collagen crosslinking by the inhibition of lysyl oxidase [26]. Blouin et al. [1] reported a significant correlation between plasma Hcy levels and collagen cross-links ratio in bone forming areas in elderly women. This was independent of the bone mineral content and/or bone mineral distribution pattern. Recently, Herrmann et al. [13] has found that increased Hcy concentrations stimulate human osteoclast activity in vitro, suggesting a mechanistic role of Hcy for bone resorption. Herrmann et al. also found moderate stimulation of primary human osteoblast activity by increasing concentrations of Hcy. However, the magnitude of this effect seems to be less pronounced than his observations on osteoclasts, suggesting an imbalance between osteoblasts and osteoclasts in favour of osteoclasts [12].
In summary, this study has shown that in our population of healthy Slovak women, Hcy is one of the predictors of BMD and HHcy is associated with bone loss. Additionally, HHcy is much higher in women on a vegetarian diet than in nonvegetarians. These results are consistent with increasing experimental evidence for an effect of Hcy on bone metabolism and confirm the hypothesis that Hcy plays a role not only in the pathogenesis of osteoporotic fractures but also in lower bone mineral density. Thus, because of HHcy, elderly women on a vegetarian diet seem to be at higher risk of low bone mineral density than nonvegetarian women.
References
Blouin S, Thaler HW, Korninger C, Schmid R, Hofstaetter JG, Zoehrer R, Phipps R, Klaushofer K, Roschger P, Paschalis EP (2009) Bone matrix quality and plasma homocysteine levels. Bone 44(5):959–964
Bozkurt N, Erdem M, Yilmaz E, Erdem A, Biri A, Kubatova A, Bozkurt M (2009) The relationship of homocysteine, B12 and folic acid with the bone mineral density of the femur and lumbar spine in Turkish postmenopausal women. Arch Gynecol Obstet 283(3):381–387
Dhonukshe-Rutten RA, van Dusseldorp M, Schneede J, de Groot LC, van Staveren WA (2005) Low bone mineral density and bone mineral content are associated with low cobalamin status in adolescents. Eur J Nutr 44(6):341–347
Elshorbagy AK, Gjesdal CG, Nurk E, Tell GS, Ueland PM, Nygard O, Tverdal A, Vollset SE, Smith AD, Refsum H (2009) Cysteine, homocysteine and bone mineral density: a role for body composition? Bone 44(5):954–958
Gerdhem P, Ivaska KK, Isaksson A, Petterson K, Väänänen HK, Obrant KJ, Åkesson K (2007) Association between homocysteine, bone turnover, BMD, mortality and fracture risk in elderly women. J Bone Min Res 22(1):127–134
Gjesdal CG, Vollset SE, Ueland PM, Refsum H, Meyer HE, Tell GS (2007) Plasma homocysteine, folate, and vitamin B12 and the risk of hip fracture: the Hordaland Homocysteine Study. J Bone Miner Res 22(5):747–756
Golbahar J, Hamidi A, Aminzadeh MA, Omrani GR (2004) Association of plasma folate, plasma homocysteine, but not methylenetetrahydrofolate reductase C667T polymorphism, with bone mineral density in postmenopausal Iranian women: a cross-sectional study. Bone 35:760–765
Grieco AJ (1977) Homocystinuria: pathogenic mechanisms. Am J Med Sci 273:120–132
Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver C (2000) Peak bone mass. Osteoporos Int 11(12):985–1009
Herrmann M, Kraenzlin M, Pape G, Sand-Hill M, Herrmann W (2005) Relationship between homocysteine and biochemical bone turnover markers and bone mineral density in peri- and post-menopausal women. Clin Chem Lab Med 43:1118–1123
Herrmann M, Tami A, Wildemann B, Wolny M, Wagner A, Schorr H, Taban-Shomal O, Umanskaya N, Ross S, Garcia P, Hübner U, Herrmann W (2008) Hyperhomocysteinemia induces a tissue specific accumulation of homocysteine in bone by collagen binding and adversely affects bone. Bone 44(3):467–475
Herrmann M, Widmann T, Colaianna G, Colucci S, Zallone A, Herrmann W (2005) Increased osteoclast activity in the presence of increased homocysteine concentrations. Clin Chem 51:2348–2353
Herrmann M, Umanskaya N, Wildemann B, Colaianni G, Widmann T, Zallone A, Herrmann W (2008) Stimulation of osteoblast activity by homocysteine. J Cell Mol Med 12(4):1205–1210
Herrmann M, Widmann T, Herrmann W (2005) Homocysteine—a newly recognised risk factor for osteoporosis. Clin Chem Lab Med 43(10):1111–1117
Houze P, Gamra S, Madelaine I, Bousquet B, Gourmel B (2001) Simultaneous determination of total plasma glutathione, homocysteine, cysteinylglycine, and methionine by high performance liquid chromatography with electrochemical detection. J Clin Lab Anal 15:144–153
Koebnick C, Garcia AL, Dagnelie PC, Strassner C, Lindemans J, Katz N, Leitzmann C, Hoffmann I (2005) Long-term consumption of a raw food diet is associated with favorable serum LDL cholesterol and triglycerides but also with elevated plasma homocysteine and low serum HDL cholesterol in humans. J Nutr 135(10):2372–2378
Leboff MS, Narweker R, Lacroix A, Wu L, Jackson R, Lee J, Bauer DC, Cauley J, Kooperberg C, Lewis C, Thomas AM, Cummings S (2009) Homocysteine levels and risk of hip fracture in postmenopausal women. J Clin Endocrinol Metab 94(4):1207–1213
Majchrzak D, Singer I, Männer M, Rust P, Genser D, Wagner KH, Elmadfa I (2006) B-vitamin status and concentrations of homocysteine in Austrian omnivores, vegetarians and vegans. Ann Nutr Metab 50(6):485–491
Maurer M, Burri S, de Marchi S, Hullin R, Martinelli M, Mohacsi P, Hess OM (2009) Plasma homocysteine and cardiovascular risk in heart failure with and without cardiorenal syndrome. Int J Cardiol (in press)
McLean RR, Jacques PF, Selhub J, Tucker KL, Samelson EJ, Broe KE, Hannan MT, Cupples LA, Kiel DP (2004) Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med 350:2042–2049
Morris MS, Jacques PF, Selhub J (2005) Relation between homocysteine and B-vitamin status indicators and bone mineral density in older Americans. Bone 37:234–242
Mudd SH, Skovby F, Levy HL, Pettigrew KD, Wilcken B, Pyeritz RE, Andria G, Boers GH, Bromberg IL, Cerone R (1985) The natural history of homocysteine due to the cystathionine beta synthase deficiency. Am J Hum Genet 37:1–31
Périer MA, Gineyts E, Munoz F, Sornay-Rendu E, Delmas PD (2007) Homocysteine and fracture risk in postmenopausal women: the OFELY study. Osteoporos Int 18:1329–1336
Refsum H, Smith AD, Ueland PM, Nexo E, Clarke R, McPartlin J, Johnston C, Engbaek F, Schneede J, McPartlin C, Scott JM (2004) Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem 50(1):3–32
Saito M (2006) Elevated plasma concentration of homocysteine, low level of vitamin B6, pyridoxal, and vitamin D insufficiency in patients with hip fracture: a possible explanation for detrimental cross-link pattern in bone collagen. Clin Calcium 16(12):1974–1984
Saito M, Fujii K, Marumo K (2006) Degree of mineralization-related collagen crosslinks in the femoral neck cancellous bone in cases of hip fracture and controls. Calcif Tissue Int 79:160–168
Selhub J, Jacques PF, Wilson PW, Rush D, Rosenberg IH (1993) Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA 270:2693–2698
Slavícek J, Kittnar O, Fraser GE, Medová E, Konecná J, Zizka R, Dohnalová A, Novák V (2009) Lifestyle decreases risk factors for cardiovascular diseases. Cent Eur J Public Health 16(4):161–164
Stanger O, Herrmann W, Pietrzik K, Fowler B, Geisel J, Dierkes J, Weger M (2003) DACH-LIGA Homocystein eV (German, Austrian and Swiss homocysteine society): consensus paper on the rational clinical use of homocysteine, folic acid and B-vitamins in cardiovascular and thrombotic diseases: guidelines and recommendations. Clin Chem Lab Med 41:1392–1403
Tucker KL, Qiao N, Scott T, Rosenberg I, Spiro A 3rd (2005) High homocysteine and low B vitamins predict cognitive decline in aging men: the Veterans Affairs Normative Aging Study. Am J Clin Nutr 82(3):627–635
Turner-McGrievy GM, Barnard ND, Scialli AR, Lanou AJ (2004) Effects of a low-fat vegan diet and a Step II diet on macro- and micronutrient intakes in overweight postmenopausal women. Nutrition 20(9):738–746
van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM, van der Klift M, de Jonge R, Lindemans J, de Groot LC, Hofman A, Witteman JC, van Leeuwen JP, Breteler MM, Lips P, Pols HA, Uitterlinden AG (2004) Homocysteine levels and the risk of osteoporotic fracture. N Engl J Med 350:2033–2041
Wolters M, Herrmann S, Hahn A (2003) B vitamin status and concentrations of homocysteine and methylmalonic acid in elderly German women. Am J Clin Nutr 78:765–772
Acknowledgments
We would like to thank Mr. Daniel Lichtenberger for careful reading of the manuscript and helpful comments. This work was supported by Research and Development Support Agency under the contract No: APVT-21-010104 and APVT-21-017704.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krivošíková, Z., Krajčovičová-Kudláčková, M., Spustová, V. et al. The association between high plasma homocysteine levels and lower bone mineral density in Slovak women: the impact of vegetarian diet. Eur J Nutr 49, 147–153 (2010). https://doi.org/10.1007/s00394-009-0059-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-009-0059-1