Abstract
Purpose
To identify the impact of the severity of diverticular disease on long-term quality of life.
Methods
Consecutive patients, hospitalized between October 2009 and November 2015 due to uncomplicated (UD) and complicated diverticulitis (CD) of the left colon, were analyzed. Patients undergoing emergent surgery for perforated disease were excluded. Primary endpoint was health-related quality of life (HrQol), measured by the Short Form 36 questionnaire (SF-36). Physical (PCS) and mental (MCS) compository scores were calculated from SF-36 subscales. To overcome bias, one-to-one propensity score matching and multivariable logistic regression analysis were performed.
Results
Two hundred eighty of the overall 392 patients (Male 138, Female 142; mean age 60.5 years, range 27–91) answered the SF-36 questionnaire. The median follow-up period was 37.8 months (range 15–85). After propensity score matching, each group consisted of 51 patients. Results of the SF-36 questionnaires showed a statistically significant difference, favoring patients with CD in 5 of 8 domains. Also, PCS (56.3 vs. 52.9, p = 0.13) and MCS (53.3 vs. 46.7, p = 0.005) were higher in patients treated for CD. By a multivariate analysis, complicated disease was independently associated with a better scoring on 6 out of 8 SF-36 subscales and on MCS. Treatment strategy (surgery or conservative) did not have any impact on SF-36 subscales, MCS, or PCS on multivariate analysis.
Conclusion
In contrast to complicated disease, the uncomplicated diverticular disease is associated with an impaired long-term quality of life especially in domains composing mental health scores independently of chosen treatment strategy.
Study registration
The study is registered with the Research Registry at June 19, 2019.
Research registry UIN: researchregistry4959.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute left-sided diverticular disease counts among the commonest abdominal emergencies in the western world. US population–based data showed an increasing frequency within the last 30 years. Bharucha et al. found an incidence rate for diverticular disease of 115/100.000 person years between 1980 and 1989, and 188/100.000 during the period from 2000 to 2007 [1]. Of note, about 70% of US citizens above 80 years of age are affected by diverticulosis [2]. In these patients, diverticulitis is the most common indication for sigmoid colectomy [3]. Thereby, the impact of diverticular disease on patients’ wellbeing and health care costs is significant. To date, acute diverticulitis can successfully be treated by conservative therapy (e.g., by antibiotic treatment) in the majority of patients. Therefore, international guidelines recommend a conservative strategy for uncomplicated as well as for most patients with complicated disease [4,5,6,7,8,9]. However, there is ongoing controversial discussion which patient should undergo interval sigmoidectomy. Overall, complicated recurrences after the first episode of acute diverticulitis are rare [10,11,12]. This should be taken into account, if the need for surgery is assessed. Interestingly there are basic differences between both main disease phenotypes: complicated and uncomplicated, i.e., perforating and non-perforating. A growing body of literature suggests that initially non-perforating disease does not develop into a perforating disease. Furthermore, the overall incidence of uncomplicated diverticulitis (UD) is increasing, while the rate of complicated disease (CD) remains stable [13]. Overall, the term “uncomplicated disease” does not seem to fit the characterization of the variety of different disease manifestations. Those patients presenting with an ongoing, chronic disease tend to have a relevantly impaired general wellbeing. Unfortunately, assessment of health-related quality of life (HrQol) in patients, suffering from diverticular disease, plays only a minor role in clinical routine and guideline recommendations.
The aim of the current study was to compare long-term HrQol in patients suffering from uncomplicated and complicated disease.
Material and methods
Ethical approval
The study protocol was in accordance with the Declaration of Helsinki and approved by the medical ethics board of the Bavarian medical council.
Report identification number: 2016-143.
Study cohort
Consecutive patients hospitalized for initial conservative treatment of acute diverticulitis entered the study and were included into the analysis. Patients who underwent emergency surgery for perforated disease, complicated by generalized peritonitis, were excluded.
Primary endpoint
The primary endpoint of the study was HrQol as assessed by the Short Form (SF-36) questionnaire.
Quality of life assessment
Patients were asked to complete the 36-Item Short Form Health Survey (SF-36) which represents a generic questionnaire for the assessment of health-related quality of life, containing 36 items covering eight different domains: general health (GH), physical functioning (PF), social functioning (SF), bodily pain (BP), role physical (RP), mental health (MH), role emotional (RE), and vitality (VT). The SF-36 subscale scores range from 0 to 100, with a higher score indicating better health status. A difference of 10 points is considered to show clinically significant differences, according to the authors of the questionnaire. The 36 scores were grouped to give composite measures of physical health, labeled as physical composite score (PCS) and mental health, labeled as mental composite score (MCS) using German general population as a reference [14]. These were computed as median score with range for comparison. The SF-36 questionnaire was administered through telephone interview.
Intention
The aim of the present study was to determine whether disease phenotype at initial presentation (complicated or uncomplicated diverticular disease) has an impact on individual and composite domains of SF-36.
Classification
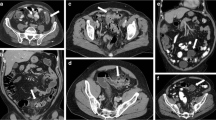
“Complicated diverticular disease” was defined as presence of extraluminal air or abscess at the initial CT-scan.
Statistical analysis
One-to-one propensity score matching was adopted in order to overcome bias arising from lack of randomization as a consequence of the different co-variable distribution among patients who were hospitalized for acute complicated or uncomplicated diverticular disease. The propensity score represents the probability of each patient to present with either disease phenotype. Propensity scores (PS) were generated using the Statistical Package for the Social Sciences version 20 (IBM, Chicago, IL, USA). A multivariable logistic regression analysis was performed, the dependent variable being the diagnosis of complicated diverticular disease, and included all relevant independent variables thought to be potential confounding factors, comprising age, sex, intake of steroids, intake of non-steroidal anti-rheumatic medication (NSAR), intake of acetylsalicylate, surgery for diverticular disease, previous flares of diverticular disease, chronic renal disease, presence of anemia, and history of malignant disease. The “probabilities” option was selected and propensity scores were generated. The predicted values were then used to obtain 1:1 nearest-neighbor matching. Nearest-neighbor matching selects by matching a control subject (patients with uncomplicated disease) whose propensity score is closest to that of case subjects (complicated diverticular disease). Thus, patients for whom the propensity score could not be matched exactly were excluded from outcome comparisons.
Comparisons between groups were conducted by a Mann-Whitney U test and Student t test for continuous variables. The distribution of continuous variables was controlled using a Kolmogorov–Smirnov test for single set of data. The χ2 and the Fisher exact test were used for analysis of categorical variables. Associations between disease phenotype and SF-36 subscale scores as well as physical and mental composite scores were calculated using Mann-Whitney U Test for the univariate analysis. The influence of disease phenotype, sigmoidectomy, age, and sex on SF-36 subscale scores was subsequently explored by multivariate Poisson regression model. Variable “Age” was used as dichotomized variable as age increase by only 1 year was expected to result in almost unmeasurable changes of dependent variable. Robust variance was used in order to avoid overdispersion. A multivariate linear regression model was applied to calculate the factors influencing mental and physical composite scores of SF-36. Since MCS and PCS were not normally distributed, we used their logarithmic values Log(MCS) and Log(PCS) for calculation. The normal distribution of standardized residues was assessed using scatterplot with Loess curve and a histogram. All statistical tests were performed two-sided on a significance level of 0.05.
Results
Patient population
Between October 2009 and November 2015, 392 patients (184 M, 208 F; mean age 61.8 years (27–93 years)) underwent a total of 429 hospitalizations for initial conservative treatment of acute diverticular disease. Thirty-three patients were admitted twice, three patients three times, and one patient 4 times. Two hundred eighty-eight cases were primarily treated in the Department of Gastroenterology, 139 in the Department of Surgery, and two cases in the Department of Urology.
Twenty patients (5%) died during the follow-up period. None of the death cases was caused by diverticular disease. Two hundred eighty patients (M 138, F 142; mean age 60.5 years, range 27–91 years) completed the quality of life questionnaire, while 92 patients did not respond or were lost for follow-up (response rate 75%). Non-responders were significantly older than responders, had a higher probability to be a resident of a nursing home or to suffer from dementia, and presented more often with renal failure and with intake of anticoagulants. Responders underwent surgery for diverticular disease significantly more often than non-responders. The median follow-up period in responders comprised 37.8 months (range 15–85 months) between initial hospitalization and the interview. In patients available for follow-up information but not responding to SF-36 questionnaire, the median follow-up period was 33.1 months (range 0.2 to 82.4 months).
Altogether, 85 of 280 patients presented with complicated (30%) and 195 with uncomplicated diverticulitis at the initial hospitalization. Sixty-two patients underwent sigmoid resection after their initial conservative treatment. During the follow-up period, 88 patients (31%) experienced at least one more flare of diverticular disease—52 of latter patients have been treated in hospital and 37 patients underwent an intestinal resection. Thus, 99 patients had undergone surgery for diverticular disease between the initial hospital stay and the time of answering to the SF-36 questionnaire. The overall postoperative complication rate comprised 22% and in 11 patients (11%), stoma was formatted temporarily. No patient answering the SF-36 questionnaire had a stoma.
For the whole study cohort, the SF-36 mean scores for general health (GH) were 69.1 ± 24.8, 88.9 ± 19.3 for physical functioning (PF), 92.7 ± 18.2 for social functioning (SF), 85.0 ± 25.9 for bodily pain (BP), 77.9 ± 35.6 for role physical limitations (RP), 74.5 ± 17.2 for mental health (MH), 86.2 ± 30.0 for role emotional (RE), and 60.3 ± 20.3 for vitality (VT). The comparison of SF-36 mean scores between patients with complicated and uncomplicated diverticular disease in the whole study population is demonstrated in Table 1. Patients with complicated disease demonstrated statistically significant superiority in several quality of life domains (GH, PF, MH, SF, VT). Also, patients with complicated disease demonstrated significantly better results in physical (54.7 ± 11.1 vs. 51.9 ± 12.0, p = 0.050) and mental compository scores (52.8 ± 8.6 vs. 49.8 ± 10.9, p = 0.026).
Results of propensity score analysis
After propensity score matching, each group consisted of 51 patients. For comparison of baseline characteristics between both groups, see Table 2. Patients with complicated disease had higher level of C-reactive protein at initial hospital admission, were taking acetylsalicylate more often, and were administered to a surgical unit more frequently than patients with uncomplicated disease. Altogether, 52 of 102 patients underwent surgery for diverticular disease: six patients during the initial hospital admission, 23 patients electively after the first hospital admission, and 24 patients (one patient has been operated twice) during the follow-up period. Eight out of 29 patients who underwent sigmoid resection during or immediately after the first admission had suffered from postoperative complications (28%).
Table 3 depicts differences in SF-36 scores between patients with complicated and uncomplicated disease. There was a statistically significant difference, favoring patients with complicated disease in 5 of 8 domains (GH, PF, MH, SF, VT). Also, PCS (56.3 vs. 52.9, p = 0.13) and MCS (53.3 vs. 46.7, p = 0.005) were higher in patients treated for complicated disease, although the difference was statistically significant only for the mental compository score.
Furthermore, the impact of treatment strategy in patients with complicated and uncomplicated disease was analyzed (Table 4). In the sigmoid resection group, patients with complicated disease demonstrated a better quality of life in one of eight SF-36 domains (physical role function), whereas, in conservatively treated patients, complicated disease was associated with better SF-36 scores in 4 of 8 domains (role emotional, physical function, social function, and vitality). Also, mental compository score was significantly higher only in conservatively treated patients with complicated disease but not in those after sigmoidectomy.
Multivariate analysis
Using the multivariate Poisson regression analysis with robust variance, impact of disease phenotype, sigmoidectomy, gender, and age on SF-36 subscale scores was analyzed (Table 5). Complicated diverticular disease as compared with uncomplicated disease was associated with a statistically significant better quality of life in 5 out of 8 subscales whereas sigmoidectomy had a significant (negative) influence only on social functioning (SF). There was a statistically significant association between increasing age and worsening of the physical functioning (PF) as well between increasing age and worsening of the general health (GH).
Linear regression equations (Table 6) were done independently for PCS and MCS using the same variables as potentially confounding factors. There was a statistically significant impact of patients’ age on PCS whereas complicated diverticular disease was independently associated with a better scoring on MCS. Sigmoidectomy had no influence on both SF-36 compository scores.
Discussion
Quality of life assessment gains increasing importance in the decision making process in patients both with benign and malignant disease. However, HrQol studies on patients with diverticular disease are still scarce. The present study is the first to compare health-related quality of life between patients, suffering from UD and CD.
In the presented study, quality of life was superior in patients with complicated disease. The difference, favoring complicated disease, could be demonstrated for all SF-36 domains (statistically significant in 5 domains) as well as in mental compository scores. Similar results were demonstrated after propensity score matching and multivariate analysis. Thus, uncomplicated diverticular disease seems to impact long-term mental quality of life more profoundly than the physical functionality.
In general perception, diverticulitis of the sigmoid colon presents a recurrent disease with asymptomatic intervals between the acute flares. To a certain extent, one part of patients is well characterized by this description [2]. However, a relevant subgroup of patients demonstrate a divergent course of the disease, characterized by chronic abdominal complaints after resolution of acute inflammation. Especially in the uncomplicated group, patients with complete and sustaining response to medical treatment can be differentiated from those who suffer from ongoing and/or atypical complaints. In this context, Wolff et al. recommended the terms “smoldering diverticulitis” and “atypical diverticulitis” [15]. Patients belonging to latter cohorts often show an overlap of symptoms to those suffering from irritable bowel syndrome (IBS). Ongoing microscopic low-grade inflammation is suspected to lead to chronic alterations of the bowel wall and the mesenteric nervous plexus, resulting in an increasing visceral hypersensitivity as described in IBS patients [2]. Clemens and coworkers showed that patients with symptomatic uncomplicated diverticular disease not only have higher pain perception on luminal distension in the diseased sigmoid colon but also in the healthy rectum. Thus, similar to IBS, uncomplicated diverticular disease may lead to the development of a generalized hyperalgesia [16].
Some authors were able to demonstrate that patients with diverticular disease experience an impairment of HrQol, as well as higher rates of depression, anxiety disorders, and somatization [2] [17] [18]. Thus, mental characteristics of the disease show further similarities with IBS. The dominance of mental health impairment in all assessments of our study may be explained in this context. Those similarities between patients with IBS and patients with uncomplicated diverticular disease as well as the fact that the uncomplicated disease is not progressing to a complicated one lead to the assumption that UD and CD are basically two different disease entities. However, in contrast to IBS, patients with uncomplicated are older and the predominance of female gender is not as strong as in IBS [17].
In our study, the difference in quality of life scores was strongly diminished by surgery. Some impairment of quality of life after surgery might be attributable to the so-called post sigmoidectomy syndrome which was described by Levack et al. About 25% of patients who previously underwent sigmoidectomy for diverticular disease suffered after surgery from fecal incontinence and 20% from fecal urgency and incomplete emptying [19]. These data seem to be alarming. Damage of the pelvic and inferior mesenteric plexus might be causative (20).
According to current knowledge, there is a low risk of complicated recurrence, emergency surgery, and unplanned stoma formation in patients with recurrent diverticulitis [3]. Given the fact that the avoidance of recurrence is the main reason for sigmoidectomy, it is questionable, whether all patients are benefiting from surgery, especially those with uncomplicated disease.
Limitations
The study is limited by its retrospective character and the lack of longitudinal data. An unbiased assessment of impact of treatment strategy (conservative vs. operative) on HQoL could only be obtained by a randomized study. Also, some 25% of patients did not respond to quality of life questionnaires which probably led to more positive assessment. Furthermore, we did not study the influence of perioperative morbidity (revision surgeries, stoma etc.) on quality of life potentially ignoring an important confounding factor.
Conclusion
Long-term health-related quality of life was significantly worse in patients with uncomplicated disease as compared with those with complicated diverticulitis in our study. The difference was largest regarding the mental health-related domains. Probably, UD and CD pose as different disease entities. Patient with uncomplicated disease should be selected carefully to undergo sigmoidectomy.
References
Bharucha AE, Parthasarathy G, Ditah I, Fletcher JG, Ewelukwa O, Pendlimari R, Yawn BP, Melton JL, Schleck C, Zinsmeister AR (2015) Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol 110(11):1589–1596
Strate LL, Modi R, Cohen E, Spiegel BMR (2012) Diverticular disease as a chronic illness: evolving epidemiologic and clinical insights. Am J Gastroenterol 107(10):1486–1493
Friel CM (2012) To operate or not to operate? Should functional outcomes after sigmoid colectomy for diverticulitis influence our decision making? Dis Colon Rectum 55(1):1–3
Fozard JBJ, Armitage NC, Schofield JB, Jones OM (2011) Association of Coloproctology of Great Britain and Ireland. ACPGBI position statement on elective resection for diverticulitis. Colorectal Dis Off J Assoc Coloproctology G B Irel. 13(Suppl 3):1–11
Kruis W, Germer C-T, Leifeld L (2014) German Society for Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Diverticular disease: guidelines of the German Society for Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Digestion. 90(3):190–207
Andeweg CS, Mulder IM, Felt-Bersma RJF, Verbon A, van der Wilt GJ, van Goor H, Lange JF, Stoker J, Boermeester MA, Bleichrodt RP (2013) Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg 30(4–6):278–292
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57(3):284–294
Leifeld L, Germer CT, Böhm S, Dumoulin FL, Häuser W, Kreis M et al (2014) S2k guidelines diverticular disease/diverticulitis. Z Gastroenterol 52(7):663–710
Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J et al (2012) Danish national guidelines for treatment of diverticular disease. Dan Med J 59(5):C4453
Sallinen V, Mali J, Leppäniemi A, Mentula P (2015) Assessment of risk for recurrent diverticulitis: a proposal of risk score for complicated recurrence. Medicine (Baltimore) 94(8):e557
Lamb MN, Kaiser AM (2014) Elective resection versus observation after nonoperative management of complicated diverticulitis with abscess: a systematic review and meta-analysis. Dis Colon Rectum 57(12):1430–1440
Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C, Marcello PW, Schoetz DJ (2011) Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum 54(3):283–288
Livingston EH, Fomby TB, Woodward WA, Haley RW (2011) Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg Chic Ill 1960 146(3):308–314
Bullinger M (1995) German translation and psychometric testing of the SF-36 Health Survey: preliminary results from the IQOLA Project. International Quality of Life Assessment. Soc Sci Med 1982 41(10):1359–1366
Wolff BG, Boostrom SY (2012) Prophylactic resection, uncomplicated diverticulitis, and recurrent diverticulitis. Dig Dis Basel Switz 30(1):108–113
Clemens CHM, Samsom M, Roelofs J, van Berge Henegouwen GP, Smout AJPM (2004) Colorectal visceral perception in diverticular disease. Gut. 53(5):717–722
Spiller R (2012) Is it diverticular disease or is it irritable bowel syndrome? Dig Dis Basel Switz. 30(1):64–69
Bolster LT, Papagrigoriadis S (2003) Diverticular disease has an impact on quality of life -- results of a preliminary study. Colorectal Dis Off J Assoc Coloproctology G B Irel 5(4):320–323
Levack MM, Savitt LR, Berger DL, Shellito PC, Hodin RA, Rattner DW, Goldberg SM, Bordeianou L (2012) Sigmoidectomy syndrome? Patients’ perspectives on the functional outcomes following surgery for diverticulitis. Dis Colon Rectum 55(1):10–17
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was in accordance with the Declaration of Helsinki and approved by the medical ethics board of the Bavarian medical council.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study highlights
What is current knowledge
• Diverticulitis is one of the most frequent abdominal disorders, leading to a significant influence on patients’ wellbeing and health care costs.
• There is a scarcity of quality of life assessments in clinical practice, guideline recommendations, and scientific analyses.
What is new here
• This is the first study, comparing health-related quality of life (HrQol) of patients, suffering from complicated (CD) and uncomplicated (UD) diverticular disease.
• Significantly worse results of HrQol-scoring in UD underline the hypothesis that UD and CD are different disease entities with diverse pathophysiologic courses, claiming for alternate assessment and management.
Rights and permissions
About this article
Cite this article
Sohn, M., Agha, A., Roussos, D. et al. Disease phenotype rather than treatment strategy impacts the long-term quality of life in patients with diverticular disease. Int J Colorectal Dis 34, 1749–1756 (2019). https://doi.org/10.1007/s00384-019-03385-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-019-03385-0