Abstract
Background
There is significant variation in the use of mechanical bowel preparation and oral antibiotics prior to left-sided elective colorectal surgery. There has been no consensus internationally.
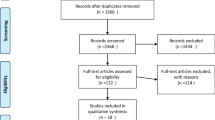
Methods
This was a retrospective analysis of the 2015 American College of Surgeons National Surgical Quality Improvement Program database. Patients were divided into four groups: those who had mechanical bowel preparation with oral antibiotics, mechanical bowel preparation alone, oral antibiotics alone and no preparation. The main outcome measures included overall, superficial, deep and organ/space surgical site infections. Secondary outcomes included anastomotic leak, ileus and rate of Clostridium difficile.
Results
A total of 5729 patients were included for analysis. The overall surgical site infection rate (any superficial, deep or organ/space infection) was significantly lower in the mechanical bowel preparation and oral antibiotics approach when compared to no preparation (OR = 0.46, 95% CI 0.36–0.59, P < 0.0001). On multivariable logistic regression analysis, mechanical bowel preparation with oral antibiotics maintained a lower risk of overall surgical site infections. MBP and OAB also had a protective effect on anastomotic leak in both the laparoscopic and open cohorts (laparoscopic multivariable adjusted OR = 0.42 (0.19–0.94), P = 0.035; open multivariable adjusted OR = 0.3 (0.12–0.77), P = 0.012). Mechanical bowel preparation alone and oral antibiotics alone was not associated with a significant decrease in surgical site infections. There was no increase in C. difficile occurrences with the use of oral antibiotics.
Conclusion
Mechanical bowel preparation with oral antibiotics significantly minimised surgical site infections and anastomotic leak following both laparoscopic and open left-sided restorative colorectal surgery. Mechanical bowel preparation alone did not reduce surgical site infections. There was a trend to reduction in surgical site infections with oral antibiotics alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Debate on the role of mechanical bowel preparation (MBP) and oral antibiotics (OAB) prior to colorectal surgery continues as large population-based studies and meta-analyses over the past four decades continue to report a range of conflicting outcomes [1,2,3,4,5,6,7,8]. Even recent studies evaluating the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database have reported different outcomes [2,3,4]. Of note, the study by Garfinkle et al. (2017) [3] recommended OAB alone, but the study by Kiran et al. (2015) [2] and Klinger et al. (2017) [4] were in favour of MBP with OAB.
It is not surprising that international guidelines such as those in America, Europe and Asia-Pacific have not reached an agreement. While the American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement in 2017 recommended the routine use of ‘MBP with OAB before elective colorectal surgery’ [9], recent international guidelines such as the Australian guidelines recommended that ‘MBP should not be used routinely in colonic surgery’ [10].
In a survey of European colorectal surgeons, less than 10% stated that they used OAB with or without MBP, and majority favoured no preparation for colon surgery and approximately 80% used MBP for rectal surgery [11]. No preparation for colon surgery and MBP alone for rectal surgery is still common practice internationally. This practice is consistent with the findings from the landmark Cochrane review in 2011 which reported no benefit for MBP in colonic surgery but suggested that MBP may be used selectively in rectal surgery [5]. The lack of benefit for MBP alone, and in some cases, harm, has also been demonstrated in numerous other studies [7, 8, 12, 13], so that while recent ACS-NSQIP studies have demonstrated that MBP with OAB is associated with benefit, it is difficult to change long-term wide-held beliefs on MBP which has been supported by levels 1 and 2 evidence reported over decades.
To date, many of the ACS-NSQIP studies on this topic have reported on data associated with a wide range of colorectal surgery for both sides [2,3,4]. An array of statistical methods such as propensity scoring, coarsened exact matching and multivariate regression analysis have been used. However, surgeons are wary of sophisticated statistical techniques that do not replace the value of a well-designed study with appropriate inclusion and exclusion criteria.
The aim of this study was to perform a focused evaluation of the ACS-NSQIP data to include only elective left-sided restorative colorectal surgery with and without faecal diversion. A separate subset analysis of open and laparoscopic outcomes was performed to determine if MBP and OAB have a role in both open and laparoscopic surgery. The 2012–2014 data was excluded, as this time period had already been extensively studied and consistently favoured OAB strategies and we wanted to assess a cohort independent of this time period.
Methods
Patients and data collection
The ACS-NSQIP targeted colectomy data from 2015 was used for analysis. The NSQIP database is a nationwide database where data are collected by trained clinical reviewers. Data on demographics, pre-operative, intraoperative and 30-day post-operative outcomes with hundreds of accurate and reliable data points were used.
Data for elective colorectal operations from the targeted colectomy Participant User File (PUF) with the American Medical Association Current Procedural Terminology (CPT) codes 44145 (colectomy, partial; with coloproctostomy (low pelvic anastomosis)), 44146 (colectomy, partial; with coloproctostomy (low pelvic anastomosis) with colostomy), 44207 (laparoscopy, surgical; colectomy, partial, with anastomosis, with coloproctostomy (low pelvic anastomosis)), 44208 (laparoscopy, surgical; colectomy, partial, with anastomosis, with coloproctostomy (low pelvic anastomosis) with colostomy) were included for analysis. These codes have been previously identified as the ‘Proctectomy’ group in the ‘Targeted Colectomy’ NSQIP database [2, 3].
Other CPT codes in the targeted colectomy PUF data included 44143, 44144, 44147 and 44206. CPT code 44147 (colectomy, partial, combined abdominal and transanal approach) was excluded as this was not a targeted procedure in this study. We also excluded 44143 and 44206 (Hartmann type procedure—open and laparoscopic) and 44144 (Colectomy, partial; with resection with stoma and creation of mucofistula) as these procedures were not restorative. Data from the ACS-NSQIP targeted proctectomy PUF were not used as the targeted proctectomy data does not include information on bowel preparation and oral antibiotics which is a limitation of the targeted proctectomy data.
The data gathered for analysis included patient demographics, pre-operative, intraoperative and 30-day post-operative variables. The primary outcomes of interest in this study included superficial (subcutaneous), deep (fascia, muscle layers) and organ space surgical site infection (SSI) (organ or spaces other that surgical incisions), anastomotic leak and post-operative ileus. Anastomotic leak has been defined by NSQIP as endoluminal contents through an anastomosis and has been classified based on need for antibiotics, drainage and surgical intervention [14]. This is similar to the International Study Group of Rectal Cancer (ISREC) severity grading system of anastomotic leak after anterior resection based on need for intervention [15, 16]. The ISREC grading system classifies leaks based on no treatment, non-operative treatment and operative treatment (similar to NSQIP)—but additionally stratifies treatment of leak by first line treatment and full clinical course (not included in NSQIP).
Statistical analysis
Normality of data distribution was assessed and information such as patients’ co-morbidities, pre- and post-operative characteristics were summarised using descriptive statistics (Table 1). Continuous variables were presented as medians with interquartile range (IQR, range from the 25th to the 75th percentile) due to data skew and comparisons made using the Mann Whitney U tests. Categorical data were presented as proportions (%) with comparisons made using the chi-square (χ2) or as required the Fisher exact tests. If appropriate, the Kruskal-Wallis test was used to compare groups of continuous data or to test for trends.
Variables such as use of MBP with or without the use of OAB were grouped into four categories. Similarly, primary indication was grouped into four categories (acute diverticulitis, Crohn’s disease or ulcerative colitis, colon cancer or other). Furthermore, variables such as age of 80 years or more, American Society of Anaesthesiology score of 3 or more, body mass index of 30 kg/m2 or more, albumin levels of 3.50 g/dL or more, white blood count (WBC × 109/) of 12 or more, haematocrit of 30% or more, total operative time of 180 min or more and anastomotic leak were dichotomised based on clinical importance. All comparisons were made by the operative technique which was classified as the laparoscopic or open. Missing variable data of greater than 90% was not included in the analysis. The rate of missing data in this study was found to be minimal and hence unlikely to modify findings with the use of multiple imputation techniques or sensitivity analysis.
Univariable (unadjusted) logistic regressions were used to test the significance of MBP and use of ABX regimen, pre- and post-operative factors for the primary outcome of any SSI which included superficial, deep or organ space occupying. Separate models were developed for the laparoscopic and open colectomy method (Table 3). For the primary outcome of any SSI (superficial, deep or organ) and the secondary outcome anastomotic leak, a multivariable (adjusted) logistic regression model was fitted to determine predictors of these outcomes while controlling for other significant covariates identified on univariable analyses (Tables 4 and 5). Statistical analyses were performed using SPSS 22.0 (IBM SPSS Statistics for Windows, Armonk, NY, USA). All tests were two tailed and differences considered statistically significant at a P < 0.05 level.
Results
Study population
A total of 5729 patients were included for analysis, 2721 (47.5%) had both MBP and OAB, 1713 (29.9%) had MBP alone, 199 (3.5%) had OAB alone and 1906 (19.1%) had no preparation. Patients in all four groups were comparable for age, gender and BMI. There was a statistically significant difference in the proportion of patients in the no preparation group and MBP alone group who had ASA ≥ 3 when compared to the subgroup who had OAB ± MBP. There was also a difference in the indication for surgery between each subgroup.
In terms of co-morbidities, there was no significant difference between the groups with respect to frequency of smoking, dyspnoea, COPD, ascites, congestive heart failure, steroid use for chronic conditions, chemotherapy within 90 days, bleeding disorders, pre-operative transfusions and pre-operative infections and albumin. A greater proportion of patients in the no preparation group were diabetic when compared to the other subgroups. Clinically relevant variables with respect to patient characteristics were similar and all study covariates were later considered in multivariable analyses (see Table 1).
The rate of minimally invasive surgery was 67–73.5% between the four subgroups, the rate of stoma was 2–4.7% in the open group and 2–5.3% in the minimally invasive group. There was no difference in operating time between the four groups based on MBP and OAB status.
Outcomes
Pooled laparoscopic and open data
With both laparoscopic and open data pooled, the overall SSI rate (any superficial, deep or organ space infection) was significantly lower in the MBP and OAB group when compared to no preparation (OR = 0.46 (0.36–0.59), P < 0.0001) on univariable analysis. On multivariable logistic regression analysis, the MBP and OAB group maintained a lower risk of overall SSIs. The OAB group alone had a trend to reduction of SSIs (univariable OR 0.84 (0.51–1.38), P = 0.49; multivariable adjusted OR 0.50 (0.16–1.54), P = 0.23), but this was not statistically significant. MBP alone prior to elective left-sided restorative colorectal surgery with pelvic anastomosis did not reduce the risk of SSIs (multivariable adjusted OR 0.98 (0.58–1.65)).
Other clinically relevant factors which increased SSI rates included anastomotic leak, BMI ≥ 30 kg/m2, dialysis, bleeding disorders and ascites on multivariable analysis. ASA, diabetes, dyspnoea, disseminated cancer, prior wound infection, > 10% body weight loss, pre-operative sepsis, albumin, WBC and total operative time were statistically significant on univariable analysis, but the adjusted multivariable OR was not statistically significant (refer to Table 2).
Separate analysis of open and laparoscopic data
When open and laparoscopic data were assessed separately, the protective effect of MBP and OAB on frequency of overall SSIs was maintained on univariable analyses in both groups (laparoscopic: OR 0.52 (0.37–0.75), P < 0.0001); open: OR 0.41 (0.29–0.57), P < 0.0001).
On multivariable analysis, the benefit of MBP and OAB for open elective left-sided colectomy remained statistically significant (OR = 0.41 (0.20–0.83), P = 0.013). For the laparoscopic cohort, the multivariable adjusted OR showed a trend but just missed statistical significance (OR = 0.44 (0.19–1.04), P = 0.062).
There was a trend to reduction in overall SSIs in the OAB alone group for both the open (multivariable adjusted OR = 0.5 (0.16–1.54), P = 0.23) and laparoscopic cohort (multivariable adjusted OR = 0.84 (0.51–1.38), P = 0.49) but outcomes were not statistically significant. On univariable analysis of the laparoscopic group, there was no benefit with respect to SSI rates for OAB alone (OR = 1.24 (0.66–2.33), P = 0.51). This study was not able to demonstrate a statistically significant improvement in SSI rates with OAB alone.
The majority of resections were performed laparoscopically. On univariable analysis, other factors influencing SSI rates in the laparoscopic cohort included BMI ≥ 30 kg/m2, ASA ≥ 3, post-operative blood transfusion, sepsis prior to surgery, total operative time ≥ 180 min and anastomotic leak. The clinically relevant factors that remained statistically significant on multivariable analyses included anastomotic leak, ascites, prolonged operative time and steroid use for chronic conditions (refer to Tables 3 and 4). For open surgery, prior wound infection was also a significant risk factor for risk of overall SSIs.
MBP and OAB also had a protective effect on anastomotic leak in both the laparoscopic and open cohorts (laparoscopic: multivariable adjusted OR = 0.42 (0.19–0.94), P = 0.035; open: multivariable adjusted OR = 0.3 (0.12–0.77), P = 0.012). OAB alone did not have a protective effect in reducing risk of anastomotic leak in the laparoscopic group (OR = 1.11 (0.28–4.37), P = 0.88). There was a trend to risk reduction in terms of anastomotic leak in the open group (OR = 0.43 (0.065–2.28), P = 0.37) but this was not statistically significant (see Table 5, Figs. 1 and 2).
Total anastomotic leak rate and leak rate by severity based on intervention required
This study reported a statistically significant reduction in total anastomotic leak rate for MBP and OAB in pooled laparoscopic and open data, and also for both open and laparoscopic cohorts when analysed separately. The overall leak rate was low in both the open and laparoscopic cohort. A separate analysis was performed to assess the risk of leak stratified by intervention required (no treatment/intervention/reoperation/unknown). The aim of this was not to show a statistically significant outcome as the number of leaks was low in both groups and it was not likely to draw conclusive results from this analysis. However, this analysis was performed as anastomotic leaks are an area of significant interest to colorectal surgeons. In this study, MBP with OAB had the lowest rate of leak requiring intervention and leak requiring reoperation in both the laparoscopic and open cohorts, but this did not reach statistical significance in either group. OAB alone had the second lowest rate of leak requiring intervention and leak requiring reoperation.
Risk of Clostridium difficile
Based on the available data, there was no increase in C. difficile occurrences with the use of MBP and OAB. The C. difficile rate was 1.3% (7/528) in the no preparation group, 1.2% (10/828) in the MBP alone group, 1.0% (1/103) in the OAB alone group and 1.2% (17/1464) in the MBP and OAB group. No significant differences were detected in C. difficile occurrences based on MBP and OAB status (P = 0.0987). However, there was a significant amount of missing data in this field (51% (2923/5729) completed).
Discussion
While there have been many ACS-NSQIP studies on this topic, this study specifically reports on left-sided elective restorative colorectal surgery with pelvic anastomosis with and without faecal diversion. This study also specifically reports on open and laparoscopic cohorts separately and also provides an analysis on anastomotic leaks classified by severity based on interventions required. Furthermore, as we previously mentioned, we only included the 2015 ACS-NSQIP data. By only analysing the 2015 ACS-NSQIP data, this study provided another point of difference from other recent studies. Studies which included data from the 2012–2014 period include Kiran et al. (2015) which analysed the 2012 ACS-NSQIP data and was in favour of MBP and OAB [2], Garfinkle et al. (2017) which analysed the 2012–2014 ACS-NSQIP data and favoured OAB alone [3] and Klinger et al. (2017) which evaluated the 2012–2015 ACS-NSQIP data, favoured MBP with OAB [4].
Comparing outcomes of this study with RCTs and meta-analysis
Majority of RCTs studying MBP and OAB report outcomes associated with open surgery. As a result, the meta-analyses which have pooled results on this topic [1, 5,6,7,8, 12] have reported on outcome measures based mainly on data from open surgery. There have been very few RCTs reporting on laparoscopic outcomes only [17, 18] and several RCTs reporting on both laparoscopic and open surgery [19,20,21,22]. There have only been a handful of RCTs that have reported on left-sided colorectal surgery [13, 20, 23]. A meta-analysis of RCTs only by Chen et al. on this topic demonstrated a benefit with MBP and OAB over MBP alone [1], but it did not report on other MBP and OAB strategies nor side of resection. Our study was able to show that MBP with OAB for left-sided restorative colorectal surgery was associated with a statistically significant risk reduction in anastomotic leak in both groups, and a significant reduction in SSIs in the open cohort and trend to risk reduction in SSIs that just missed statistical significance on multivariable analysis in the laparoscopic cohort.
Our study also confirmed no difference between MBP alone and no preparation. The outcome of our study was similar to several meta-analyses including the Cochrane review [5, 6] which have demonstrated no difference between MBP alone and no preparation in terms of mortality, anastomotic leak, surgical site infection or reoperation. Several meta-analyses have even shown harm with MBP [7, 8]. Our study did not show increased risk of harm with MBP alone.
Comparing outcomes of this study with other ACS-NSQIP studies
While most ACS-NSQIP studies report on both sides, our study was not the first ACS-NSQIP study to look specifically at left-sided colorectal surgery. Elnahas et al. evaluated left-sided colorectal surgery using the 2011–2012 ACS-NSQIP data. This study reported on MBP alone vs. no preparation prior to elective left-sided colorectal surgery but did not report on OAB. This study showed that MBP alone decreased the rate of anastomotic leaks [24]. Our study was not able to demonstrate a difference between MBP alone and no preparation. Compared to no preparation, MBP alone was not associated with a statistically significant reduction in anastomotic leak in total nor in the laparoscopic group (OR 0.94, 95% CI 0.43–2.03). There appeared to be a risk reduction for MBP alone vs. no preparation in the open group (OR 0.29, 95% CI 0.087–0.98) but this was an isolated finding. There were no other risk reductions in SSIs or short-term outcomes with MBP alone when compared to no preparation in this study. The greatest benefit in terms of minimising anastomotic leak in both the open and laparoscopic groups was with MBP with OAB (Laparoscopic OR = 0.42, 95% CI 0.19–0.94; Open OR = 0.30, 95% CI 0.12–0.77). OAB alone did not reduce the risk of anastomotic leak on multivariate logistic regression.
Another study that reported on left-sided colorectal surgery was by Moghadamyeghaneh et al. which assessed the 2012–2013 ACS-NSQIP data [25]. This study included outcomes from both sides but performed a separate analysis of right and left sides [25]. In this study, left-sided surgery included surgery for splenic flexure, descending colon, sigmoid and rectosigmoid junction surgery [25], whereas our study focused only on left-sided colorectal surgery with low pelvic anastomosis. While there were differences between the study by Moghadamyeghaneh et al. and ours, both studies showed that MBP with OAB reduced SSIs and anastomotic leakage [25]. Other ACS-NSQIP studies which have favoured MBP with OAB include studies by Kiran et al. [2], Scarborough et al. [26] and Klinger et al. [4]. The point of difference between these studies and ours was that our study did not include any data from the 2012–2014 period and we excluded a large number of procedures that were included in the abovementioned studies.
This study challenged the outcomes reported by the ACS-NSQIP studies performed by Garfinkle et al. [3] and Atkinson et al. [27] which recommend OAB alone strategies. Although we demonstrated a trend to reduction in SSIs with OAB alone in our study, results were not statistically significant. On univariable analysis of the laparoscopic cohort, the OR for SSIs for OAB alone was 1.24 (0.66–2.33), P = 0.51; on multivariable analysis, the OR was 0.58 (0.11–3.08), P = 0.51. Nor were we able to demonstrate a statistically significant benefit in minimising anastomotic leak with OAB alone. The lack of statistical significance in our study may have been due to the smaller number of patients who received OAB alone (n = 199) as we only included four CPT codes for analysis to perform a focused analysis. This was the least common of the four strategies (MBP with OAB, OAB alone, MBP alone, no preparation) prior to elective left-sided colorectal surgery reported in the ACS-NSQIP database.
This study has several limitations including the observational nature of this study, lack of information on the type of MBP and OAB used, the inherent difficulties and inaccuracies of using data from a large surgical registry with missing and unknown data, the small number of patients in the OAB alone group, the inconsistencies in the NSQIP data for colectomies and proctectomies, lack of propensity score matching (we found propensity score matching significantly reduced the number of observations used in analysis without any real advantage to the multivariable logistic regression model), group heterogeneity and high risk of selection bias both due to the non-randomised nature of this study as well as missing data in variable fields.
The main strength of this study was the specific inclusion criteria to only include data from left-sided elective restorative colorectal surgery with pelvic anastomosis only, the separate analysis for open and laparoscopic procedures, analysis of anastomotic leak classified by severity based on interventions required and analysis of a cohort independent from previous studies. By using a large population-based database, even with a focused review of four CPT codes for a one-year period, the size of our study was still substantial (n = 5729). To the best of our knowledge, this is the largest observational study evaluating the role of MBP with OAB on SSIs and anastomotic leak specifically prior to left-sided restorative colorectal surgery with pelvic anastomosis. A large, well-designed, multicentre, placebo-controlled RCT comparing all four strategies or at least MBP with OAB vs. OAB alone (with IV antibiotics as standard) would be ideal to confirm the findings of this study.
Conclusions
This study has clearly demonstrated that of the four strategies (MBP with OAB, OAB alone, MBP alone, no preparation), MBP with OAB is associated with the greatest risk reduction in SSIs and anastomotic leak when used prior to elective left-sided restorative colorectal surgery with pelvic anastomosis with and without faecal diversion in both a laparoscopic and open setting. MBP alone has no significant benefit over no preparation. Both MBP alone and no preparation strategies were associated with higher risk of SSIs. There may be a small benefit with OAB alone, but it did not reach statistical significance. MBP with OAB is the best approach to reduce surgical site infection in patients undergoing left-sided elective restorative colorectal surgery.
References
Chen M, Song X, Chen LZ, Lin ZD, Zhang XL (2016) Comparing mechanical bowel preparation with both oral and systemic antibiotics versus mechanical bowel preparation and systemic antibiotics alone for the prevention of surgical site infection after elective colorectal surgery: a meta-analysis of randomized controlled clinical trials. Dis Colon Rectum 59:70–78
Kiran RP, Murray AC, Chiuzan C, Estrada D, Forde K (2015) Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg 262:416–425 discussion 23-5
Garfinkle R, Abou-Khalil J, Morin N, Ghitulescu G, Vasilevsky CA, Gordon P, Demian M, Boutros M (2017) Is there a role for oral antibiotic preparation alone before colorectal surgery? ACS-NSQIP analysis by coarsened exact matching. Dis Colon Rectum 60:729–737
Klinger AL, Green H, Monlezun DJ (2017) The role of bowel preparation in colorectal surgery: results of the 2012-2015 ACS-NSQIP data. Ann Surg https://doi.org/10.1097/SLA.0000000000002568
Guenaga KF, Matos D, Wille-Jorgensen P (2011) Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev (9):Cd001544
Dahabreh IJ, Steele DW, Shah N, Trikalinos TA (2015) Oral mechanical bowel preparation for colorectal surgery: systematic review and meta-analysis. Dis Colon Rectum 58:698–707
Slim K, Vicaut E, Launay-Savary MV, Contant C, Chipponi J (2009) Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg 249:203–209
Bucher P, Mermillod B, Gervaz P, Morel P (2004) Mechanical bowel preparation for elective colorectal surgery: a meta-analysis. Arch Surg 139:1359–1364 discussion 65
Holubar SD, Hedrick T, Gupta R, Kellum J, Hamilton M, Gan TJ et al (2017) American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on prevention of postoperative infection within an enhanced recovery pathway for elective colorectal surgery. Perioper Med (London, England) 6:4
Elizabeth Murphy AH, Freeman V, Barclay K, Burbury K, Froessler B, Koh C, Price T, Robinson K; Cancer Council Australia Colorectal Cancer Guidelines Working Party (2017) PRP2-5, 7: Can peri operative management be optimised? Clinical practice guidelines for the prevention, early detection and management of colorectal cancer. Version URL: https://wiki.cancer.org.au/australiawiki/index.php?oldid=173079, cited 2018 Mar 30
Devane LA, Proud D, O'Connell PR, Panis Y (2017) A European survey of bowel preparation in colorectal surgery. Color Dis 19:O402–O406
Slim K, Vicaut E, Panis Y, Chipponi J (2004) Meta-analysis of randomized clinical trials of colorectal surgery with or without mechanical bowel preparation. Br J Surg 91:1125–1130
Bucher P, Gervaz P, Soravia C, Mermillod B, Erne M, Morel P (2005) Randomized clinical trial of mechanical bowel preparation versus no preparation before elective left-sided colorectal surgery. Br J Surg 92:409–414
(2014) User Guide for the 2013 ASCS NSQIP Procedure Targeted Participant Use Data File. American College of Surgeons National Surgical Quality Improvement Program. November 32
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
Kulu Y, Ulrich A, Bruckner T, Contin P, Welsch T, Rahbari NN, Büchler MW, Weitz J (2013) Validation of the International Study Group of Rectal Cancer definition and severity grading of anastomotic leakage. Surgery 153:753–761
Hata H, Yamaguchi T, Hasegawa S, Nomura A, Hida K, Nishitai R, Yamanokuchi S, Yamanaka T, Sakai Y (2016) Oral and parenteral versus parenteral antibiotic prophylaxis in elective laparoscopic colorectal surgery (JMTO PREV 07-01): a phase 3, multicenter, open-label, randomized trial. Ann Surg 263:1085–1091
Ikeda A, Konishi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Akiyoshi T, Yamaguchi T (2016) Randomized clinical trial of oral and intravenous versus intravenous antibiotic prophylaxis for laparoscopic colorectal resection. Br J Surg 103:1608–1615
Bertani E, Chiappa A, Biffi R, Bianchi PP, Radice D, Branchi V, Spampatti S, Vetrano I, Andreoni B (2011) Comparison of oral polyethylene glycol plus a large volume glycerine enema with a large volume glycerine enema alone in patients undergoing colorectal surgery for malignancy: a randomized clinical trial. Color Dis 13:e327–e334
Bretagnol F, Panis Y, Rullier E, Rouanet P, Berdah S, Dousset B, Portier G, Benoist S, Chipponi J, Vicaut E (2010) Rectal cancer surgery with or without bowel preparation: the French GRECCAR III multicenter single-blinded randomized trial. Ann Surg 252:863–868
Sasaki J, Matsumoto S, Kan H, Yamada T, Koizumi M, Mizuguchi Y, Uchida E (2012) Objective assessment of postoperative gastrointestinal motility in elective colonic resection using a radiopaque marker provides an evidence for the abandonment of preoperative mechanical bowel preparation. J Nippon Med Sch 79:259–266
Sadahiro S, Suzuki T, Tanaka A, Okada K, Kamata H, Ozaki T, Koga Y (2014) Comparison between oral antibiotics and probiotics as bowel preparation for elective colon cancer surgery to prevent infection: prospective randomized trial. Surgery 155:493–503
Zmora O, Mahajna A, Bar-Zakai B, Hershko D, Shabtai M, Krausz MM, Ayalon A (2006) Is mechanical bowel preparation mandatory for left-sided colonic anastomosis? Results of a prospective randomized trial. Tech Coloproctol 10:131–135
Elnahas A, Urbach D, Lebovic G, Mamdani M, Okrainec A, Quereshy FA, Jackson TD (2015) The effect of mechanical bowel preparation on anastomotic leaks in elective left-sided colorectal resections. Am J Surg 210:793–798
Moghadamyeghaneh Z, Carmichael JC, Mills SD, Pigazzi A, Stamos MJ (2015) Association between prolonged ileus and type of colon resection in colon cancer surgery. Surgical Endoscopy and Other Interventional Techniques 29:S415
Scarborough JE, Mantyh CR, Sun Z, Migaly J (2015) Combined mechanical and oral antibiotic bowel preparation reduces incisional surgical site infection and anastomotic leak rates after elective colorectal resection: an analysis of colectomy-targeted ACS NSQIP. Ann Surg 262:331–337
Atkinson SJ, Swenson BR, Hanseman DJ, Midura EF, Davis BR, Rafferty JF, Abbott DE, Shah SA, Paquette IM (2015) In the absence of a mechanical bowel prep, does the addition of pre-operative oral antibiotics to parental antibiotics decrease the incidence of surgical site infection after elective segmental colectomy? Surg Infect 16:728–732
Author information
Authors and Affiliations
Contributions
Dr. James Toh made substantial contributions to the design and interpretation of the study including acquisition of data, statistical analysis, drafting and revision of manuscript. Associate Professor Kerry Hitos contributed to the statistical analysis and revision of manuscript. Susan Donovan and Mingjuan Zeng contributed to the acquisition of data and revision of manuscript. Dr. Kevin Phan, Dr. Grahame Ctercteko, Dr. Nimalan Pathma-Nathan, Dr. Toufic El-Khoury, Associate Professor Arthur Richardson, Associate Professor Gary Morgan, Dr. Reuben Tang, Dr. Dan Chu and Associate Professor Greg Kennedy contributed to the drafting and revision of manuscript. Final approval of the version to be published was made by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Toh, J.W.T., Phan, K., Ctercteko, G. et al. The role of mechanical bowel preparation and oral antibiotics for left-sided laparoscopic and open elective restorative colorectal surgery with and without faecal diversion. Int J Colorectal Dis 33, 1781–1791 (2018). https://doi.org/10.1007/s00384-018-3166-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3166-8