Abstract
Background
In a previous report, acute mitral regurgitation (MR) was found to indicate the more severe end of the spectrum of Takotsubo cardiomyopathy (TC). The aim of this study was to determine the incidence and clinical significance of acute MR in TC.
Methods
Early (<24 h of presentation) left ventricular (LV) angiograms of 47 patients with TC were reviewed by two blinded reviewers. MR severity was graded on a four graded scale. MR ≥ grade 2 was considered significant.
Results
Significant MR was present in nine (19%) patients. MR was severe (grade 3 or 4) in four and moderate (grade 2) in five. LV outflow tract gradients were not observed in any of these patients. Patients with and without significant MR did not differ with regard to various clinical parameters, including age, gender, type of TC, cardiovascular risk factors, presenting ECG, level of troponin I, triggering factors, ejection fraction (EF), vasopressor therapy, pulmonary edema, and survival to discharge. When patients were grouped according to the presence or absence of pulmonary edema, the only significant difference between the two groups was EF which was significantly lower in patients with pulmonary edema (40 ± 12% vs. 50 ± 12%, P = 0.011).
Conclusions
Acute MR is a noteworthy finding in TC, but it is not associated with the severity of TC. Dysfunction of mid-ventricular myocardium seems to be a conditio sine qua non, whereas LVOT obstruction does not seem to play an important role.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Functional mitral regurgitation (MR) is a known complication of Takotsubo cardiomyopathy (TC) [1, 2]. Until recently, however, no data on the incidence and clinical significance of acute MR in TC were available. In a recent publication, Parodi et al. [3] demonstrated that significant MR (defined as moderate-to-severe or severe MR by echocardiography) was present in 14 of 68 patients (21%). They also found that patients with significant MR presented more often in Killip class III or IV, showed more severe impairment of left ventricular (LV) function, required more frequent treatment with an intra-aortic balloon pump, and had more often systolic anterior movement (SAM) of the mitral valve. In that study, significant MR was the only predictor of Killip class III or IV at presentation.
In the present study, we assessed the prevalence and clinical significance of MR in a cohort of consecutive patients over a 42-month period.
Methods
Study population
Between November 2004 and December 2007, 60 patients (53 women; mean age 68 ± 12 years) with a clinical diagnosis of TC were prospectively entered into a database at our institution. Of these, 47 patients had left ventriculography performed within 24 h of presentation and constituted the study population. Diagnosis of TC was based on the following criteria: (1) acute onset of LV wall-motion abnormalities not confined to the vascular territory of a single major coronary artery; (2) improvement of wall-motion abnormalities within a few days of initial diagnosis; and (3) exclusion of ischemic myocardial stunning by coronary angiography. Classical TC was defined as TC with the involvement of the LV apex, whereas variant TC denoted a subgroup of patients in whom the LV apex was spared [2, 4, 5].
Clinical assessment
Clinical examination, laboratory tests, 12-lead ECGs, chest X-rays, and serial echocardiograms were performed according to the standard protocol for the management of acute coronary syndromes at our institution and as clinically indicated. Chest X-rays were evaluated by different experienced staff radiologists unaware of the fact that their reports will be used for this study.
Review of these data complied with the Declaration of Helsinki and was approved by our institutional review committee.
Left ventriculography and MR grading
Coronary angiography and left ventriculography were performed by standard techniques. Left ventriculography was performed in a 30° right anterior oblique projection in 10 patients and 30° right and 60° left anterior oblique projections in 37 patients, with injection of 36 ml of contrast through a pigtail catheter in the central LV cavity. The severity of MR was graded according to standard criteria [6] by two experienced interventionalists (DH and TS) who had no knowledge of the patients’ clinical data. Any disagreements were resolved through consensus. Significant MR was defined as MR ≥ grade 2.
Statistical analysis
Continuous variables are expressed as mean ± SD. Continuous variables were compared using the unpaired student t test or Mann–Whitney U test. Categorial variables were compared with the Chi-square test or Fisher exact test. All tests were two-sided. A P value <0.05 was considered statistically significant. All calculations were carried out with the SPSS version 15.0 software package (SPSS Inc., Chicago, IL, USA).
Results
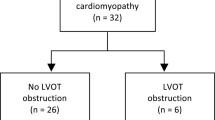
There were 29 patients with classical TC (62%) and 18 patients with variant TC (38%). Mean EF was significantly lower in classical TC compared to variant TC (44 ± 12% vs. 52 ± 11%, P = 0.006). Significant MR, by ventriculography, was present in nine patients (19%; 95% confidence interval [CI] 10–34%). Four patients had severe (grade 3 or 4) and five patients had moderate (grade 2) MR. The clinical features of patients are shown in Table 1. Five of 18 patients (28%; 95% CI 11–54%) with variant TC and 4 of 29 patients (14%; 95% CI 5–33%) with classical TC had significant MR (P = NS) (Fig. 1). Patients with variant TC and significant MR (n = 5) had higher ejection fractions compared to patients with classical TC and significant MR (n = 4), although this difference did not reach the level of significance (54 ± 12% vs. 37 ± 8%; P = 0.065).
There were no significant differences with regard to various clinical variables between patients with (MR+) and those without (MR−) significant MR (Table 1). Vasopressor support was more frequent in MR+ patients, but this difference was not statistically significant (P = 0.08). Importantly, EF did not differ significantly between the two groups (45 ± 12% in MR + vs. 48 ± 12% in MR−, respectively; P = 0.51). Overall, 17 patients (16 with classical TC) had an EF ≤ 40%. Of these patients, only four [(24%), three with classical TC] had significant MR. The prevalence of significant MR among these patients did not differ significantly from patients with ejection fractions >40% (P = 0.7).
All patients underwent transthoracic echocardiography within 48 h of admission. Grading of MR by echocardiography showed good agreement with left ventriculography (Table 2). However, in two patients (patients 1 and 5) agreement was poor. In both patients, echocardiography had been performed rather late after hospitalization, although still within 48 h of admission as required by protocol. MR was found to be functional in all cases. Follow up echocardiography in MR+ patients was performed 47 ± 56 days (range 2–156 days) after presentation and demonstrated resolution of significant MR in all patients.
A significant intraventricular gradient and mitral SAM were present in a single patient in the MR− group but were absent in MR+ patients. None of the patients in the entire study group received dobutamine while in hospital.
Chest X-rays on the day of presentation were performed in all patients. When patients were grouped according to the presence or absence of pulmonary edema, no significant differences with regard to various clinical parameters were observed (Table 3), except for EF which was significantly lower in patients with pulmonary edema (40 ± 12% vs. 50 ± 12%, P = 0.011).
Discussion
The present study supports previous observations by Parodi et al. [3] who found that significant MR is a common phenomenon in TC, occurring in about one-fifth of patients. In contrast to their report, however, we did not find convincing evidence that significant MR indicates the more severe end of the spectrum of TC. Overall, EF was similar between patients with and those without significant MR. A lack of relationship between significant MR and poor systolic LV function is also supported by the observation that of 17 patients with significantly depressed LV function (EF ≤ 40%) only four had significant MR. Most patients with significant MR had ejection fractions >40%.
In the present study, the presence of significant MR had no clinically relevant implications. Prevalence of pulmonary edema, vasopressor therapy and survival to discharge were not significantly different between MR+ and MR− patients.
There might be several reasons behind these observed differences between our study and the previous report by Parodi et al., including differences in patient profiles (classical TC in the study by Parodi et al. vs. classical and variant TC in the present study) and differences in diagnostic methods for the assessment of relevant parameters such as LV function (echocardiography vs. ventriculography), MR severity (echocardiography vs. ventriculography), and pulmonary congestion (auscultation vs. chest X-ray).
The mechanism of acute MR was not specifically addressed in this study. However, the observation that patients with significant MR invariably had involvement of the midventricular segments underlines the pathogenic role of midventricular myocardium in the development of MR. It seems reasonable to assume that dysfunctional and/or displaced papillary muscles are of particular importance. Furthermore, resolution of significant MR could be demonstrated by echocardiography in all patients, indicating the functional nature of MR in TC. It must be noted, however, that in an occasional patient severe MR can also be due to structural abnormalities such as rupture of papillary muscles [7].
Left ventricular outflow tract (LVOT) obstruction does not seem to play a major role in the pathogenesis of MR and was not present in any of our patients with significant MR on catheter pullback. However, this is in contrast to findings by Parodi et al. [3] who reported SAM of the mitral valve and concomitant LVOT obstruction in 5 of their 14 MR+ patients (38%). The overall incidence of LVOT obstruction in our study was lower than in several previous studies from different countries where incidences as high as 25% were reported [8]. However, the incidence of LVOT obstruction among German patients seems to be rather low ranging from 5% in one report [9] to 7% in a large registry of 119 patients [10]. Whether these differences are due to population-based differences in LV size (smaller ventricles will more easily develop LVOT obstruction) or to selection bias or whether they simply constitute a chance effect remains unknown.
Pulmonary edema on chest X-ray was present in 19% of our study patients. Importantly, when patients were grouped according to the presence or absence of pulmonary edema, only EF differed significantly between the two groups, underlining the importance of LV dysfunction rather than MR in the pathogenesis of pulmonary congestion in TC.
Limitations
Limitations of this study include its small sample size, the limited sensitivity and specificity of chest X-ray for the detection of pulmonary edema [11], and inherent limitations of left ventriculography for the assessment of EF (including but not limited to high interobserver variability [12]) as well as for the assessment of MR (including but not limited to its dependency on the amount of injected contrast medium, left-atrial and LV size, and position of the pigtail catheter within the LV cavity). Besides, assessment of EF and MR by left ventriculography can significantly be influenced by premature ventricular beats which cannot always be avoided during catheterization.
Conclusions
In conclusion, acute significant MR is a noteworthy finding in TC. Dysfunction of mid-ventricular myocardium seems to be a conditio sine qua non, whereas LVOT obstruction does not seem to play an important role. However, in contrast to the previous findings, significant MR does not indicate the more severe end of the spectrum of TC and is not associated with the severity of disease in TC.
References
Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K, Umemura T, Nakamura S, Yoshida M, Sato H (2003) Myocardial perfusion and fatty acid metabolism in patients with Tako-tsubo-like left ventricular dysfunction. J Am Coll Cardiol 41(5):743–748
Haghi D, Papavassiliu T, Fluchter S, Kaden JJ, Porner T, Borggrefe M, Suselbeck T (2006) Variant form of the acute apical ballooning syndrome (Takotsubo cardiomyopathy): observations on a novel entity. Heart 92(3):392–394
Parodi G, Del Pace S, Salvadori C, Carrabba N, Olivotto I, Gensini GF (2007) Left ventricular apical ballooning syndrome as a novel cause of acute mitral regurgitation. J Am Coll Cardiol 50(7):647–649
Hurst RT, Askew JW, Reuss CS, Lee RW, Sweeney JP, Fortuin FD, Oh JK, Tajik AJ (2006) Transient midventricular ballooning syndrome: a new variant. J Am Coll Cardiol 48(3):579–583
Shimizu M, Takahashi H, Fukatsu Y, Tatsumi K, Shima T, Miwa Y, Okada T, Fujita M (2003) Reversible left ventricular dysfunction manifesting as hyperkinesis of the basal and the apical areas with akinesis of the mid portion: a case report. J Cardiol 41(6):285–290
Sellers RD, Levy MJ, Amplatz K, Lillehei CW (1964) Left retrograde cardioangiography in acquired cardiac disease: technic, indications and interpretations in 700 cases. Am J Cardiol 14:437–447
Nef HM, Mollmann H, Hilpert P, Masseli F, Troidl C, Rolf A, Dill T, Skwara W, Weber M, Hamm C, Elsasser A (2009) Severe mitral regurgitation in Tako-Tsubo cardiomyopathy. Int J Cardiol 132(2):e77–e79
El Mahmoud R, Mansencal N, Pilliere R, Leyer F, Abbou N, Michaud P, Nallet O, Digne F, Lacombe P, Cattan S, Dubourg O (2008) Prevalence and characteristics of left ventricular outflow tract obstruction in Tako-Tsubo syndrome. Am Heart J 156(3):543–548
Koeth O, Mark B, Kilkowski A, Layer G, Cornelius B, Kouraki K, Bauer T, Zahn R, Senges J, Zeymer U (2008) Clinical, angiographic and cardiovascular magnetic resonance findings in consecutive patients with Takotsubo cardiomyopathy. Clin Res Cardiol 97(9):623–627
Schneider B, Athanasiadis A, Pistner W, Schamberger R, Toepel W, Schoeller R, Bublak A, Gerecke B, Stellbrink C, Gottwald U, Schwab J, Peters K, Stein J, Sechtem U (2007) Clinical spectrum of Tako-Tsubo-cardiomyopathy in a western population: results of the Tako-Tsubo-registry of the Arbeitsgemeinschaft Leitende Kardiologische Krankenkenhausaerzte (ALKK). Circulation 116(Suppl II):338
Michard F (2007) Bedside assessment of extravascular lung water by dilution methods: temptations and pitfalls. Crit Care Med 35(4):1186–1192
Hoffmann R, von Bardeleben S, ten Cate F, Borges AC, Kasprzak J, Firschke C, Lafitte S, Al-Saadi N, Kuntz-Hehner S, Engelhardt M, Becher H, Vanoverschelde JL (2005) Assessment of systolic left ventricular function: a multi-centre comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast-enhanced echocardiography. Eur Heart J 26(6):607–616
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haghi, D., Röhm, S., Suselbeck, T. et al. Incidence and clinical significance of mitral regurgitation in Takotsubo cardiomyopathy. Clin Res Cardiol 99, 93–98 (2010). https://doi.org/10.1007/s00392-009-0078-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-009-0078-1