Abstract
The objective of this work was to assess the predictive value of pre-procedural N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels in patients undergoing atrial fibrillation (AF) ablation. Seventy-three consecutive patients with AF (paroxysmal n = 49, persistent n = 24) and preserved left ventricular (LV) systolic function (LV ejection fraction > 45%) were prospectively enrolled in this study. All of the enrolled patients underwent catheter ablation after a measurement of their plasma NT-proBNP levels, and an echocardiographic examination with assessment of their LV diastolic function and left atrial(LA) volume. Patients with AF recurrence at 3 months had more persistent AF (P = 0.001), a higher LA volume index (P = 0.002), lesser decelerating times (DT) of mitral inflow (P = 0.014), and higher NT-proBNP levels (P < 0.001), when compared with patients with sinus rhythm restoration. The baseline log NT-proBNP correlated significantly with age (r = 0.26, P = 0.025), LA volume index (r = 0.41, P = 0.001), E/E’ (r = 0.34, P = 0.007), DT (r = −0.34, P = 0.007), and E (r = 0.25, P = 0.04). The log NT-proBNP (HR 7.76, 95% CI 2.95–20.39, P < 0.001) was an independent predictor of AF recurrence. The measurement of NT-proBNP added incremental predictive value to standard indexes of LA size or diastolic function, including LA volume index and DT (P = 0.02). This study suggests the clinical utility of the level of NT-proBNP as an integrating marker of various risk factors, and as an incremental predictive marker for AF catheter ablation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Levels of plasma B-type natriuretic peptide (BNP) and its inactive, more stable pro-hormone amino-terminal fragment N-terminal pro-B-type natriuretic peptide (NT-proBNP) have been used to detect various cardiac conditions and to evaluate patient’s hemodynamic status [1]. Recently, some studies have indicated that these peptides are elevated in patients with atrial fibrillation (AF) and preserved left ventricular (LV) systolic function [4, 15]. The increased atrial stretch associated with increased left atrial (LA) volume can be responsible for the elevated levels of plasma BNP, because BNP is released primarily from the atria [7]. Increased wall stress by the diastolic dysfunction itself that frequently coexists with AF may also induce the release of BNP from the ventricle [8, 18]. Such complex and various mechanism regarding to BNP release may make its levels heterogeneous among individuals with AF, consequently making its clinical role unclear. In patients with old age, LA enlargement, and persistent AF among those with AF, BNP levels have been known to be more elevated [15]. On the other hand, these are concurrently well-known risk factors of recurrent AF after catheter ablation [2, 11]. Thus, we hypothesized that pre-procedural elevated NT-proBNP levels may be associated with short-term recurrence after catheter ablation. We also evaluated the predictive value of NT-proBNP levels, and compared it with other established risk factors.
Methods
Study population
Seventy-three patients with symptomatic paroxysmal or persistent AF and drug-refractory AF episodes were included in this study. Exclusion criteria were intracardiac thrombi, left ventricular (LV) ejection fraction (EF) < 45% or right ventricular pressure >35 mmHg on an echocardiogram, renal failure, or a history of myocardial infarction or cardiac surgery.
Study protocol
All of the patients provided written informed consent for their participation. All anti-arrhythmic medications except for amiodarone were discontinued 4–5 half-lives prior to the blood sampling. Blood samples were taken from a peripheral vein to evaluate the plasma concentrations of NT-proBNP at least 12 h before the procedure, and the echocardiographic examination was performed 1 day before the procedure.
Catheter ablation procedures were carried out for the treatment of AF. Afterwards, all of the enrolled patients were scheduled for repeated visits in an outpatient clinic at 1, 2, and 3 months after the ablation. At each of these visits, the patients underwent intensive questioning for arrhythmia-related symptoms (palpitations, chest discomfort, dizziness, and nausea) since the last follow-up visit and a 12 lead electrocardiogram was also performed. One-day holter monitoring was performed each time arrhythmia-related symptoms were reported, and at 3 months for all of the patients. Freedom from AF recurrence was defined as no detected episodes of AF beyond 1 month after the initial procedure, because an early recurrence of AF within several weeks after the ablation may be transient.
Echocardiographic evaluation
Two-dimensional echocardiograms were performed in the parasternal long- and short-axis views and apical 4- and 2-chamber views before AF ablation. Standard two-dimensional measurements (LV end- diastolic and end-systolic dimensions, ventricular septal and posterior wall thickness) were obtained with M-mode quantification [9]. The LV EF was calculated by the modified Quinones method [12]. The LA volume index was measured by the prolate ellipsoidal method [9]. The LV mass index was calculated by dividing the LV mass by the body surface area [6]. Pulsed Doppler velocity recordings were obtained from a 4 × 4-mm sample volume placed at the tips of the mitral leaflets to derive the following measurements: peak velocity of the early diastolic transmitral flow (E), and deceleration time (DT). Tissue Doppler imaging of the septal annulus motion was undertaken to measure the early diastolic velocity (E′). The severity of mitral regurgitation (MR) was evaluated by MR jet area by planimetry [5]. For the evaluation of irregular rhythms at the time of echocardiographic study, ten consecutive cardiac cycles were recorded for the Doppler echocardiographic assessment and the results from 5 cardiac cycles, excluding the longest and shortest cardiac cycles, were averaged.
NT-proBNP assays
Blood samples for NT-proBNP analysis were drawn from a peripheral vein immediately before the AF ablation, centrifuged at 4°C, and analyzed within 4 h of sampling. The plasma was then analyzed in triplicate by an electrochemiluminescence immunoassay method to evaluate the NT-proBNP level (Elecsys proBNP, Roche Diagnostics, Basel, Switzerland).
Ablation procedure
Thirty-three patients (45%) underwent segmental pulmonary vein (PV) isolation, and the remaining 40 (55%) underwent circumferential PV isolation as previously described [16]. All catheters were introduced through a femoral vein. A steerable quadripolar 6F electrode catheter was placed in the coronary sinus, and a non-steerable quadripolar catheter was placed in the right ventricular apex. The LA was approached by a standard transseptal puncture using a Brockenbrough needle and a Preface sheath.
For the segmental PV isolation, a circular, steerable, decapolar mapping catheter (Lasso, Biosense Webster, Inc) was inserted. After the PV was entered, the circular mapping catheter was positioned as close to the PV ostium as possible. PV isolation was performed by applying a radiofrequency current at the ostial sites showing the earliest bipolar PV potentials during sinus or paced rhythms, as previously described. Disappearance or dissociation of the distal local pulmonary vein potential during a sinus or paced rhythm throughout the ostial circumference was considered the criterion for effective electric isolation of the PV from the left atrium. For circumferential PV isolation, continuous circumferential lesions that encircled the right and left PV ostia, guided by the NavX system using a 4-mm-tip ablation catheter (EP Technologies, Boston Scientific, Inc.), were created. Ablation lines consisted of contiguous focal lesions deployed at a distance 1.5–2 mm from the PV ostia. An additional linear ablation of the cavotricuspid isthmus was created with the achievement of a bidirectional isthmus conduction block to prevent the occurrence of typical atrial flutter after AF ablation. When there were any PV potentials within the PVs, PV isolation was performed as previously described [16].
Statistical analyses
All continuous data are presented as the mean ± SD, and categorical variables are presented as proportions. For group comparisons, we used the Student t test or Mann–Whitney U test for continuous variables and the chi-square test or the Fisher exact test for categorical variables. The NT-proBNP levels are summarized with the median and inter-quartile range (IQR). The logarithmic transformation of NT-proBNP levels was performed to assess their correlation with the echocardiographic indexes and for Cox regression analysis. Associations between the log NT-proBNP and the echocardiographic and clinical indexes were assessed by Pearson’s correlation. Estimations of risk were performed using the Cox proportional hazard models by univariate and multivariate analysis. The incremental value of the NT-proBNP levels over the clinical data, LA size, and transmitral inflow variables was assessed in three modeling steps in the same order as in clinical practice. The first step consisted of clinical data and LA size that were used as the baseline risk factors. The transmitral inflow variable was then added in the next block. In the final step, the NT-proBNP variable was added. A value of P < 0.05 was considered statistically significant.
Results
Radiofrequency catheter ablation of AF was performed in all 73 patients. Patients had a mean age of 52 years (range, 30–72). Paroxysmal AF was seen in 49 patients (67.1%) and persistent AF in 24 patients (32.9%). The mean AF duration was 5.1 years in all of the patients. No complications occurred in any of the patients during either the procedure or the follow-up. During the 3 months follow-up after the ablation procedure, AF recurred in 20 (27.4%) patients. Baseline characteristics of the study population are described in Table 1. There was no significant difference in age, sex, duration of disease, body mass index, hypertension, diabetes, alcohol, or previous coronary disease between the patients with sinus rhythm (SR) restoration and those with AF recurrence. Patients with AF recurrence had more persistent AF (14% Vs. 86%, P = 0.001), a higher LA volume index (38.2 ± 11.2 Vs. 29.3 ± 9.7 ml/m2, P = 0.002), lesser DT (162.7 ± 21.4 Vs. 195.5 ± 35.1 ms, P = 0.014), and higher NT-proBNP levels (602.2, IQR 293.0–770.3 Vs. 122.6, IQR 37.0–222.9 pg/ml, P < 0.001) compared to patients with SR restoration. There were no statistical differences in LV end-diastolic dimension, LV end-systolic dimension, LV EF, E′, or E/E′ (all P value > 0.05) between patients in the two groups.
Determinants of plasma NT-proBNP levels
Log NT-proBNP was significantly correlated with age (r = 0.26, P = 0.025), LA AP diameter (r = 0.32, P = 0.007), LA volume index (r = 0.41, P = 0.001), E/E’(r = 0.34, P = 0.007), and E (r = 0.25, P = 0.04) (Table 2). There was an inverse correlation between log NT-proBNP and DT (r = −0.34, P = 0.007). Patients with persistent AF had higher levels of NT-proBNP compared with patients who presented with paroxysmal AF (494.3, IQR 155.7–728.3 Vs. 111.7 pg/ml, IQR 37–111.7, P = 0.001). However, the LV end-systolic dimension, LV end-diastolic dimension, EF, LV mass index, E, and E’ were not correlated with log NT-proBNP (all P values > 0.05).
Univariate and multivariate analyses of AF recurrence
Univariate analysis results for AF recurrence during the 3 month follow-up are shown in Table 3. The variables significantly associated with AF recurrence included sex, persistent AF, LA volume index, decelerating time, and log NT-proBNP. In the multivariate Cox regression, forward stepwise analysis adjusted by age, sex, persistent AF, LA volume index, DT, and log NT-proBNP indicated that log NT-pro BNP was an independent predictor of recurrence at 3 months (hazard ratio 7.76, 95% confidence interval 2.95–20.39, P < 0.001) (Table 3).
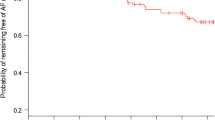
The incremental value of NT-proBNP is shown in Fig. 1. DT has a tendency to improve the prognostic value of a model containing age, sex, persistent AF, and LA volume index, but not statistically significant (P = 0.07). NT-proBNP levels significantly improved the outcome of a model that contained clinical risk factors, LA volume index and DT (P = 0.02).
Incremental value of NT-proBNP and decelerating time (DT) in predicting short-term recurrence. The addition of DT and NT-proBNP resulted in incremental improvements in the predictive value of a model including other established risk factors (age, sex, persistent AF, and LA size): chi-square = 25.1, df = 4 for other established risk factors; chi-square = 26.1, df = 1 for other established risk factors plus DT; and chi-square = 29.5, df = 1 for other established risk factors plus DT plus log NT-proBNP
Predictive value of NT-proBNP
The ability of NT-proBNP to detect AF recurrence was assessed with ROC curve (Fig. 2). The Area Under Curve for the ROC curve with NT proBNP used to detect AF recurrence was 0.88 (95% CI, 0.805–0.958, P < 0.001). When using a NT proBNP cutoff of 220 pg/ml, NT proBNP value >220 pg/ml had a sensitivity of 80%, a specificity of 75.5%, a positive predictive value of 55.2%, and a negative predictive value 90.9% for predicting AF recurrence.
Discussion
Many studies have investigated the role of BNP and its inactive form, NT-proBNP, as surrogate markers of LV systolic dysfunction, LV diastolic dysfunction, and MR severity [1, 17]. Recently, it was shown that these peptides are increased in patients with AF compared with controls [4, 15].
In our study, we demonstrated that the baseline level of NT-proBNP before ablation could also predict a successful outcome after ablation. To the best of our knowledge, this is the first report in which pre-procedural NT-proBNP levels were used to predict the short-term outcomes after AF ablation. Our results showed that NT-proBNP levels correlated to the LA volume index, E, DT, and E/E′, parameters of diastolic function, and age, as recent studies have suggested [10]. Furthermore, the NT-proBNP levels were higher in persistent AF than in paroxysmal AF [15, 19]. Interestingly, age, LA size, and persistent AF are well-known risk factors of AF recurrence after AF ablation [2, 11]. Moreover, diastolic dysfunction is known to be associated with an increased incidence of AF [17, 18], although the relationship between AF recurrence after AF ablation and these parameters was not investigated prior to this study.
The secretion and clearance of BNP or NT-proBNP is complex and incompletely characterized. Increased atrial stretch, which is associated with increased LA volume, is known to be responsible for elevated levels of plasma BNP, because BNP is released primarily from the atria especially in the non-failing heart [7]. In addition, increased LV diastolic wall stress caused by diastolic dysfunction can possibly induce BNP secretion from the ventricle [8]. Some reported that plasma BNP concentrations have been shown to decrease after successful cardioversion or ablation, and a reduction in BNP level after the procedure was related to good outcome [3, 14, 20]. However, we cannot know whether diastolic dysfunction cause AF relapse and sequentially small decrease of BNP levels, or only AF burden itself cause an elevation of BNP. Our study suggest that diastolic dysfunction may also trigger and perpetuate AF after ablation, although it may have a small effect on recurrence compared with other factors such as LA size, or age. The relationship of NT-proBNP levels to these factors may also explain why elevated NT-proBNP levels are such a powerful independent predictor of AF recurrence after AF ablation. AF recurrence in the current study indicated just beyond 4 weeks. We excluded early recurrence within 4 weeks as a definition of AF recurrence in order to mainly focus on hemodynamic or structural aspect as its cause” because early recurrence may be due to incomplete PV isolation or to recovery of conduction in a previously isolated PV.
NT-proBNP levels seem to act as a global index of hemodynamic status, cardiac structure reflecting LA volume and diastolic function, and AF type, which are well known risk factors of AF recurrence after ablation. It is possible that a still-enlarged LA or diastolic dysfunction at a time early after the ablation, even though electrical isolation was complete, would trigger or stabilize AF initiated by another cause, because reverse structural remodeling of the LA, and improvement of the LV diastolic and systolic functions would develop slowly after restoration of a sinus rhythm by AF ablation [13]. Accordingly, we are not convinced that elevated NT-proBNP levels can be associated with long-term outcomes after AF ablation in addition to their association with short-term outcomes. Despite this limitation, this study shows that the measurement of NT-proBNP levels is helpful in predicting short-term outcomes after ablation, adding incremental predictive data to clinical factors and echocadiographic parameters.
Several limitations of our study must be acknowledged. Heart rhythm at the time of baseline blood sampling was not recorded, although the patients were asymptomatic at the time of baseline blood sampling. We did not measure NT-proBNP levels after ablation, although recent studies demonstrate a change in the BNP level as a powerful predictor of a successful outcome. We did not demonstrate the superiority of a baseline NT-proBNP as a predictor over a change in its concentration [3, 20]. In addition, we did not perform echocardiography after ablation which could have been used to demonstrate whether or not patients with high concentrations of NT-proBNP at baseline still had an enlarged LA size or diastolic dysfunction even after ablation. In this study, AF free survival rate might have been overestimated because only intermittent 24 h holter recordings and interviews might miss asymptmatic AF recurrence for the clinical follow-up.
In conclusion, this current study shows that pre-procedural NT-proBNP levels are helpful for predicting short-term recurrences as an integrating marker for other established risk factors, and that it has incremental predictive value in patients undergoing AF ablation.
References
Anand IS, Fisher LD, Chiang YT, Latini R et al (2003) Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation 107:1278–1283
Berruezo A, Tamborero D, Mont L et al (2007) Pre-procedural predictors of atrial fibrillation recurrence after circumferential pulmonary vein ablation. Eur Heart J 28:836–841
Date T, Yamane T, Inada K et al (2006) Plasma brain natriuretic peptide concentrations in patients undergoing pulmonary vein isolation. Heart (Br Cardiac Soc) 92:1623–1627
Ellinor PT, Low AF, Patton KK et al (2005) Discordant atrial natriuretic peptide and brain natriuretic peptide levels in lone atrial fibrillation. JACC 45:82–86
Enriquez-Sarano M, Bailey KR, Seward JB et al (1993) Quantitative Doppler assessment of valvular regurgitation. Circulation 87:841–848
Hense HW, Gneiting B, Muscholl M et al (1998) The associations of body size and body composition with left ventricular mass: impacts for indexation in adults. JACC 32:451–457
Inoue S, Murakami Y, Sano K et al (2000) Atrium as a source of brain natriuretic polypeptide in patients with atrial fibrillation. J Cardiac Fail 6:92–96
Iwanaga Y, Nishi I, Furuichi S et al (2006) B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. JACC 47:742–748
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Lee SH, Jung JH, Choi SH et al (2006) Determinants of brain natriuretic peptide levels in patients with lone atrial fibrillation. Circ J 70:100–104
Oral H, Knight BP, Tada H et al (2002) Pulmonary vein isolation for paroxysmal and persistent atrial fibrillation. Circulation 105:1077–1081
Quinones MA, Waggoner AD, Reduto LA (1981) A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation 64:744–753
Reant P, Lafitte S, Jais P et al (2005) Reverse remodeling of the left cardiac chambers after catheter ablation after 1 year in a series of patients with isolated atrial fibrillation. Circulation 112:2896–2903
Shin DI, Jaekel K, Schley P et al (2005) Plasma levels of NT-pro-BNP in patients with atrial fibrillation before and after electrical cardioversion. Zeitschrift fur Kardiologie 94:795–800
Silvet H, Young-Xu Y, Walleigh D et al (2003) Brain natriuretic peptide is elevated in outpatients with atrial fibrillation. Am J Cardiol 92:1124–1127
Tada H, Kurosaki K, Ito S et al (2005) Left atrial and pulmonary vein ostial ablation as a new treatment for curing persistent atrial fibrillation. Circ J 69:1057–1063
Troughton RW, Prior DL, Pereira JJ et al (2004) Plasma b-type natriuretic peptide levels in systolic heart failure: importance of left ventricular diastolic function and right ventricular systolic function. JACC 43:416–422
Tsang TS, Gersh BJ, Appleton CP et al (2002) Left ventricular diastolic dysfunction as a predictor of the first diagnosed nonvalvular atrial fibrillation in 840 elderly men and women. JACC 40:1636–1644
Tsuchida K, Tanabe K (2004) Influence of paroxysmal atrial fibrillation attack on brain natriuretic peptide secretion. J Cardiol 44:1–11
Yamada T, Murakami Y, Okada T et al (2006) Plasma atrial natriuretic peptide and brain natriuretic peptide levels after radiofrequency catheter ablation of atrial fibrillation. Am J Cardiol 97:1741–1744
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Hwang and Dr. Son contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hwang, H.J., Son, J.W., Nam, BH. et al. Incremental predictive value of pre-procedural N-terminal pro-B-type natriuretic peptide for short-term recurrence in atrial fibrillation ablation. Clin Res Cardiol 98, 213–218 (2009). https://doi.org/10.1007/s00392-009-0744-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-009-0744-3