Abstract
Aims
Beta-blockers are recommended for the treatment of chronic heart failure (CHF). However, it is disputed whether beta-blockers exert a class effect or whether there are differences in efficacy between agents.
Methods and results
6010 out-patients with stable CHF and a reduced left ventricular ejection fraction prescribed either bisoprolol, carvedilol or metoprolol succinate were identified from three registries in Norway, England, and Germany. In three separate matching procedures, patients were individually matched with respect to both dose equivalents and the respective propensity scores for beta-blocker treatment. During a follow-up of 26,963 patient-years, 302 (29.5%), 637 (37.0%), and 1232 (37.7%) patients died amongst those prescribed bisoprolol, carvedilol, and metoprolol, respectively. In univariable analysis of the general sample, bisoprolol and carvedilol were both associated with lower mortality as compared with metoprolol succinate (HR 0.80, 95% CI 0.71–0.91, p < 0.01, and HR 0.86, 95% CI 0.78–0.94, p < 0.01, respectively). Patients prescribed bisoprolol or carvedilol had similar mortality (HR 0.94, 95% CI 0.82–1.08, p = 0.37). However, there was no significant association between beta-blocker choice and all-cause mortality in any of the matched samples (HR 0.90; 95% CI 0.76–1.06; p = 0.20; HR 1.10, 95% CI 0.93–1.31, p = 0.24; and HR 1.08, 95% CI 0.95–1.22, p = 0.26 for bisoprolol vs. carvedilol, bisoprolol vs. metoprolol succinate, and carvedilol vs. metoprolol succinate, respectively). Results were confirmed in a number of important subgroups.
Conclusion
Our results suggest that the three beta-blockers investigated have similar effects on mortality amongst patients with CHF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beta-blockers have become one of the mainstays of chronic heart failure (CHF) therapy since they improve both morbidity and mortality in patients with reduced ejection fraction [1,2,3,4,5,6,7,8]. Current guidelines advise the use of bisoprolol, carvedilol and metoprolol succinate interchangeably in the treatment of CHF [1, 2]. Given that beta-blockers differ in their selectivity for adrenergic receptors, their lipophilicity and their effects on peripheral circulation [9], there is, however, the question whether beta-blockers exert a class effect or whether any beta-blocker is superior to another [10,11,12,13].
As almost all key beta-blocker trials have compared beta-blockers against placebo [3,4,5,6,7,8], prospective data on the comparative effectiveness of beta-blockers are scarce [14, 15]. Since published head-to-head comparisons have not been convincing, a variety of meta-analyses and retrospective studies has been published [12, 13, 16,17,18,19,20,21,22,23]. The results, however, were inconclusive. Thus, there is little evidence to inform clinical decisions.
In the present study, we compared the prognosis of patients prescribed bisoprolol, carvedilol or metoprolol succinate in a contemporary multicentre real-world cohort of patients with stable CHF from three European countries.
Methods
Databases
Patients’ data were extracted from three different European heart failure databases: the Norwegian Heart Failure Registry, the Heart Failure Registry of the Department of Academic Cardiology, University of Hull, UK, and the Heart Failure Registry of the University of Heidelberg, Germany. Recruitment was prospective and continuous for each database and centre. All patients gave their written informed consent for data storage and evaluation. The study conformed to the principles outlined in the Declaration of Helsinki and was approved by the local ethics committees.
The Norwegian Heart Failure Registry was initiated in October 2000 and patients were enrolled from outpatients’ clinics of 27 recruiting hospitals well distributed in all regions of Norway ranging in size and scope from small community to large university hospitals. The participating centres recorded their data using a web-based database.
Patients who attended the community heart failure clinics of the University of Hull, UK, and the University of Heidelberg, Germany, for evaluation of heart failure were offered inclusion into the local heart failure registries. Since both university hospitals are providers of secondary and tertiary care, the registries reflect a broad representation of patients of their respective regions.
Patient selection and follow-up
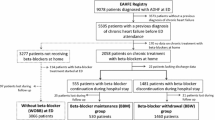
All databases reflect all-comer cohorts. Patients were included after stabilisation of both clinical status and medication. Patients were eligible for the study if they met the following criteria: (a) attendance at the heart failure outpatient clinic of any of the participating hospitals, (b) written informed consent for inclusion into the respective heart failure registry, (c) history of heart failure due to left ventricular systolic dysfunction. Medication was at the discretion of the referring physician. For further analyses, we selected patients who were treated with either bisoprolol, carvedilol or metoprolol succinate in conjunction with either an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker. The present analysis was restricted to bisoprolol, carvedilol and metoprolol succinate, since their use is recommended by guidelines and they were commonly prescribed in the three heart failure registries (Fig. 1).
Target doses and dose equivalents for beta-blockers were derived from ESC guidelines for the diagnosis and treatment of acute and chronic heart failure [1]. For example, daily doses of 10 mg bisoprolol or 50 mg carvedilol were both considered as 100% dose equivalent, while 5 mg bisoprolol and 25 mg carvedilol were defined as 50% dose equivalent.
The diagnosis of heart failure was established according to guidelines on the basis of typical symptoms and signs associated with an objective abnormality of cardiac structure or function on echocardiography, cardiac magnetic resonance imaging, or left heart catheterisation [1]. All patients included in the present analysis had a left ventricular ejection fraction (LVEF) <45%.
Baseline characteristics included medical history, physical examination, LVEF, blood count and chemistry, and medication. Glomerular filtration rate (GFR) was estimated using the modification of diet in renal disease (MDRD) formula [24].
Surviving patients were followed up for a minimum of 6 months. Determination of survival status and follow-up were performed by scheduled visits to the outpatient clinic, by telephone calls either to the patients’ homes or to their physicians, or by electronic hospital records. For the purpose of the present analysis, patients were censored as “alive” at the date of this last contact. In addition, for the Norwegian Heart Failure Registry, mortality data were obtained at regular intervals from the National Registry and no patients were lost to follow-up. Patients who underwent heart transplantation were followed until transplantation and censored thereafter. All-cause mortality was the predefined endpoint of the study.
Statistical analysis
All tests are two-tailed and a p value of less than 5% was regarded as being statistically significant. Variables are presented as mean ± standard deviation, median (interquartile range), or number [percentages (%)] as appropriate. Chi-squared tests were used to compare frequencies. To test for significant differences between groups, the Kruskal–Wallis test and analysis of variance (ANOVA) tests were used where appropriate.
In order to prevent bias in further statistical analyses due to missing baseline values, we performed a multiple imputation analysis with n = 100 repetitions using the Markov chain Monte Carlo method. This procedure replaces each missing value with a set of plausible values that represent the uncertainty about the correct value for imputation.
Differences in event-free survival between patients treated with bisoprolol, carvedilol or metoprolol succinate were analysed using Cox proportional hazard models and displayed using the Kaplan–Meier method for survival. To account for possible confounders, patients were matched with respect to beta-blocker treatment using pairwise multi-level propensity score matching as described below. Survival analyses were then repeated in matched cohorts.
Propensity score calculation and matching
Propensity scores were calculated as the single composite variable from a non-parsimonious multivariate logit-linked binary logistic regression of the baseline characteristics. The beta-blocker agent was the dependent variable [25]. In a first step, propensity scores were calculated separately for “bisoprolol vs. carvedilol”, “bisoprolol vs. metoprolol succinate”, and “carvedilol vs. metoprolol succinate” as dependent variables. Propensity scores were derived from all baseline variables (except beta-blocker dose equivalent) using the multiple imputed baseline data sets. The logits of the probability of receiving a certain beta-blocker according to the respective propensity scores formed the basis of three separate matching procedures. Dose equivalent of the respective beta-blocker was not part of the propensity scores to account separately for one of the main criticisms of the Carvedilol or Metoprolol European Trial (COMET) trial [14, 26].
Patients were individually matched for both the propensity of receiving a particular beta-blocker AND their dose equivalents. Each matching procedure was performed in two steps: First, calliper matching of the propensity score was applied with calliper size predefined as 0.2 of the standard deviation of the total sample. In a one-pass procedure starting with a given patient receiving a certain beta-blocker (e.g., bisoprolol), the closest match of a patient receiving a different beta-blocker (e.g., carvedilol) was identified. Second, dose equivalents for the beta-blockers were compared. If doses were equivalent or varied ≤10%, the pair of patients was retained for analysis and removed from the total sample to allow for the next matching cycle to take place. If doses varied >10%, the pair was rejected. Then the first step of the matching process was repeated to identify the next closest match to the given bisoprolol patient of the failed match according to the propensity score. If a further patient on carvedilol was, thus, identified, the second step was repeated. If no match according to the propensity score AND dose equivalent could be identified, the bisoprolol patient was removed from the total sample and the matching cycle started with the next bisoprolol patient.
The matching procedures of patients treated with bisoprolol vs. metoprolol succinate and carvedilol vs. metoprolol succinate were performed analogously. Owing to this statistical design, the matched patients included in each drug cohort differed between comparisons.
Bias reduction, balance and sensitivity analysis
The balance of baseline covariates before and after matching was assessed using standardised differences [27]. Standardised difference scores are intuitive indexes which measure the effect size between two groups. Compared to a t test or Wilcoxon rank-sum test, they are independent of sample size. Thus, their use can be recommended for comparing baseline covariates in clinical trials as well as propensity score-matched studies. In addition, we conducted a formal sensitivity analysis to quantify the degree of a hidden bias that would need to be present to invalidate our main conclusions following the method suggested by Love [28].
Subgroups
Analyses were repeated in pre-specified subgroups of the matched samples with respect to age (above vs. below median), sex, LVEF (≤35 vs. >35%), NYHA functional class (I/II vs. III/IV), heart rate (≤75 vs. >75/min), and rhythm (sinus rhythm yes vs. no). Interaction terms were calculated for each of the predefined subgroups in the propensity-matched samples.
Results
Of 6010 patients who met the inclusion criteria outlined above, 4011 patients were from Norway, 1171 patients were from Germany, and 728 patients were from England.
Bisoprolol was prescribed for 1023 patients (17.0%) with a median dose of 5 (2.5–10) mg/day [equivalent to 50 (25–100)% of target dose], carvedilol for 1721 patients (28.6%) with a median dose of 25 (12.5–50) mg/day [equivalent to 50 (25–100)% of target dose], and metoprolol succinate for 3266 patients with a median dose of 100 (50–150) mg/day [equivalent to 52.6 (26.3–100)% of target dose].
Baseline characteristics of CHF patients differed with respect to beta-blocker treatment for a substantial number of variables (Table 1). Overall, patients receiving metoprolol succinate were older and more likely to have NYHA functional class III symptoms than those on carvedilol. In addition, the proportion of patients with ischemic heart disease was higher in the metoprolol succinate group.
Total follow-up was 323,560 patient-months (26,963 patient-years) with a median follow-up duration of 49 (26–76) months. For bisoprolol, median follow-up was 46 (26–72) months, whereas it was 56 (30–84) months and 47 (25–74) months for carvedilol and metoprolol succinate, respectively. During that time 2171 (36.1%) patients died: 302 (29.5%) on bisoprolol, 637 (37.0%) on carvedilol, and 1232 (37.7%) on metoprolol succinate.
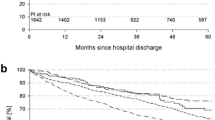
In univariable analysis of the overall cohort, patients prescribed bisoprolol and carvedilol therapy both had lower mortality when compared with those prescribed metoprolol succinate (HR 0.80, 95% CI 0.71–0.91, p < 0.01, and HR 0.86, 95% CI 0.78–0.94, p < 0.01, respectively). Survival on bisoprolol was similar to that on carvedilol (HR 0.94, 95% CI 0.82–1.08, p = 0.37). Kaplan–Meier curves for 10-year survival of CHF outpatients with respect to beta-blocker treatment are shown in Fig. 2.
The matching procedures identified 839, 986 and 1380 pairs of patients with similar dose equivalent for each of the three comparisons (bisoprolol vs. carvedilol, bisoprolol vs. metoprolol succinate and carvedilol vs. metoprolol). Of these, 553 (33%), 554 (28%), and 941 (34%) patients died during 10-year follow-up, respectively. Each of the propensity score matching procedures significantly reduced standardised differences below 10% in the absolute values for most observed covariates, demonstrating an improvement in the covariate balance across the treatment groups. Figure 3 shows standardised differences of baseline variables before (a) and after (b) matching in each of the three matched cohorts. For example, in the overall cohort, the standardised difference of left ventricular ejection fraction between patients treated with bisoprolol and those given carvedilol was ≈20%. However, after matching, the standardised difference of left ventricular ejection fraction was reduced to 0%.
Absolute standardised differences before (a) and after (b) propensity score matching comparing covariate values for hospital outpatients with chronic heart failure receiving bisoprolol vs. carvedilol, bisoprolol vs. metoprolol succinate, and carvedilol vs. metoprolol succinate, respectively. ACEi angiotensin-converting enzyme, ARB angiotensin receptor blocker, eGFR estimated glomerular filtration rate using the Modification of Diet in Renal Disease equation, HR heart rate, BPsys systolic blood pressure, LVEF left ventricular ejection fraction, aHT arterial hypertension, OPD obstructive pulmonary disease, NYHA New York Heart Association functional class, BMI body mass index
Cox proportional hazard analyses did not find any significant association between the particular beta-blocker prescribed and all-cause mortality in any of the matched samples (bisoprolol vs. carvedilol, HR 0.90, 95% CI 0.76–1.06, p = 0.20; bisoprolol vs. metoprolol succinate HR 1.10, 95% CI 0.93–1.31, p = 0.24; carvedilol vs. metoprolol succinate HR 1.08, 95% CI 0.95–1.22, p = 0.26). The Kaplan–Meier curves for survival of matched CHF patients with respect to beta-blocker treatment are presented in Figs. 4, 5 and 6.
Subgroup analyses mainly confirmed that none of the beta-blockers was inferior to any other with two exceptions: in patients without sinus rhythm, there was a survival benefit of metoprolol succinate over carvedilol (p = 0.03), and in patients with a resting heart rate ≤75/min, there was a marginally significant benefit of carvedilol over bisoprolol (p = 0.05). The interaction terms indicated that there was no significant interaction between subgroups and individual beta-blocker agents. The relevant plot is shown in Fig. 7.
Cox regression analyses for all-cause mortality regarding beta-blocker use in the predefined subgroups for the propensity score-matched cohorts. LVEF left ventricular ejection fraction, NYHA New York Heart Association functional class. *p for interaction refers to subgroups of each propensity matched sample
The formal sensitivity analyses indicate only a small residual bias. The respective Γ-values were 0.93, 0.65, and 0.78 for bisoprolol vs. carvedilol, bisoprolol vs. metoprolol succinate, and carvedilol vs. metoprolol succinate (no residual bias at Γ = 1.0). This means that in order to attribute a possible survival benefit to an unobserved covariate rather than the receipt of, e.g., bisoprolol (vs. carvedilol), that unobserved covariate would only need to produce a 7% increase in the odds of receipt of bisoprolol while being a weak predictor of all-cause mortality.
Discussion
We found no evidence for a difference in survival amongst patients prescribed bisoprolol, carvedilol, or metoprolol succinate and all-cause mortality in a large contemporary international cohort of patients with stable CHF and reduced ejection fraction. The finding was consistent through a range of important subgroups including patients in sinus rhythm for whom the benefits of beta-blockers are best established. Our results support the view that the reduction in mortality compared to placebo was similar across landmark trials that used these three beta-blockers [3, 4, 7, 8].
Our results contrast to the Carvedilol or Metoprolol European Trial (COMET) that is the only adequately powered randomised head-to-head comparison of two beta-blockers. In COMET, carvedilol was associated with better survival than metoprolol tartrate in 3029 patients with CHF symptoms (NYHA II–IV) and LVEF <35% [14]. However, metoprolol was used at a lower dose and with a different formulation than that proved to reduce mortality [4, 8]. A network meta-analysis of eight randomised beta-blocker trials including 4563 patients reported a potential benefit in favour of carvedilol over beta 1-receptor selective blockers [13], but 94% of the deaths derived from the COMET trial. The results must therefore be interpreted with caution. Our analysis supports results from other observational studies [16, 17, 22] and meta-analyses [12, 19, 23] that found carvedilol and metoprolol similarly effective. Some of these studies included metoprolol tartrate [12, 16] and did not account for beta-blocker dose [17, 19]. Our study therefore adds important evidence to current knowledge.
In patients who were not in sinus rhythm, however, we noted a benefit of metoprolol succinate over carvedilol, although this may have been a chance finding reflecting the number of comparisons being made. However, this again contrasts with a post hoc analysis from the COMET trial that reported additional benefits on mortality and morbidity of carvedilol relative to metoprolol tartrate in patients with CHF whether or not they were in atrial fibrillation. We have previously reported similar effectiveness of carvedilol and metoprolol succinate in 1480 matched patients irrespective of the underlying heart rhythm [22]. Prior meta-analyses have questioned the prognostic benefit of beta-blockers in patients with CHF in atrial fibrillation [29, 30]. Here it is important to note that our results merely indicate equal effectiveness of the beta-blockers concerned but—in the absence of an alternative comparator—cannot assess overall effectiveness.
The Multistep Administration of bisoprolol IN Chronic Heart Failure II (MAIN-CHF II) trial prospectively compared bisoprolol and carvedilol in the treatment of Japanese patients with mild to moderate CHF [15]. The trial, however, recruited only 59 patients and therefore lacks statistical power to test non-inferiority of bisoprolol vs. carvedilol. An observational study of 217 patients with CHF and NYHA functional class III/IV symptoms reported no significant differences in the survival and cardiac event-free rates between treatment groups [18]. In addition, prospective trials found comparable tolerability of bisoprolol and carvedilol [31, 32]. Similarly, our study does not find any evidence of superiority of carvedilol over bisoprolol while including a much larger cohort of contemporary CHF patients.
Bisoprolol and metoprolol succinate are both lipophilic beta 1-receptor selective blockers. However, their relative beta 1/beta 2-affinities differ, varying between 2.3 and 35 for metoprolol and 13.5–18 for bisoprolol [9, 33, 34]. The difference may be of clinical relevance, but there are no prospective trials on the comparative effectiveness of bisoprolol vs. metoprolol succinate in patients with CHF. An indirect head-to-head comparison using Bayesian network meta-analysis of randomised beta-blocker trials as well as an analysis from the Danish Heart Failure Registry did not find any statistical evidence for the superiority of bisoprolol vs. metoprolol [12, 21]. However, the inclusion of both metoprolol succinate and metoprolol tartrate trials limits the informative value of the analyses. Moreover, the proportion of bisoprolol users in the Danish study was rather small (11.2%), and it is unclear how many patients received target doses of beta-blockers. In contrast, our study was performed with particular focus on equal dosing of beta-blockers.
Limitations
As with any non-randomised, observational design, the present study may be subject to unmeasured confounders. Sensitivity analyses cannot prove or rule out the presence of such an unmeasured confounder. However, our data result from comprehensive outpatient databases with continuous inclusion and close surveillance. The detailed characterization of patients allows consideration of various potential confounders through the use of comprehensive propensity score models. The large sample size and inclusion of patients from three European countries are obvious strengths of the present study. The results are therefore likely to be generalizable to other CHF populations. We observed substantial differences in patient characteristics between countries. However, as patient characteristics were used for propensity score calculation and matching, we expect that this should not have an impact on our results in the matched cohorts. We further cannot comment on the specific reasons for the selection of a particular beta-blocker, nor on medication adherence. In addition, our data do not allow identification of patients who either switched from one beta-blocker to another or changed the beta-blocker dose during follow-up. As inclusion into the analyses of our study was performed after stabilisation of both clinical status and medication in an ambulatory setting, however, this may reduce the necessity for further modulation of beta-blocker treatment.
From this observational study, we can infer that there is no association between the beta-blocker prescribed and mortality but we cannot be sure that the lack of observed difference truly reflects similar benefit. Ideally, our results should be confirmed in a large-scale, randomised head-to-head comparison of beta-blockers. Given the required sample size and associated costs, such a trial may never be done.
Conclusion
In an international, real-world cohort of CHF patients with reduced ejection fraction, we found no difference in all-cause mortality for patients treated with bisoprolol, carvedilol or metoprolol succinate. The finding was consistent in subgroups with respect to age, sex, LVEF, NYHA functional class, heart rate, and rhythm. In accordance with current guidelines, this analysis suggests that bisoprolol, carvedilol, and metoprolol succinate may be used interchangeably in the treatment of patients with CHF.
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force M (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. doi:10.1093/eurheartj/ehw128
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos G, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2016) 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. doi:10.1016/j.jacc.2016.05.011
The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial (1999). Lancet 353 (9146):9–13
MERIT-HF investigators: effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF) (1999). Lancet 353 (9169):2001–2007
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH (1996) The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 334(21):1349–1355. doi:10.1056/NEJM199605233342101
Packer M, Colucci WS, Sackner-Bernstein JD, Liang CS, Goldscher DA, Freeman I, Kukin ML, Kinhal V, Udelson JE, Klapholz M, Gottlieb SS, Pearle D, Cody RJ, Gregory JJ, Kantrowitz NE, LeJemtel TH, Young ST, Lukas MA, Shusterman NH (1996) Double-blind, placebo-controlled study of the effects of carvedilol in patients with moderate to severe heart failure. The PRECISE Trial. Prospective Randomized Evaluation of Carvedilol on Symptoms and Exercise. Circulation 94(11):2793–2799
Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P, Rouleau JL, Tendera M, Castaigne A, Roecker EB, Schultz MK, DeMets DL; Carvedilol Prospective Randomized Cumulative Survival Study G (2001) Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 344(22):1651–1658. doi:10.1056/NEJM200105313442201
Hjalmarson A, Goldstein S, Fagerberg B, Wedel H, Waagstein F, Kjekshus J, Wikstrand J, El Allaf D, Vitovec J, Aldershvile J, Halinen M, Dietz R, Neuhaus KL, Janosi A, Thorgeirsson G, Dunselman PH, Gullestad L, Kuch J, Herlitz J, Rickenbacher P, Ball S, Gottlieb S, Deedwania P (2000) Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group. JAMA J Am Med Assoc 283(10):1295–1302
Baker JG (2010) The selectivity of beta-adrenoceptor agonists at human beta1-, beta2- and beta3-adrenoceptors. Br J Pharmacol 160(5):1048–1061. doi:10.1111/j.1476-5381.2010.00754.x
Lechat P, Packer M, Chalon S, Cucherat M, Arab T, Boissel JP (1998) Clinical effects of beta-adrenergic blockade in chronic heart failure: a meta-analysis of double-blind, placebo-controlled, randomized trials. Circulation 98(12):1184–1191
Brophy JM, Joseph L, Rouleau JL (2001) Beta-blockers in congestive heart failure. A Bayesian meta-analysis. Ann Intern Med 134(7):550–560
Chatterjee S, Biondi-Zoccai G, Abbate A, D’Ascenzo F, Castagno D, Van Tassell B, Mukherjee D, Lichstein E (2013) Benefits of beta blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. BMJ 346:f55. doi:10.1136/bmj.f55
DiNicolantonio JJ, Lavie CJ, Fares H, Menezes AR, O’Keefe JH (2013) Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol 111(5):765–769. doi:10.1016/j.amjcard.2012.11.031
Poole-Wilson PA, Swedberg K, Cleland JG, Di Lenarda A, Hanrath P, Komajda M, Lubsen J, Lutiger B, Metra M, Remme WJ, Torp-Pedersen C, Scherhag A, Skene A, Carvedilol Or Metoprolol European Trial I (2003) Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet 362(9377):7–13. doi:10.1016/S0140-6736(03)13800-7
Hori M, Nagai R, Izumi T, Matsuzaki M (2014) Efficacy and safety of bisoprolol fumarate compared with carvedilol in Japanese patients with chronic heart failure: results of the randomized, controlled, double-blind, Multistep Administration of bisoprolol IN Chronic Heart Failure II (MAIN-CHF II) study. Heart Vessels 29(2):238–247. doi:10.1007/s00380-013-0340-3
Lazarus DL, Jackevicius CA, Behlouli H, Johansen H, Pilote L (2011) Population-based analysis of class effect of beta blockers in heart failure. Am J Cardiol 107(8):1196–1202. doi:10.1016/j.amjcard.2010.12.017
Pasternak B, Svanstrom H, Melbye M, Hviid A (2014) Association of treatment with carvedilol vs metoprolol succinate and mortality in patients with heart failure. JAMA Intern Med 174(10):1597–1604. doi:10.1001/jamainternmed.2014.3258
Konishi M, Haraguchi G, Kimura S, Inagaki H, Kawabata M, Hachiya H, Hirao K, Isobe M (2010) Comparative effects of carvedilol vs bisoprolol for severe congestive heart failure. Circ J 74(6):1127–1134
Wikstrand J, Wedel H, Castagno D, McMurray JJ (2014) The large-scale placebo-controlled beta-blocker studies in systolic heart failure revisited: results from CIBIS-II, COPERNICUS and SENIORS-SHF compared with stratified subsets from MERIT-HF. J Intern Med 275(2):134–143. doi:10.1111/joim.12141
Shore S, Aggarwal V, Zolty R (2012) Carvedilol or sustained-release metoprolol for congestive heart failure: a comparative effectiveness analysis. J Cardiac Fail 18(12):919–924. doi:10.1016/j.cardfail.2012.10.016
Pasternak B, Mattsson A, Svanstrom H, Hviid A (2015) Comparative effectiveness of bisoprolol and metoprolol succinate in patients with heart failure. Int J Cardiol 190:4–6. doi:10.1016/j.ijcard.2015.03.441
Fröhlich H, Zhao J, Täger T, Cebola R, Schellberg D, Katus H, Grundtvig M, Hole T, Atar D, Agewall S, Frankenstein L (2015) Carvedilol compared to metoprolol succinate in the treatment and prognosis of patients with stable chronic heart failure. The Carvedilol or Metoprolol Evaluation Study (COMES). Circ Heart Fail. doi:10.1161/CIRCHEARTFAILURE.114.001701
Briasoulis A, Palla M, Afonso L (2015) Meta-analysis of the effects of carvedilol versus metoprolol on all-cause mortality and hospitalizations in patients with heart failure. Am J Cardiol 115(8):1111–1115. doi:10.1016/j.amjcard.2015.01.545
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J 51(1):171–184. doi:10.1002/bimj.200810488
Kveiborg B, Major-Petersen A, Christiansen B, Torp-Pedersen C (2007) Carvedilol in the treatment of chronic heart failure: lessons from the Carvedilol Or Metoprolol European Trial. Vasc Health Risk Manag 3(1):31–37
Rosenbaum PR (2002) Observational studies, 2nd edn. Springer, Heidelberg
Love TE (2008) Spreadsheet-based sensitivity analysis calculations for matched samples. Center for Health Care Research & Policy. http://www.chrp.org/propensity
Kotecha D, Holmes J, Krum H, Altman DG, Manzano L, Cleland JG, Lip GY, Coats AJ, Andersson B, Kirchhof P, von Lueder TG, Wedel H, Rosano G, Shibata MC, Rigby A, Flather MD, Beta-Blockers in Heart Failure Collaborative G (2014) Efficacy of beta blockers in patients with heart failure plus atrial fibrillation: an individual-patient data meta-analysis. Lancet 384(9961):2235–2243. doi:10.1016/S0140-6736(14)61373-8
Rienstra M, Damman K, Mulder BA, Van Gelder IC, McMurray JJ, Van Veldhuisen DJ (2013) Beta-blockers and outcome in heart failure and atrial fibrillation: a meta-analysis. JACC Heart Fail 1(1):21–28. doi:10.1016/j.jchf.2012.09.002
Dungen HD, Apostolovic S, Inkrot S, Tahirovic E, Topper A, Mehrhof F, Prettin C, Putnikovic B, Neskovic AN, Krotin M, Sakac D, Lainscak M, Edelmann F, Wachter R, Rau T, Eschenhagen T, Doehner W, Anker SD, Waagstein F, Herrmann-Lingen C, Gelbrich G, Dietz R; Investigators C-E; Project Multicentre Trials in the Competence Network Heart F (2011) Titration to target dose of bisoprolol vs. carvedilol in elderly patients with heart failure: the CIBIS-ELD trial. Eur J Heart Fail 13(6):670–680. doi:10.1093/eurjhf/hfr020
Galatius S, Gustafsson F, Atar D, Hildebrandt PR (2004) Tolerability of beta-blocker initiation and titration with bisoprolol and carvedilol in congestive heart failure—a randomized comparison. Cardiology 102(3):160–165. doi:10.1159/000080485
Maack C, Cremers B, Flesch M, Hoper A, Sudkamp M, Bohm M (2000) Different intrinsic activities of bucindolol, carvedilol and metoprolol in human failing myocardium. Br J Pharmacol 130(5):1131–1139. doi:10.1038/sj.bjp.0703400
Maack C, Tyroller S, Schnabel P, Cremers B, Dabew E, Sudkamp M, Bohm M (2001) Characterization of beta(1)-selectivity, adrenoceptor-G(s)-protein interaction and inverse agonism of nebivolol in human myocardium. Br J Pharmacol 132(8):1817–1826. doi:10.1038/sj.bjp.0703992
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding sources
This work was supported from the AOK Baden-Württemberg, Germany, within the scope of the junior researcher’s academy “health care research Baden-Württemberg, Germany”.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All patients gave their written informed consent for data storage and evaluation. The study conformed to the principles outlined in the Declaration of Helsinki and was approved by the local ethics committees. Patients’ data were pseudonymised for analyses.
Rights and permissions
About this article
Cite this article
Fröhlich, H., Torres, L., Täger, T. et al. Bisoprolol compared with carvedilol and metoprolol succinate in the treatment of patients with chronic heart failure. Clin Res Cardiol 106, 711–721 (2017). https://doi.org/10.1007/s00392-017-1115-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1115-0