Abstract
Background
Geographical differences may impact the treatment of heart failure (HF) and the results of clinical trials. We have investigated the differences between geographical areas across Europe in the BIOSTAT-CHF program.
Methods
Patients with worsening HF enrolled in BIOSTAT-CHF were subdivided, according to the European geographical areas, into those from Northern countries (The Netherlands, Norway, Sweden, UK), Central countries (Germany, Poland, Serbia, Slovenia), and Mediterranean countries (France, Greece, Italy). Patients were compared for baseline characteristics, treatment, and outcomes. The primary endpoint was a composite of all-cause mortality or HF hospitalization.
Results
Among 2516 patients enrolled in BIOSTAT-CHF, 814 (32.3%) were from Northern European centers, 816 (32.4%) from Central European centers, and 886 (35.2%) from Mediterranean centers. Patients from Northern European centers were older, had more severe signs and symptoms of HF, and with lower incidence of non-cardiac comorbidities such as chronic kidney dysfunction, diabetes and, hypertension, compared to those from the Central and Mediterranean centers. Patients receiving ≥ 50% of the target dose of both ACE-I/ARB after the up-titration phase were higher in the Northern European centers compared with the other regions (60% versus 58.7% in the Central European centers and 46.5% in the Mediterranean ones; p < 0.001). The primary endpoint occurred at a higher rate in the Northern centers (44.3% versus 37.4% in central centers and 39.6% in Mediterranean centers; p = 0.014), this difference became non-significant after the adjustment for important confounders. Importantly, treatment up-titration reduced the event rates regardless of the geographical region (p for interaction > 0.05).
Conclusion
The BIOSTAT-CHF study showed significant differences in the clinical features, treatment and prognosis in European patients with HF. Patients from the Mediterranean centers less often had the HF treatments up-titrated; however, the treatment up-titration benefited patients irrespective of their geographical region and should be part of the “default” clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is prevalent worldwide and its incidence is increasing due to the aging of the population and the efficacy of treatment of acute cardiovascular diseases [1,2,3,4]. However, the patients’ characteristics, HF treatments, and prognosis may differ with the geographical region and these geographical differences may affect the way each individual patient is treated and also limit the generalizability of the research results [5,6,7,8,9]. These differences may be important even within one single continent, such as in the case of the European countries [10,11,12]. This was first shown in the retrospective analyses of randomized trials and then in registries [13,14,15]. The European Society of Cardiology’s (ESC) HF pilot survey showed differences across European geographical areas [15]. Patients from Eastern European countries were younger, with a more frequent ischemic etiology and had higher systolic blood pressure. Patients in Northern countries had a lower left ventricular ejection fraction (EF). Devices were under-used in Eastern countries [15]. In the more recent ESC-HF Long-term registry, patients from middle Eastern and Northern European countries were older and more likely to have an ischemic etiology. The use of implantable cardioverter defibrillators (ICDs) or cardiac resynchronization therapy with defibrillation (CRT-D) was also different across European areas. Geographical areas were independently related with the outcomes of chronic heart failure patients at multivariable analysis, with a lower risk of events in Northern European versus Southern European countries [16].
The biological study of tailored treatment in chronic HF (BIOSTAT-CHF) is a European (11 European countries) multicenter (most patients were enrolled and followed by tertiary referral centers), prospective study, which included patients with worsening signs and/or symptoms of HF who were considered to be on sub-optimal medical treatment [17]. Therefore, this study allows the assessment of geographical differences between different areas of Europe in patients whose treatment was not optimal, but the study protocol recommended treatment optimization. Consequently, observing eventual patterns and differences in HF treatment optimization may help in developing strategies for the improvement of HF treatment across Europe.
The aim of this secondary, non-prespecified analysis is to investigate the geographic differences in the clinical characteristics, prognosis, and treatment up-titration in the BIOSTAT-CHF study.
Methods
The design and main results of the study is described in detail elsewhere [18, 19]. The primary inclusion criteria were defined by either a left ventricular ejection fraction (LVEF) < 40% or plasma concentrations of BNP and/or N-terminal pro-brain natriuretic peptide (NT-proBNP) > 400 ng/ml or > 2000 ng/ml and treated with at least 40 mg of diuretics. Patients were enrolled from 11 European countries and had to be treated with sub-optimal dose of angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers. Of the 2516 patients included in the index cohort, 2281 (91%) have a left ventricular ejection fraction ≤ 40% while only 235 (10%) patients have ventricular ejection fraction greater than 40%. Patients had to be not previously treated with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor antagonists (ARBs) and beta-blockers or should have been receiving ≤ 50% of their target doses according to the current guidelines [1]. Patients hospitalized for acute HF and outpatients with of signs and symptoms of HF could be included in the study. The outpatients included in the study were 822 (33%) while inpatients were 1694 (67%) (Table 1). The primary endpoint was time to a composite of all-cause death and heart failure hospitalization. The trial was approved by the ethics committee at each study center. All the patients provided written informed consent. The study design included a 3-month up-titration phase, during which the investigators had to introduce and/or up-titrate guideline-recommended medications with special attention to ACE-inhibitors, ARBs, beta-blockers and mineralocorticoid receptor antagonists (MRA). The NT-pro BNP values were measured using the Proseek Multiplex CVDII panel (Olink Proteomics AB, Uppsala, Sweden) and presented in normalized protein expression (NPX) values, which is an arbitrary unit on a log2 scale in which a high value corresponds to a higher protein expression [20].
For the purpose of this analysis, the study patients of BIOSTAT-CHF were subdivided according to their country of origin’s geographical area. Northern countries included The Netherlands, Norway, Sweden, and UK; Central countries included Germany, Poland, Serbia, and Slovenia; Mediterranean countries included France, Greece, and Italy. All countries were classified by the World Bank as belonging to the high-income economies with the exception of Serbia which is included (by the World Bank) among the upper-middle-income economies [21]. Each country contributed with a different number of centers: The Netherlands 12, France 12, Germany 1, Serbia 8, Slovenia 3, Greece 11, Italy 8, Sweden 4, Norway 5, Poland 5, and Scotland (UK) 6. The recruitment centers were mainly general cardiology at some tertiary centers [17].
Statistical analysis
Continuous variables are shown as mean ± standard deviation, dichotomous variables as number (%). Comparisons of the demographic and clinical baseline characteristics, medical history, and medications were done by ANOVA for continuous variables and the two test for categorical variables. Categorical variables are expressed as frequencies and proportions (%). Individual country contributing to the enrollment and treatment according to the geographical area are expressed as frequencies and proportions (%). Kaplan–Meier plots were generated for each area to evaluate clinical outcomes. A p value < 0.05 was used to indicate statistical significance. The outcomes of interest are time to a composite of death or unscheduled hospitalizations for heart failure, HF hospitalization, and all-cause mortality. Cox proportional hazard regression models were used to model long-term event rates, both in univariable and multivariable analyses. A validated multivariable risk model was used to predict all-cause mortality and hospitalizations and assess the independent prognostic value of geographical areas [20]. Cox model’s proportional hazard assumptions have been verified and no violations found. Statistical analysis was performed with Stata ®software 14.2 (Release 14, 2015, StataCorp LP, College Station, TX).
Results
Patients were enrolled from December 2010 to 15 December 2012. The end of study follow-up was on 1 April 2015. A total of 2516 patients were enrolled in the BIOSTAT-CHF study with a median follow-up of 21 months (interquartile range: 15–27 months).
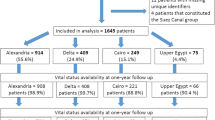
The distribution according to the geographic region was as follows: 814 (32.3%) in Northern centers, 816 (32.4%) in Central centers, and 886 (35.2%) in Mediterranean centers. Results regarding the baseline characteristics of the patients subdivided according to the European area are shown in Table 1 and individual country’s contribution to enrollment in the study is represented in supplementary Fig. 1. Data about the enrollment contribution and baseline characteristics for each individual country are listed in supplementary Table 1.
Baseline characteristics
The patients from northern European centers were more hospitalized and with a higher percentage of LVEF > 40% (Table 1). Patients from Northern European centers were also much older, more often female, had a higher heart beat rate (88.3 ± 24.7 beats per minute in Northern area vs 79.6 ± 19.5in Central area and 79.3 ± 18.4 in the Mediterranean area; p < 0.001), more severe signs and symptoms of HF and higher NT-pro BNP values (log-NT-pro BNP3.40 ± 1.34 NPX in the Northern area vs 2.79 ± 1.39 NPX in the Central area vs 2.89 ± 1.36 NPX in the Mediterranean area; p < 0.001). History of diabetes and high blood pressure were lower in Northern European centers (diabetes: Northern centers 26.5%, Central centers 24.3%, Mediterranean centers 36.5%, p < 0.001; high blood pressure: Northern countries 50.4%, Central countries 75.4%, Mediterranean countries 61.4%, p < 0.001). The presence of atrial fibrillation and chronic obstructive pulmonary diseases has been more frequent in patients from northern European centers (atrial fibrillation: Northern centers 47.5%, Central centers 41.8%, Mediterranean centers 46.8%, p < 0.038; COPD: Northern centers 19.0%, Central centers 14.0%, Mediterranean centers 18.8%, p < 0.009). Arterial hypertension and valvular disease were more often the cause of heart failure in patients form Northern European centers compared with the others areas of origin (hypertension: Northern Countries 9.7%, Central centers 10.9%, Mediterranean centers 9.7%; valvular disease: Northern centers 8.8%, Central centers 7.7%, Mediterranean centers 6.2%). Instead, the ischemic etiology of heart failure was less frequent in the Northern European centers (Northern centers 38.9%, Central centers 46.7%, Mediterranean centers 45.7%). With regard to the biochemical profile, the baseline glomerular filtration rate was lower in Northern area patients compared to the others (eGFR, ml/min/1.73m2: Northern centers 58.9 ± 23.0, Central centers 66.3 ± 22.4, and Mediterranean centers 62.2 ± 23.6, p < 0.001), as well as sodium plasma levels (sodium, mmol/l: Northern centers 138.9 ± 4.0, Central centers 139.8 ± 3.8, and Mediterranean centers, 138.8 ± 4.1, p < 0.001), and potassium levels (Northern centers 4.2 ± 0.5, Central centers 4.4 ± 0.6, and Mediterranean centers, 4.2 ± 0.6, p < 0.001).
The use of implantable devices was most common in the Mediterranean centers, as well as a previous history of coronary revascularization with percutaneous coronary angioplasty (PCI) or coronary artery bypass (BPAC).
Figure 2a, b represents the country-by-country distribution of signs of congestion. Patients from the Northern European centers tended to have a higher prevalence of pulmonary congestion, peripheral edema and elevated jugular venous pressure compared with Central and Mediterranean centers.
Treatment
The data regarding treatments are shown in Table 1 and Supplementary Fig. 2 and refer to the end of the 3-month up-titration period. The prescription of guideline-recommended therapies varied across the groups. Patients from Central European centers received more ACE-inhibitors or ARBs compared to those from Northern European and Mediterranean centers (78.4% versus 73.3% and 63.6%, respectively). Beta-blockers and MRA were administered more often in central Europe compared with the other countries (87.5% versus 81.3% and 80% for beta-blockers and 66.5% versus 42.6% and 50.7% for MRA in the Northern European and Mediterranean centers, respectively).
Digoxin was frequently prescribed in Central Europe (23.5%) and was less used in Mediterranean patients (14.6%). Loop diuretics were prescribed, as required in the protocol, in almost all patients, with slightly lower, but statistically significant (p = 0.026) rates in the Mediterranean centers (99.1% versus 99.5% and 100% in the Northern and Central centers, respectively).
Notably, the proportion of patients receiving ≥ 50% of the target dose of both ACE-I/ARB after the up-titration phase was higher in the Northern European centers compared with the other regions (60%, versus 58.7% in the Central centers and 46.5% in the Mediterranean ones; p 0.001). Similarly, achievement of ≥ 50% of the target doses of beta-blockers was greater in patients in the Northern European centers than in the Central and Mediterranean ones (46.6%, 32.5%, 31.2%, respectively, p < 0.001).
Outcomes and interaction with treatment
The incidence of the endpoints is shown in Table 1. Patients from the Northern centers had higher numerical rate of the primary endpoint of the study of all-cause mortality and HF hospitalization (44.3% in the Northern centers versus 37.4% in the Central centers and 39.6% in the Mediterranean centers; p = 0.014). A similar result was found for all-cause mortality alone (29.2%, 24.1% and 25.1% in the Northern, Central and Mediterranean centers, respectively; p = 0.043) and HF hospitalizations alone (27.1%, 21.0% and 24.5% in the Northern, Central and Mediterranean centers, respectively; p = 0.014). During the up-titration period, the patients from Northern European centers had a significant increase in all-cause mortality compared with other regions (Northern centers 8.2%, Central centers 5.3%, Mediterranean centers 4.6%, p 0.004). Figure 2a, b represents the country-by-country distribution of outcomes.
Unadjusted and adjusted outcome analyses for the primary and secondary endpoints are shown in (Table 2). After adjustment for other predictors of the outcome, there were no significant differences between the geographical areas in terms of relative risk of clinical outcomes. Differences in the outcomes were evaluated by the Log-rank test and are shown in the Kaplan–Meier curves (Fig. 1).
Treatment up-titration
Reaching to at least 50% of the recommended dose of beta-blockers and ACEi/ARBs was associated with a reduced primary outcome (death or HF hospitalization) event rate: HR (95%CI) = 0.82 (0.72–0.94); p = 0.003. Without treatment by region interaction; p for interaction = 0.058. Supplementary Table 2.
Discussion
This analysis of BIOSTAT-CHF shows that there are marked differences in patient characteristics and HF treatment in different geographical areas in Europe. Patients from Northern European centers were older, more often female and had a higher heart rate, more severe signs and symptoms of HF and higher NT-proBNP values. Patients from Central European centers were younger, had a higher prevalence of hypertension and were more likely to receive ACE-inhibitors/ARBs, beta-blockers and MRAs at baseline. Mediterranean patients were more likely to be diabetics and had a greater history of PCA or CABG. A device implantation was more likely in these patients. In general, patients from Northern European centers seem to have a greater severity of heart failure but the adjusted event rates were similar across regions. Importantly, treatment up-titration benefited all patients regardless of their region of origin.
A previous analysis of BIOSTAT-CHF study, reaching less than 50% of the recommended doses of ACE-inhibitors/ARBs and beta-blockers was associated with a greater risk of death and/or heart failure hospitalization [22]. The authors also demonstrated that achieving ≥ 50% of the target doses of these drugs predicted better outcomes and this association persisted after adjustment for baseline variables. These data were recently confirmed in the QUALIFY international registry where the prescription of at least 50% of recommended dosages of ACEIs, ARBs, BBs, MRAs and ivabradine was associated with better outcomes [23]. In our analysis, patients from Northern European centers have reached higher doses of ACE-inhibitors/ARBs and beta-blockers compared with the other regions. Patients from this region were also more hospitalized at the time to inclusion in the BIOST-CHF study and showed higher mortality rates in univariate analysis during the titration period compared with the Central and Mediterranean patients (Table 1). Although patients from Northern Europe were the oldest, the presence of common co-morbidities usually related with age such as diabetes, arterial hypertension and chronic kidney disease were lower than in the Central Europe and in the Mediterranean areas. These data are also consistent with the Heart Failure Long-Term Registry (ESC-HF-LT) in which the proportion of patients with diabetes and hypertension in both acute and chronic HF were higher in Northern Europe compared with the other European countries [15].
In general, our results confirm previous studies showing significant differences in the characteristics, outcomes and medical treatment of patients with HF from different geographical areas [5,6,7,8,9,10,11,12,13,14]. In particular, it has also been demonstrated that there are substantial variations in the use of guideline-recommended medications in patients of the same geographical area [24]. Many factors may account for these differences within one continent and may include climate, socioeconomic conditions, income, health system organization [25,26,27]. Data from the CHAMP-HF (change the management of patients with heart failure) registry showed that sex (women), race (blacks and Hispanics) and lower socioeconomic status are associated with worse quality of life, functional and socioeconomic status and more severe symptoms [28]. Despite the differences among the 11 European countries in national health systems, economy and quality of life, we did not find significant differences in the outcomes of patients included in the BIOSTAT-CHF study.
Non-pharmacological treatment of HF also differed across the regions. Patients from the Northern European centers were less likely to receive ICD and CRT-D devices while Central European centers had less coronary revascularization despite the higher incidence of coronary artery disease. Data from the BIOSTAT-CHF study show that coronary revascularization (percutaneous or surgical) and device implantation were greater in the Mediterranean European centers. These data are consistent with epidemiological studies [29, 30]. In particular, the number of implantable electronic defibrillators was higher in the Southern than the Northern region with, respectively, 135 and 100 implants per million inhabitants [31]. The presence of an old healthcare organizational structure and less control of health expenditure could explain the greater use of revascularization and device therapy in the centers of Southern Europe compared to the Central and Northern Europe. The control of the accuracy of health expenditure is a priority in some countries like Italy [32]. Socioeconomic factors are well-known determinants of the use of devices and may also have had a major role in our patients [33].
National income is another determinant of the quality of health care offered by a nation [34]. Indeed, high-income European countries provide citizens a better quality of care especially for what concerns disease-management specific programs as well as integrated prevention initiatives often realized with the help of dedicated medical and nurse-led programs [35]. The prospective urban rural epidemiologic (PURE) study has shown that the rates of major cardiovascular disease and death were higher in low-income countries than in high-income countries despite having a higher burden of cardiovascular risk factors [36]. The PURE study evaluated 628 urban and rural communities in 17 countries from Asia, Africa, North and South America and Europe.
Our results show the same event rates in patients coming from different countries, independent of their incomes. This may be caused by lower differences in the healthcare systems, when related to tertiary care centers, such as those involved in BIOSTAT-CHF, compared to a worldwide study such as PURE. Recently the income inequality was associated with poor outcomes in patients with HF, with an impact similar to those of major comorbidities [37]. In this study, 15,216 participants from 54 countries worldwide were enrolled in the two largest trials including patients with HF, namely reduced LVEF: PARADIGM-HF trial(Prospective comparison of ARNI [angiotensin receptor neprilysin inhibitor] with ACEI [angiotensin-converting enzyme inhibitor] to determine the impact on global mortality and morbidity in heart failure) and the ATMOSPHERE trial (aliskiren trial to minimize outcome in patients with heart failure). Income should, however, be considered as a potential novel variable on HF outcomes in the context of international mega trials [12, 38].
In our study, variables related to HF severity were the only determinants of outcomes at multivariable analysis. Medical treatment, despite significant geographical differences, had no independent role.
Limitations
One major limitation is the representativeness of our patients. BIOSTAT-CHF involved only 11 countries, so most of the European countries were not included. More importantly, only a few centers were included from each country and these were mainly tertiary care centers. Germany has contributed with only one center. The value of this analysis is more in showing how differences in clinical characteristics and medical prescriptions can lose their impact on outcomes once the treatment is optimized in all the patients. This is also a selected cohort of patients randomized in a clinical trial.
The subdivision of countries was based on geographical criteria. However, this may not reflect real differences between different areas. For instance, the Mediterranean area was slightly penalized as it was represented only by two countries (Italy and Greece) with a strong Mediterranean vocation and by France, which has many social and economic aspects more closely related to the European Central countries. Differences in the health care systems, delivery of care and incomes are present between different geographical areas and they were likely the main determinants of our results. However, unfortunately these variables were not collected in the BIOSTAT-CHF study. Dietary aspects, such as salt content, may also have had a role [26]. Furthermore, Serbia is the only country to be classified by the World Bank as upper-middle-income economy, whereas all the other countries (n = 10) are classified as high-income economies [21].
However, all the countries in this study were broadly distributed across the European territories and well represented each macro area. However, some sites have contributed to the enrollment of a preponderant portion of patients for their respective country, and therefore a “single-center” driven effect cannot be excluded (supplementary Table 1).
Conclusion
The BIOSTAT-CHF study showed significant differences in clinical features, treatment and prognosis in European patients with HF. Patients from the Mediterranean Countries less often had HF treatments up-titrated; however, treatment up-titration benefited patients irrespective of their geographical region and should be part of the “default” clinical practice.
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force M, and Document R (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18:891–975
Schmidt M, Ulrichsen SP, Pedersen L, Botker HE, Sorensen HT (2016) Thirty-year trends in heart failure hospitalization and mortality rates and the prognostic impact of co-morbidity: a Danish nationwide cohort study. Eur J Heart Fail 18:490–499
Omersa D, Farkas J, Erzen I, Lainscak M (2016) National trends in heart failure hospitalization rates in Slovenia 2004–2012. Eur J Heart Fail 18:1321–1328
Metra M, Teerlink JR (2017) Heart failure. Lancet 28:1981–1995
Massie BM, Cleland JG, Armstrong PW, Horowitz JD, Packer M, Poole-Wilson PA, Ryden L (1998) Regional differences in the characteristics and treatment of patients participating in an international heart failure trial. The Assessment of Treatment with Lisinopril and Survival (ATLAS) Trial Investigators. J Cardiac Fail 4:3–8
Blair JE, Zannad F, Konstam MA, Cook T, Traver B, Burnett JC Jr, Grinfeld L, Krasa H, Maggioni AP, Orlandi C, Swedberg K, Udelson JE, Zimmer C, Gheorghiade M, Investigators E (2008) Continental differences in clinical characteristics, management, and outcomes in patients hospitalized with worsening heart failure results from the EVEREST (Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study with Tolvaptan) program. J Am Coll Cardiol 52:1640–1648
O'Connor CM, Fiuzat M, Swedberg K, Caron M, Koch B, Carson PE, Gattis-Stough W, Davis GW, Bristow MR (2011) Influence of global region on outcomes in heart failure beta-blocker trials. J Am Coll Cardiol 58:915–922
Metra M, Ponikowski P, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Hua TA, Severin T, Unemori E, Voors AA, Teerlink JR (2013) Effects of serelaxin in subgroups of patients with acute heart failure: results from RELAX-AHF. Eur Heart J 34:3128–3136
Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Heitner JF, Lewis EF, O'Meara E, Rouleau JL, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, McKinlay SM, Pitt B (2015) Regional variation in patients and outcomes in the treatment of preserved cardiac function heart failure with an aldosterone antagonist (TOPCAT) trial. Circulation 131:34–42
Metra M, Mentz RJ, Hernandez AF, Heizer GM, Armstrong PW, Clausell N, Corbalan R, Costanzo MR, Dickstein K, Dunlap ME, Ezekowitz JA, Howlett JG, Komajda M, Krum H, Lombardi C, Fonarow GC, McMurray JJ, Nieminen MS, Swedberg K, Voors AA, Starling RC, Teerlink JR, O'Connor CM (2016) Geographic differences in patients in a global acute heart failure clinical trial (from the ASCEND-HF trial). Am J Cardiol 117:1771–1778
Kristensen SL, Martinez F, Jhund PS, Arango JL, Belohlavek J, Boytsov S, Cabrera W, Gomez E, Hagege AA, Huang J, Kiatchoosakun S, Kim KS, Mendoza I, Senni M, Squire IB, Vinereanu D, Wong RC, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, Packer M, McMurray JJ (2016) Geographic variations in the PARADIGM-HF heart failure trial. Eur Heart J 37:3167–3174
Dokainish H, Teo K, Zhu J, Roy A, AlHabib KF, ElSayed A, Palileo-Villaneuva L, Lopez-Jaramillo P, Karaye K, Yusoff K, Orlandini A, Sliwa K, Mondo C, Lanas F, Prabhakaran D, Badr A, Elmaghawry M, Damasceno A, Tibazarwa K, Belley-Cote E, Balasubramanian K, Islam S, Yacoub MH, Huffman MD, Harkness K, Grinvalds A, McKelvie R, Bangdiwala SI, Yusuf S, Investigators I-C (2017) Global mortality variations in patients with heart failure: results from the international congestive heart failure (INTER-CHF) prospective cohort study. Lancet Glob Health. 5:e665–e672
van Veldhuisen DJ, Charlesworth A, Crijns HJ, Lie KI, Hampton JR (1999) Differences in drug treatment of chronic heart failure between European countries. Eur Heart J 20:666–672
Maggioni AP, Dahlstrom U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, Fruhwald F, Gullestad L, Logeart D, Fabbri G, Urso R, Metra M, Parissis J, Persson H, Ponikowski P, Rauchhaus M, Voors AA, Nielsen OW, Zannad F, Tavazzi L, Heart Failure Association of the European Society of C (2013) EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail 15:808–817
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, Ferrari R, Piepoli MF, Delgado Jimenez JF, Metra M, Fonseca C, Hradec J, Amir O, Logeart D, Dahlstrom U, Merkely B, Drozdz J, Goncalvesova E, Hassanein M, Chioncel O, Lainscak M, Seferovic PM, Tousoulis D, Kavoliuniene A, Fruhwald F, Fazlibegovic E, Temizhan A, Gatzov P, Erglis A, Laroche C, Mebazaa A, Heart Failure Association of the European Society of C (2016) European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail 18:613–625
Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo-Leiro MG, Laroche C, Seferovic PM, Anker SD, Ferrari R, Ruschitzka F, Lopez-Fernandez S, Miani D, Filippatos G, Maggioni AP, Investigators ESCHFL-TR (2017) Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC Heart Failure Long-Term Registry. Eur J Heart Fail 19:1242–1254
Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, van der Harst P, Hillege HL, Lang CC, Ter Maaten JM, Ng L, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zannad F, Zwinderman AH, Metra M (2016) A systems biology study to tailored treatment in chronic heart failure: rationale, design, and baseline characteristics of BIOSTAT-CHF. Eur J Heart Fail 18:716–726
Ferreira JP, Rossignol P, Machu JL, Sharma A, Girerd N, Anker SD, Cleland JG, Dickstein K, Filippatos G, Hillege HL, Lang CC, Ter Maaten JM, Metra M, Ng L, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zwinderman AH, Voors A, Zannad F (2017) Mineralocorticoid receptor antagonist pattern of use in heart failure with reduced ejection fraction: findings from BIOSTAT-CHF. Eur J Heart Fail. 19(10):1284–1293
Voors AA, Ouwerkerk W, Zannad F, van Veldhuisen DJ, Samani NJ, Ponikowski P, Ng LL, Metra M, Ter Maaten JM, Lang CC, Hillege HL, van der Harst P, Filippatos G, Dickstein K, Cleland JG, Anker SD, Zwinderman AH (2017) Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur J Heart Fail. 19(5):627–634
Assarsson E, Lundberg M, Holmquist G, Björkesten J, Thorsen SB, Ekman D, Eriksson A, Rennel Dickens E, Ohlsson S, Edfeldt G, Andersson AC, Lindstedt P, Stenvang J, Gullberg M, Fredriksson S (2014) Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE 9(4):e95192
https://data.worldbank.org/about/country-and-lending-groups. Accessed Oct 2019
Ouwerkerk W, Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, van der Harst P, Hillege HL, Lang CC, Ter Maaten JM, Ng LL, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zannad F, Metra M, Zwinderman AH (2017) Determinants and clinical outcome of uptitration of ACE-inhibitors and beta-blockers in patients with heart failure: a prospective European study. Eur Heart J 38:1883–1890
Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS, QUALIFY Investigators (2017) Physicians' guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail. 19(11):1414–1423
Peterson PN, Chan PS, Spertus JA, Tang F, Jones PG, Ezekowitz JA, Allen LA, Masoudi FA, Maddox TM (2013) Practice-level variation in use of recommended medications among outpatients with heart failure: Insights from the NCDR PINNACLE program. Circ Heart Fail. 6(6):1132–1138
Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, Mieres JH, Ferdinand KC, Mensah GA, Sperling LS (2018) Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation 137(20):2166–2178
Callender T, Woodward M, Roth G, Farzadfar F, Lemarie JC, Gicquel S, Atherton J, Rahimzadeh S, Ghaziani M, Shaikh M, Bennett D, Patel A, Lam CS, Sliwa K, Barretto A, Siswanto BB, Diaz A, Herpin D, Krum H, Eliasz T, Forbes A, Kiszely A, Khosla R, Petrinic T, Praveen D, Shrivastava R, Xin D, MacMahon S, McMurray J, Rahimi K (2014) Heart failure care in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 11(8):e10016
Kondo N, Sembajwe G, Kawachi I, van Dam RM, Subramanian SV, Yamagata Z (2009) Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ 10(339):b4471
Khariton Y, Nassif ME, Thomas L et al (2018) Health status disparities by sex, race/ethnicity, and socioeconomic status in outpatients with heart failure. JACC Heart Fail. 6(6):465–473
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M (2016) Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 37(42):3232–3245
Finegold JA, Asaria P, Francis DP (2013) Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int J Cardiol. 168(2):934–945
Raatikainen MJP, Arnar DO, Merkely B, Nielsen JC, Hindricks G, Heidbuchel H, Camm J (2017) A decade of information on the use of cardiac implantable electronic devices and interventional electrophysiological procedures in the European Society of Cardiology Countries: 2017 report from the European Heart Rhythm Association. Europace. 19(1):ii1–ii90
Ghislandi S, Krulichova I, Garattini L (2005) Pharmaceutical policy in Italy: towards a structural change? Health Policy 72:53–63
Lund LH, Braunschweig F, Benson L, Stahlberg M, Dahlstrom U, Linde C (2017) Association between demographic, organizational, clinical, and socio-economic characteristics and underutilization of cardiac resynchronization therapy: results from the Swedish Heart Failure Registry. Eur J Heart Fail 19:1270–1279
Ferreira JP, Rossignol P, Dewan P, Lamiral Z, White WB, Pitt B, McMurray JJV, Zannad F (2019) Income level and inequality as complement to geographical differences in cardiovascular trials. Am Heart J. 1(218):66–74
Devaux M (2015) Income-related inequalities and inequities in health care services utilisation in 18 selected OECD countries. Eur J Health Econ. 16:21–33
Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, Yu L, Zhang S, Mony P, Swaminathan S, Mohan V, Gupta R, Kumar R, Vijayakumar K, Lear S, Anand S, Wielgosz A, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Yusoff K, Ismail N, Iqbal R, Rahman O, Rosengren A, Yusufali A, Kelishadi R, Kruger A, Puoane T, Szuba A, Chifamba J, Oguz A, McQueen M, McKee M, Dagenais G, Investigators P (2014) Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 371:818–827
Dewan P, Rørth R, Jhund PS, Ferreira JP, Zannad F, Shen L, Køber L, Abraham WT, Desai AS, Dickstein K, Packer M, Rouleau JL, Solomon SD, Swedberg K, Zile MR, McMurray JJ, ATMOSPHERE Investigators (2019) Income inequality and outcomes in heart failure: a global between-country analysis. JACC Heart Fail. 7:336–346
Maggioni AP (2017) Uncovering difference: a glimpse at patients with heart failure in low-income and middle-income countries. Lancet Glob Health. 5(7):e634–e635
Funding
BIOSTAT-CHF was funded by a grant from the European Commission: FP7-242209-BIOSTAT-CHF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interest with this post-hoc analysis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lombardi, C.M., Ferreira, J.P., Carubelli, V. et al. Geographical differences in heart failure characteristics and treatment across Europe: results from the BIOSTAT-CHF study. Clin Res Cardiol 109, 967–977 (2020). https://doi.org/10.1007/s00392-019-01588-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01588-7