Abstract
Background
The presence of left bundle branch block (LBBB) represents a particular challenge in properly measuring the QT interval. Here we demonstrate the applicability of the “Bogossian formula” in pacemaker patients with LBBB due to apical or nonapical right ventricular (RV) pacing and preserved left ventricular function.
Methods
A total of 163 patients with a cardiac one- or two-chamber pacemaker were included in this prospective, multicentre observational study. Twelve-lead ECG recordings were obtained during both intrinsic rhythm and RV pacing with induced LBBB. The QT interval measured during LBBB was corrected using the Bogossian formula to obtain the “modified QT” (QTm). The QTmc interval was calculated with the Bazett formula, and this was compared with the QTc interval during intrinsic rhythm.
Results
Eighty-three patients (78 ± 9 years; male n = 83) with apical and eighty patients (71 ± 13 years; male n = 80) with non-apical RV pacing were included in this study. In the apical group the QTmc was determined to be 444 ± 39 ms in paced rhythm and the QTc interval 413 ± 36 ms in intrinsic rhythm. In the non-apical group these values were 430 ± 34 ms in paced and 416 ± 32 ms in intrinsic rhythm.
Conclusion
The Bogossian formula is a reliable tool for QTc interval evaluation in pacemaker patients with LBBB due to apical or non-apical RV pacing. However, an overestimation of 30 ms should be included in the calculation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Evaluation of the QTc interval by a 12-lead electrocardiogram is an important and readily available diagnostic screening tool used to identify patients of any age at increased risk for ventricular tachycardia and consequently sudden cardiac death. In addition to being linked to the congenital channelopathies (e.g. primary long QT syndrome), a prolonged QT interval can be secondarily associated with the intake of specific drugs, bradycardia, or hypokalemia [1]. Prolongation of the QT interval is also observed in the presence of bundle branch block. In particular, the left bundle branch block (LBBB) is a common conduction disorder in patients with structural heart disease that is known to be an independent risk factor for all-cause mortality [2, 3]. About 11% of all patients with LBBB show no signs of structural heart disease [2]. In order to more easily identify patients at high risk for ventricular arrhythmias with LBBB due to true prolonged QT duration, the Bogossian formula was recently introduced (Fig. 1) [3]. This formula (QT = QTLBBB − 50% × QRSLBBB) was derived by comparing intrinsic QT intervals of patients with narrow QRS with a QT interval in the same patient collective after right ventricular (RV) pacing and induction of a LBBB in the course of an invasive electrophysiological examination [3]. The Bogossian formula was also evaluated in patients with intermittent intrinsic LBBB and in patients who presented initially with a narrow QRS who developed LBBB after transcatheter aortic valve implantation. The formula performed well in these various clinical scenarios [4]. Furthermore, the formula has recently been evaluated in patients with structural heart disease and an implanted cardioverter defibrillator (ICD) [5]. In this specific cohort the formula also proved to be a reliable tool; however, a slight overestimation of the QT interval was inherent and should be noted.
The formula has never been evaluated in a pacemaker patient collective, which usually includes patients with preserved left ventricular function [5, 6]. Functional LBBB due to right ventricular apical- or non-apical pacing is a common finding in pacemaker recipients. Until now, to accurately quantify the QT interval in this patient cohort, it has been necessary to measure the QT interval during intrinsic ventricular rhythm. This requires, first of all, that the investigator has expertise in programming pacemaker devices and that a programmer of the specific pacemaker manufacturer is at hand. Secondly, the patient must have an intrinsic ventricular rhythm of ≥ 30 beats per minute (bpm). Application of the Bogossian formula in this patient collective would help to simplify the measurement of the correct QT interval and to make it easier for non-electrophysiologists.
Methods
Study patients and ECG analysis
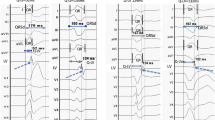
The study conforms to the guiding principles of the Declaration of Helsinki and was approved by the local ethics committees of the various centres. All patients gave informed consent for participation. Consecutive patients with a transvenous pacemaker with an apical or non-apical RV lead who presented with an intrinsic narrow QRS with a duration of less than 120 ms and a heart rate > 30/min were included in this prospective observational study. All parameters were acquired during routine pacemaker follow-up. In all patients, QRS duration, the intrinsic JT (JTi) interval, and the intrinsic QT (QTi) interval were measured in the presence of an intrinsic narrow QRS with VVI 30/min backup stimulation of the pacemaker system. Next, patients underwent RV pacing during the course of RV pacing threshold testing, thereby causing a functional LBBB (Figs. 2, 3), and the same ECG parameters as those measured in intrinsic rhythm were assessed again. The pacing rate during threshold testing was up to 40 bpm above the intrinsic heart rate. The QT interval was always measured in the lead presenting the longest interval, usually V2 or V3, in line with current recommendations [7]. A tangent was applied to the T wave for accurate determination of the QT interval [8]. In all patients, ECG parameters were assessed individually by two independent operators (one experienced electrophysiologist and one trainee) to additionally analyse any potential effects of the level of experience.
Finally, measured values were compared with the corrected QT interval employing the simplified Bogossian formula (QT = QTLBBB– 50% × QRSLBBB). A deviation of less than 10% of intrinsic QT duration was considered to be acceptable. To exclude potential effects of the heart rate, the Bazett formula was applied before and after employment of the new formula in all patients.
Statistical analysis
Continuous data are displayed as mean ± standard deviation. Data were analysed by employing a computerized database (Microsoft Excel 2010, Microsoft, Redmond, WA, USA) and were statistically evaluated using SPSS Software Release 23.0.0. The Shapiro–Wilk test was employed to assess normal distribution. Differences between groups were determined by Student’s t test. Differences were regarded significant when p < 0.05 (two-sided).
Results
RV lead in the apical position
Eighty-three consecutive pacemaker patients with an apical RV lead were included in this study. Table 1 shows the patients’ baseline characteristics. The mean age and comorbidities are consistent with a typical pacemaker patient collective.
In the presence of a narrow QRS the mean intrinsic QRS (QRSi) duration measured by the experienced electrophysiologist was 97 ± 8 ms with a mean JTi interval of 302 ± 33 ms and a mean QTi interval of 398 ± 33 ms. The mean intrinsic QTc (QTci) interval was 417 ± 34 ms. No significant difference was observed for values measured by the trainee: QRSi duration: 97 ± 8 ms; JTi interval 298 ± 33 ms; QTi interval 394 ± 34 ms; QTci interval 409 ± 36 ms. During apical RV pacing and LBBB the intervals assessed by the experienced electrophysiologist were: QRSLBBB duration 171 ± 18 ms, JTLBBB interval 280 ± 28 ms, QTLBBB interval 451 ± 29 ms. These measurements led to a QTcLBBB interval of 544 ± 46 ms that was prolonged compared with that of intrinsic rhythm, as anticipated. Again, the values measured by the trainee did not vary significantly from these values: QRSLBBB duration 171 ± 18 ms, JTLBBB interval 287 ± 29 ms, QTLBBB interval 456 ± 32 ms, QTcLBBB interval 551 ± 52 ms.
The corrected QT interval derived from the Bogossian formula was 366 ± 27 ms for values obtained by the electrophysiologist and 371 ± 30 ms for values obtained by the trainee. After correction for heart rate by application of the Bazett formula, the modified QTc intervals were 440 ± 36 ms as measured by the experienced electrophysiologist and 447 ± 41 ms as measured by the trainee. Table 2 shows the mean values of the pooled ECG measurements of both examiners.
It is worth mentioning that the difference between the true intrinsic QT interval in the presence of a narrow QRS and the corrected QT interval with LBBB was more distinct when heart rate correction by the Bazett formula was performed before employing the Bogossian formula (QTcm 470 ± 39 ms vs. QTci 413 ± 36 ms). This is why it is recommended to apply the Bazett formula only after assessment of the adjusted QT interval.
RV lead in the non-apical position
Eighty consecutive pacemaker patients with a RV lead in the non-apical position were included in this study. Patients with a non-apical RV lead were younger (71 ± 13 years vs. 79 ± 9 years; p < 0.001) and had a lower prevalence of atrial fibrillation (22 vs. 41%; p = 0.01) than those with an apical lead. Nevertheless, ECG measurements were comparable to those obtained in patients with an apical RV lead. Here, mean QRSi duration measured by the experienced electrophysiologist was 96 ± 8 ms, resulting in a JTi interval of 298 ± 30 ms and a QTi interval of 394 ± 30 ms. No significant differences were observed for values assessed by the trainee: QRSi duration: 96 ± 8 ms, JTi interval 297 ± 31 ms, QTi interval 393 ± 31 ms. During RV pacing the following intervals were measured by the experienced electrophysiologist and the trainee, respectively: QRSLBBB duration 156 ± 18 ms (vs. 156 ± 18 ms), JTLSB interval 285 ± 29 ms (vs. 285 ± 29 ms), QTLBBB interval 441 ± 30 ms (vs. 442 ± 31 ms), QTcLBBB interval 522 ± 41 ms (vs. 524 ± 43 ms).
After use of the Bogossian formula the corrected QT interval was 363 ± 28 ms for values obtained by both the electrophysiologist and the trainee. Heart rate correction by Bazett’s formula led to modified QTc intervals of 429 ± 34 ms for values obtained by the experienced electrophysiologist and 430 ± 35 ms for those measured by the trainee. The pooled mean values of the two examiners for the ECG measurements in the non-apical position are listed in Table 2.
As mentioned above for patients with apical leads, the difference between corrected intrinsic QTci interval and corrected modified QTc interval in LBBB was more marked when heart rate correction by the Bazett formula was performed before application of the Bogossian formula (QTcm 447 ± 34 ms vs. QTci 416 ± 32 ms).
Deviation of the intrinsic QTc from the modified QTc during LBBB and heart rate regression
Intrinsic QTc intervals were compared with the values obtained for the modified QTc interval during paced LBBB after use of the Bogossian formula. An accepted deviation of 30 ms (according to 7.6% of intrinsic QTci) reached a significant value in the equivalent paired t-test (Table 3). The regression analysis revealed a linear relationship between the deviation of the intrinsic QTc from the modified QTc and the difference between the intrinsic heart rate and paced heart rate (Fig. 4). A fast heart rate resulted in an increasing difference between intrinsic and modified QTc.
Discussion
The implication of a long QT interval for cardiovascular risk stratification has been demonstrated in large populations [9, 10]. A bundle brunch block is commonly associated with an extended QTc interval. However, the QT interval, which is easily overestimated, is the result of a prolongation of depolarisation and not of repolarisation [3]. In the past, it was suggested that the JT interval may be measured in patients with LBBB as an alternative method of risk stratification in the presence of LBBB [11]. A different approach in pacemaker recipients is the subtraction of 50 ms of the QTcLBBB as a rule of thumb, leading to reasonable values at a paced rate of 66 bpm (± 16 ms). Higher paced rates lead to a relevant overestimation of up to 81 ms [12]. A specific RV lead position-dependent QTc measurement was not conducted.
Recently, the Bogossian formula was evaluated in a heart failure patient collective with transvenous ICDs. The formula delivered acceptable results in comparing the true QT interval in a narrow QRS with the corrected QT interval in LBBB, although the formula led to a slight overestimation of the true QT interval (± 25 ms) in this patient cohort [13]. Since chronic heart failure is known to be associated with a prolonged repolarization period as a result of complex electrical remodelling and a downregulation of cardiac potassium currents, we sought to investigate the Bogossian formula in a pacemaker patient collective with normal left ventricular function [14,15,16].
Right ventricular lead position and operator dependency
The localization of the RV pacing lead profoundly influences the morphology of the QRS complex and thus the ensuing repolarization period. Results from our previous studies showed no significant differences between values obtained from right ventricular apical pacing and from pacing in the right ventricular outflow tract [3, 13]. In the present study that included patients with preserved ejection fraction, the results for QTc adjustment were similar to those observed in the heart failure patient collective studied previously [13]. Interestingly, in the pacemaker patient cohort a reduced width of QRS complexes was associated with non-apical RV lead position. In the literature, data concerning QRS width and the position of the RV lead are contradictory [17, 18]. In particular, pacing in the high RV outflow tract leads to broad QRS complexes with a width that is similar to that obtained in the apical pacing position. In our experience, QRS complexes can be expected to be rather narrow only if the lead is in absolute proximity to the sound intrinsic cardiac conduction system, which we have usually observed to be mid-septal. Although a non-apical RV lead position results in an improved calculation of QTc with significantly less deviation to the true QTci, our results suggest that the Bogossian formula can be effectively applied in pacemaker patients independent of the position of the RV lead.
Accurate analysis of ECG parameters is essential for precise determination of the QT interval. The aspect of investigator-dependant divergent results is also addressed in the current recommendations for ECG interpretation [7]. In the present study, ECG parameters were assessed by two independent operators. No significant differences were observed between the experienced electrophysiologist and the trainee. This applied for all measured values as well as for calculation of the corrected QT interval employing the Bogossian formula. These findings underline the fact that general analysis of ECG parameters can and needs to be standardized and that the Bogossian formula can easily be applied by any physician.
Systematic deviation of the corrected QT interval
In the present study, a slight systematic overestimation of the true QT interval by the Bogossian formula was observed in almost all individuals, which is comparable to our recent findings in heart failure patients. The corrected QT interval was about 25 ± 21 ms longer than QTci. This phenomenon was detected in all patients independent of RV lead position. Of note, these results are consistent with well-known divergences reported for heart rate-dependant QT correction using Bazett’s or Fridericia’s formula where deviations of up to 15% are considered to be acceptable [7]. Of note, the Bogossian formula for correction of the QT interval in the presence of LBBB displayed a mean deviation of only 5.5% (from the mean intrinsic QTc interval). In the present study, the deviation of the QTci from the modified QTc was driven mainly by an increasing alteration between intrinsic heart rate and stimulated heart rate during threshold measurement (Fig. 4). The fact that the Bogossian formula tends to slightly overestimate the true QT interval may be regarded as a kind of safety margin for risk assessment during therapy with QT-prolonging drugs. On the other hand in cases with borderline QTc prolongation, bearing a marginal QTc overestimation in mind, unnecessary discontinuation of medication should be avoided.
Limitations
LBBB induced by RV pacing features differences compared to intrinsic LBBB regarding the ventricular activation pattern. This may contribute to the deviation observed between the intrinsic and modified QTc interval.
Conclusion
The Bogossian formula is a simple and reliable tool that can be used in routine clinical practice for QTc interval evaluation in pacemaker patients with LBBB due to apical or non-apical right ventricular pacing. The observed overestimation of the QTc interval of approximately 15 ms (for non-apical pacing) and 30 ms (for apical pacing) should be taken into consideration when using the Bogossian formula in pacemaker recipients.
References
Woosley RL, Romero K (2013) Assessing cardiovascular drug safety for clinical decision-making. Nat Rev Cardiol 10(6):330–337
Schneider JF, Thomas HE Jr, McNamara PM, Kannel WB (1985) Clinical-electrocardiographic correlates of newly acquired left bundle branch block: the Framingham Study. Am J Cardiol 55(11):1332–1338
Bogossian H, Frommeyer G, Ninios I, Hasan F, Nguyen QS et al (2014) New formula for evaluation of the QT interval in patients with left bundle branch block. Heart Rhythm 11(12):2273–2277
Bogossian H, Frommeyer G, Ninios I, Hasan EP F, et al.: A new experimentally validated formula to calculate the QT-interval in the presence of left bundle branch block holds true in the clinical setting. Ann Noninvasive Electrocardiol. 2016 in press
Markewitz A (2015) Annual report 2013 of the German Cardiac Pacemaker And Defibrillator Register–Part 2: implantable cardioverter-defibrillators. Pacemaker and AQUA Institute for Applied Quality Improvement and Research in Health Care GmbH workgroup. Herzschrittmacherther Elektrophysiol. 26(4):399–423
Markewitz A (2015) Annual report 2013 of the German Cardiac Pacemaker and Defibrillator Register, part 1–Pacemaker. Pacemaker and AQUA Institute for Applied Quality Improvement and Research in Health Care GmbH workgroup. Herzschrittmacherther Elektrophysiol 26(4):374–398
Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R et al (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 119(10):e241-e250
Postema PG, De Jong JS, Van der Bilt IA, Wilde AA (2008) Accurate electrocardiographic assessment of the QT interval: teach the tangent. Heart Rhythm 5(7):1015–1018
Nielsen JB, Graff C, Rasmussen PV, Pietersen A, Lind B et al (2014) Risk prediction of cardiovascular death based on the QTc interval: evaluating age and gender differences in a large primary care population. Eur Heart J 35(20):1335–1344
Priori SG, Schwartz PJ, Napolitano C, Bloise R, Ronchetti E et al (2003) Risk stratification in the long-QT syndrome. N Engl J Med 348(19):1866–1874
Rautaharju PM, Zhang ZM, Prineas R, Heiss G (2004) Assessment of prolonged QT and JT intervals in ventricular conduction defects. Am J Cardiol 93(8):1017–1021
Chakravarty S, Kluger J, Chhabra L, Ramu B, Coleman C (2015) Corrected QT in ventricular paced rhythms: what is the validation for commonly practiced assumptions? Cardiology 130(4):207–210
Frommeyer G, Bogossian H, Pechlivanidou E, Conzen P, Gemein C et al (2017) Applicability of a novel formula (Bogossian formula) for evaluation of the QT-interval in heart failure and left bundle branch block due to right ventricular pacing. Pacing Clin Electrophysiol 40(4):409–416
Frommeyer G, Milberg P, Witte P, Stypmann J, Koopmann M et al (2011) A new mechanism preventing proarrhythmia in chronic heart failure: rapid phase-III repolarization explains the low proarrhythmic potential of amiodarone in contrast to sotalol in a model of pacing-induced heart failure. Eur J Heart Fail 13(10):1060–1069
Frommeyer G, Rajamani S, Grundmann F, Stypmann J, Osada N et al (2012) New insights into the beneficial electrophysiologic profile of ranolazine in heart failure: prevention of ventricular fibrillation with increased postrepolarization refractoriness and without drug-induced proarrhythmia. J Card Fail 18(12):939–949
Vrtovec B, Ryazdanbakhsh AP, Pintar T, Collard CD, Gregoric ID, Radovancevic B (2006) QTc interval prolongation predicts postoperative mortality in heart failure patients undergoing surgical revascularization. Texas Heart Inst J 33(1):3–8
Inoue K, Okayama H, Nishimura K, Saito M, Yoshii T et al (2011) Right ventricular septal pacing preserves global left ventricular longitudinal function in comparison with apical pacing: analysis of speckle tracking echocardiography. Circ J 75(7):1609–1615
Pang BJ, Kumar S, Tacey MA, Mond HG (2014) Capturing the His-Purkinje system is not possible from conventional right ventricular apical and nonapical pacing sites. Pacing Clin Electrophysiol 37(6):724–730
Acknowledgements
We thank Inga Bayh and Prof. Dr. Frank Krummenauer (Institute for Medical Biometry and Epidemiology, School of Medicine, Faculty of Health, Witten/Herdecke University, Witten, Germany) for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to disclose.
Rights and permissions
About this article
Cite this article
Weipert, K.F., Bogossian, H., Conzen, P. et al. Application of the Bogossian formula for evaluation of the QT interval in pacemaker patients with stimulated left bundle branch block. Clin Res Cardiol 107, 1033–1039 (2018). https://doi.org/10.1007/s00392-018-1275-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1275-6