Abstract
Background
Non-pharmacological treatment programmes are being developed, in which specialised nurses take care of heart failure (HF) patients. Such disease management programmes might increase survival and quality of life in HF patients, but evidence on their cost-effectiveness remains limited.
Methods and results
A prospective economic evaluation piggy-backed onto the randomised controlled Interdisciplinary Network for Heart Failure (INH) Study weighted costs of the intervention HeartNetCare -HF™ (HNC) regarding effectiveness, mortality and quality-adjusted life years (QALYs). To consider uncertainty sensitivity analyses were performed. Compared to usual care (UC), HNC revealed 8,284 € per death avoided within the 6 month study follow-up period. The cost-utility analysis showed additional costs of 49,335 € per QALY.
Conclusion
Although HNC did not reduce short-term re-admission rates of HF patients hospitalised for cardiac decompensation within the first 180 days after discharge, HNC might reduce mortality and increase quality of life in these patients at reasonable costs. Therefore, long-term HNC-effects deserve further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is one of the most common, disabling and cost-intensive diseases. Prevalence estimates of symptomatic HF in the general European population range 1–2 % [1]. The burden of disease and the resources required to manage HF are likely to escalate over the next decade for several reasons, the most important being is the general aging of the population, since incidence of HF increases steeply with age. The prolongation of life span of cardiac patients with hypertension or myocardial infarction by modern and innovative treatments and improvement of HF pharmacotherapy may further increase the incidence and prevalence of HF.
As a leading cause of hospitalisation among patients older than 65 years in western societies, HF results, as a consequence, in a major burden for healthcare systems. About 1–2 % of the total annual health care expenditure is due to the care of HF patients [1]. According to estimates of the Federal Office of Statistics [2], in Germany about 2.7 billion Euros are spent for the treatment of HF. These costs are mainly driven by hospital admissions and are positively correlated with severity of disease [1]. This relation is non-linear and rises almost exponentially as the New York Heart Association (NYHA) class of HF increases.
Against this background, there is increasing need for more efficacious treatment options. Especially, the care of HF patients by a nurse-led approach represents an evolving concept within the German Health Care System [3].
Similar to the rebranded concept of the “medical home”, they seek to improve care for complex patients through better coordination. While this results in some additional upfront costs, the hope is that both future spending and health outcomes will be improved. Information about costs and cost-effectiveness of DMPs remains limited [4]. The objective of the present study was to provide an economic evaluation of the recently published Interdisciplinary Network for Heart Failure (INH) Study [3].
Methods
Study design
The INH study was designed as a randomised controlled trial evaluating the effect (all-cause mortality and all-cause hospitalisation) of a nurse-led HF management programme (HeartNetCare-HF™, HNC) compared to usual care (UC) in patients with systolic HF. The HNC approach consisted of telephone-based monitoring, patient education and collaboration with the patients’ social and medical networks. All activities were coordinated and carried out by specialised nurses. A composite of time to all-cause death or rehospitalisation was the primary end point. Secondary end points were cardiovascular and all-cause death or hospitalisation separately as well as quality of life amongst others. Details regarding the goals and tools of the HNC programme were reported in detail elsewhere [3]. Patients were recruited in nine hospitals in the region of Würzburg, Germany.
A prospective piggy-back cost-effectiveness and cost-utilities analysis of the INH study was incorporated in the INH protocol.
Resource consumption data were collected for the period of 6 months prior to the index hospitalisation, and for a period of 6 months following the index hospitalisation. The case record form (CRF) included demographic and clinical patient characteristics and health-care resources like drugs, hospitalisations because of HF, cardiac or non-cardiac causes, outpatient care, home or child care, in-patient care, home support, emergency admissions, rehabilitation leaves as well as sickness certification, temporary and permanent productivity loss.
Study sample
The target population included patients aged > 18 years with signs and symptoms of decompensated HF, who had a left ventricular ejection fraction (LVEF) < 40 % (echocardiography) at random assignment at the time of discharge from hospital.
All patients provided informed consent prior to study participation. New-onset structural heart disease, logistic or health reasons precluding participation in telephone-based interventions, and lack of written consent were defined as exclusion criteria. Mentally or physically disabled patients were eligible if family assistance to follow the protocol was available.
Economic analysis
Costs
The economic evaluation was performed from a societal perspective. All costs were adjusted to 2007 Euros. The index hospitalisation was not included in the costs of managing the two groups. The costing of the resource use with regard to outpatient contacts was based on the German recommendations of Krauth et al. 18.80 € per general practitioner visit; 67.03 € per cardiologist visit; 49.24 € per other specialist visit [5]. German market values were used for drugs.
To calculate inpatient costs, we applied different methods depending on the cause of hospitalisation. With regard to HF, unit costs for hospitalisation were estimated by applying the weighted mean price of the respective diagnosis related groups (DRG) (F62A, F62B, F62C) for that hospitalisation, using cost data from the German Institute for the Hospital Remuneration System (InEK). With regard to the length of hospitalisation regarding HF, the following costs were included: 2,074.39 € (≤4 days); 3,513.30 € (4 < x ≤ 17 days); 5,175.18 € (≥18 days). Costs of hospitalisations because of other cardiac reasons or non-cardiac reasons were estimated using the recommendations of Krauth et al. (356.63 € per cardiac hospitalisation day and 477.55 € per hospitalisation day because of other reasons). Rehabilitation costs were also derived from Krauth et al. (118.25 € per rehabilitation day because of other reasons, 112.50 € per rehabilitation day concerning the heart failure) [5].
Programme costs were included with an average of 50 € per study participant and month. Costs for inpatient long-term care were derived from requirements of compulsory long-term care insurance. Outpatient long-term care costs were estimated by an empirical study (Federal Office of Statistics) [2]. The time spent for home or child care was determined as 7.66 € per hour according to patient statement of costs charged to the statutory health insurance. Unit costs for emergency contact were obtained from the Red Cross (545.50 €). Working day losses as well as permanent and partially productivity losses were evaluated using the friction cost approach.
Cost-effectiveness
The clinical outcome, on which cost-effectiveness analysis was based, was all-cause mortality. All-cause mortality was calculated using the rate of mortality per group. The primary measurement of a cost-effectiveness analysis is the incremental cost-effectiveness ratio (ICER), which is defined as the difference between the costs of the intervention and usual care divided by the difference between the rate of mortality of HNC and UC.
Cost-utility
Using a common metric of health effects, quality-adjusted life years (QALY) allows comparing ICERs of interventions across different interventions and diseases. QALYs were calculated by integrating utilities (weights measured on a scale from 0 to 1, where 0 reflects death and 1 reflects perfect health) over time. In this analysis, the German tariff for EQ-5D mapping to utility was used.
Health-related quality of life in both groups (HNC and UC) was evaluated with the EuroQol questionnaire (EQ-5D), a standardised self-administered instrument that measures health outcome via five dimensions: mobility, self care, usual activities, pain/discomfort and anxiety/depression. The incremental cost-utility ratio (ICUR) was calculated by dividing the difference in costs by the difference in QALY obtained in the two groups.
Sensitivity analysis
The sensitivity analysis was performed by recalculation of the cost-effectiveness and cost-utility ratio using a non-parametric bootstrapping.
Statistical analysis
Descriptive statistics are presented as mean ± standard deviation. Mean values of the two groups were compared with Chi- [2] and t-test, respectively, as applicable. A probability value of ≤0.05 was considered statistically significant. Data were analysed using IBM PASW Statistics 17.
Results
Between 1 March 2004, and 31 August 2007, a total of 715 patients were randomised to HNC or UC. Baseline characteristics did not show significant differences between the two groups, except of a slightly higher age in the UC group (Table 1). In the total cohort, 53 % of patients were 70 years or older. Only few patients were in the NYHA functional classes I (2 %) and IV (4 %) at the time of discharge from hospital. The majority of patients were in NYHA class II (58 %) and III (36 %). For more details of the study design, patient characteristics and outcome see Angermann et al. 2012 [3].
Clinical outcomes
During the first 180 days of the trial there was no statistically significant difference between the HNC and the UC group regarding the combined primary endpoint of all-cause mortality and/or all-cause hospitalisation (37 % HNC vs. 38 % UC; p = 0.74). The frequency of rehospitalisation was similar in both study groups (34 vs. 31 %, p = 0.28). However, HNC was associated with a reduction in the risk of all-cause death (uncensored data 9 vs. 14 %, p = 0.03).
Quality of life assessment with EQ-5D showed that there were significant differences in the accumulation of QALYs between the two groups, favouring the HNC group. The mean values of QALYs after 6 months were 0.385 in the HNC and 0.363 in the UC group (p = 0.02).
Costs
General practitioner (GP) visits and hospitalisations were the most frequent health care services used by patients in both groups (Table 2). The most expensive health care service used was hospitalisation with overall costs of 2,355 € per person in the HNC and 2,200 € in the UC group. With regard to other resource utilisation such as GP visits, rehabilitation or informal care, there was no difference between the two groups with the exception of more frequent visits of specialist in the usual care group. The overall costs per person were 3,535 € in the HNC and 3,038 € in the UC group.
Cost-effectiveness analysis
The difference in mean costs per patient between the two groups amounted to 497 €. The ratio between the difference in costs and the difference in all-cause mortality was 8,284 € per death avoided.
Cost-utility analysis
The difference of mean costs per patient between the two groups for a period of 180 days amounted to 497 €. Over the same time period the HNC group accumulated 0.385 QALY as compared to 0.363 QALY in the UC group. The ratio between the difference in costs and the difference in QALY was 49,335 € per QALY gained.
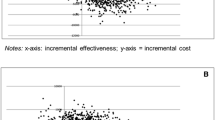
Sensitivity analysis
To account for the uncertainty bootstrapping was done (Figs. 1, 2). According to this analysis, the cost/effectiveness ratio amounted to 8,398 € per death avoided, and the cost/utility ratio was 51,692 € per QALY. The cost-effectiveness acceptability curve shows that the DMP HeartNetCare HF™ had a probability of between 55 and 90 % of being cost-effective from a societal perspective (Fig. 3).
Discussion
The INH study investigated the effects of a structured collaborative-nurse-coordinated disease management programme compared to UC in the first 180 days after discharge from hospital after a cardiac decompensation. While there was no difference in the primary composite endpoint of rehospitalisation or mortality, mortality was significantly lower in the HNC group, which suggests that the HNC intervention facilitated a patient-relevant improvement in this post discharge phase, in which compared with stable individuals patients are at a greatly increased risk of either death or rehospitalisation [6].
Rehospitalisation was previously reported to predict adverse prognosis. Regarding our study, we rather assume that the numerically slightly higher total re-admission rate in the intervention group may reflect better awareness of imminent cardiac decompensation in patients and caregivers [3]. Previous DMP trials did not show consistent results but indicated that some programmes might be efficacious [7–10]. However, there is a lack of information with regard to the economic aspects of these programmes, with only few studies considering their costs or cost-effectiveness [7, 8]. A systematic review on costs and cost-effectiveness of HF nurses in the management of patients with heart failure reports incremental cost-effectiveness ratios of 490 € up to cost savings of 7,330 € per prevented rehospitalisation [11]. Most of the studies identified in this review only focused on direct costs, specifically on costs for rehospitalisation, and failed to include or report indirect costs separately.
In this study, we conducted a cost-effectiveness and cost-utility of the nurse-led collaborative DMP HeartNetCare HF™, estimating additional costs of 8,284 € per death avoided and additional costs of 49,335 € per QALY gained. To our knowledge, this is the first time economic evaluation of a nurse-led programme performed in a large representative study population in Germany that considers both, direct and indirect costs related to HF in the vulnerable early post-discharge period. There is no fix threshold for Germany. Regarding to other health systems 50,000 € per QALY is a very high threshold in case of reimbursement.
Limitations of the present analysis include the short observation period of 6 months, which precludes conclusions about the long-term cost-effectiveness of the intervention in the chronic, more stable patient.
Furthermore, external validity may be reduced due to the use of the randomised controlled trial efficacy data to calculate the cost-effectiveness. Costs of death may be underestimated given sparse information on the resource use during the last days of life which is usually accompanied with high cost.
Due to demographic changes in most industrialised countries, a tremendous increase in the number of patients with HF has to be suspected [1]. Along with these demographic alterations there will be an increase of costs for the treatment of patients suffering from HF. There is a need to develop new innovative programmes to better manage patients with HF and to implement these in clinical practice. The standardised collaborative nurse-led HNC intervention shows clinical efficacy and seems to be cost-effective even when compared to other interventions in cardiology, as cardioverter defibrillators or cardiac resynchronisation therapy [12]. Further studies need to be performed to evaluate the effectiveness in the real world setting and over a longer term period.
Conclusion
Although prior evaluations of the efficacy of different HF management programmes exist, information about the cost-effectiveness of these programmes in the early post-discharge period remains scarce. The present study provides information about the short-term cost-effectiveness and cost-utility of a nurse-based HF management programme compared to usual care.
The results indicate that the implementation of a nurse-based HF management programme will cost 8,284 € per death avoided and additional 49,335 € per QALY gained within the first 180 days post-discharge. Considering short-term results, the programme appears to be cost-effective regarding death avoiding, even if it is compared to other technologies in cardiology.
References
Neumann T, Biermann J, Neumann A, Wasem J, Ertl G, Dietz R et al (2009) Herzinsuffizienz: Häufigster Grund für Krankenhausaufenthalte, Medizinische und ökonomische Aspekte [Heart Failure: The most common reason for hospitalization, medical and economic aspects]. Deutsches Ärzteblatt International 106(16):269–275
Federal Office of Statistics Germany (2004) Krankheitskostenrechnung für Deutschland. https://www.destatis.de/DE/Publikationen/WirtschaftStatistik/Gesundheitswesen/Krankheitskosten.pdf?__blob=publicationFile. Accessed 5 September 2012
Angermann CE, Störk S, Gelbrich G, Faller H, Jahns R, Frantz S et al (2012) Mode of action and effects of standardized collaborative disease management on mortality and morbidity in patients with systolic heart failure: The Interdisciplinary Network for Heart Failure (INH) Study. Circ Heart Fail 5(1):25–35
Göhler A, Conrads-Frank A, Worrell SS, Geisler BP, Halpern EF, Dietz R et al (2008) Decision-analytic evaluation of the clinical effectiveness and cost-effectiveness of management programmes in chronic heart failure. Eur J Heart Fail 10(10):1026–1032
Krauth C, Hessel F, Hansmeier T, Wasem J, Seitz R, Schweikert B (2005) Empirical standard costs for health economic evaluation in Germany—a proposal by the working group methods in health economic evaluation. Gesundheitswesen 67(10):736–746
Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB et al (2007) Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 116(13):1482–1487
Capomolla S, Febo O, Ceresa M, Caporotondi A, Guazzotti G, La Rovere M et al (2002) Cost/utility ratio in chronic heart failure: comparison between heart failure management programme delivered by day-hospital and usual care. J Am Coll Cardiol 40(7):1259–1266
Del Sindaco D, Pulignano G, Minardi G, Apostoli A, Guerrieri L, Rotoloni M et al (2007) Two-year outcome of a prospective, controlled study of a disease management programme for elderly patients with heart failure. J Cardiovasc Med 8(5):324–329
Koelling TM, Johnson ML, Cody RJ, Aaronson KD (2005) Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation 111(2):179–185
Kimmelstiel C, Levine D, Perry K, Patel AR, Sadaniantz A, Gorham N et al (2004) Randomized, controlled evaluation of short- and long-term benefits of heart failure disease management within a diverse provider network: The SPAN-HF Trial. Circulation 110(11):1450–1455
Biermann J, Mostardt S, Neumann T, Erbel R, Wasem J, Neumann A (2010) Cost-Effectiveness of study nurses in the management of patients with heart failure. A systematic review. Herz 35(4):273–283
Sanders GD, Hlatky MA, Owens DK (2005) Cost-effectiveness of implantable cardioverter-defibrillators. N Engl J Med 353(14):1471–1480
Acknowledgments
This work was supported by the Competence Network of Heart Failure funded by the Federal Ministry of Education and Research (BMBF) [01GI0205/23].
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Neumann, S. Mostardt, C. E. Angermann and J. Wasem contributed equally to the study.
Rights and permissions
About this article
Cite this article
Neumann, A., Mostardt, S., Biermann, J. et al. Cost-effectiveness and cost-utility of a structured collaborative disease management in the Interdisciplinary Network for Heart Failure (INH) study. Clin Res Cardiol 104, 304–309 (2015). https://doi.org/10.1007/s00392-014-0781-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0781-4