Abstract
Purpose
The purpose of this study was to determine whether patients diagnosed with colorectal cancer and synchronous unresectable metastases (stage IV) can benefit from resection of the primary tumor in terms of an improvement in cancer-specific survival.
Methods
Stage IV colorectal cancer patients are eligible for inclusion in a randomized multicenter study carried out in 22 hospitals throughout Spain. Exclusion criteria are rectal tumors below 12 cm from the anal verge or locally advanced tumors, multiple bone or central nervous system metastases, and history of another primary cancer. The parallel design of the trial includes an arm of systemic chemotherapy alone versus an arm of resection of the primary tumor plus systemic chemotherapy after surgery. The primary endpoint of the study is cancer-specific survival that is assessed with a minimum follow-up of 24 months. Secondary endpoints are postoperative morbidity and mortality associated with resection of the primary tumor, complications and need of surgery in patients treated with systemic chemotherapy only, safety of systemic chemotherapy in both treatment strategies, and quality of life.
Conclusions
Confirmation of a survival benefit of surgical resection of the primary tumor in stage IV colorectal cancer patients not amenable to curative therapy is very relevant from a clinical and societal perspective, particularly considering the increase in the incidence and prevalence of colorectal cancer in developed countries.
ClinicalTrials.gov Identifier: NCT02015923.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Resection of the primary tumor in asymptomatic patients with colorectal cancer (CRC) and synchronous unresectable metastases was a common procedure until the 1990s even though scientific evidence of its benefit was scarce. The purpose of resection was to control the possible complications due to the primary tumor, which occurred in approximately 20% of patients [1]. However, after the introduction of new chemotherapeutic agents resulting in an improvement in global survival of stage IV CRC patients, data reported in the literature and scientific societies including the American Cancer Society recommend treating these patients with chemotherapy only, reserving surgery for patients with symptoms derived from the primary tumor or at risk of intestinal obstruction [2]. This change in the management strategy of CRC patients with unresectable metastases is based on the beneficial effects of chemotherapy not only on the metastatic disease but also on the primary tumor [3, 4]. It has been shown that the rate of primary tumor-related complications is reduced by 7%. Also, the benefits on survival are remarkable when survival rates of patients treated with modern chemotherapy combination regimens are compared with those of patients treated in the past decades when only fluorouracil was available [5,6,7].
Recent evidence points towards an improvement in prognosis associated with resection of the primary tumor before starting systemic chemotherapy in patients with stage IV CRC and a good performance status [8, 9]. By contrast, other authors argue that benefits of primary tumor resection on overall survival have not been convincingly demonstrated and, furthermore, that morbimortality related to tumor resection should be avoided, because it could delay the start of chemotherapy and therefore have a negative effect on survival [4, 10,11,12]. In fact, different studies have reported a longer mean survival in patients undergoing resection of the primary tumor versus no resection [8, 9, 13, 14]. These data, however, have been obtained from non-randomized retrospective case series studies, and it is possible that patients treated surgically had a better performance status or relatively small tumor burden. Other studies have also found a higher toxicity of chemotherapy in patients without resection when compared to patients who had resection of the primary tumor [8, 9].
Recently, the Dutch Colorectal Cancer Group published a study [14] evaluating the prognostic value of primary tumor resection as the first-line treatment in a retrospective review of the CAIRO and CAIRO2 phase 3 randomized clinical trial [15, 16]. The results showed a median survival rate of 13 months for the non-resection group versus 22–24 months in the resection group. These patients had not been randomized before excision of the primary tumor, and therefore, it can be questioned that the patients might not be comparable due to heterogeneity. Our group has observed that the 2-year survival rate for patients with intestinal obstruction due to stage IV CRC with unresectable metastasis who underwent resection of the primary tumor was better than patients without resection (39.3 vs. 10%) [17].
Other research groups have attempted to resolve this dilemma formulating different hypotheses. The National Surgical Adjuvant Breast and Bowel Project C-10 (NSABP C-10) hypothesized specifically if the addition of bevacizumab to standard FOLFOX regimen increased the number of complications in patients with stage IV CRC without resection of the primary tumor [18]. The results showed that only 14% of patients presented major complications (e.g., obstruction, perforation, hemorrhage), and the authors concluded that non-resection of the primary tumor resulted in an acceptable rate of complications. Furthermore, they highlighted that survival was not compromised by leaving the primary tumor “in situ.” More recently, a clinical trial carried out at University College London Hospitals has been completed but results are still unpublished [19]. The primary objective of the trial was to assess whether overall survival in patients with asymptomatic stage IV CRC with unresectable metastasis is higher in patients treated with chemotherapy alone or with resection of the primary tumor plus chemotherapy (ClinicalTrials.gov identifier: NCT01086618). The effectiveness of resection of primary tumor in patients with stage IV CRC is currently a focus of great interest, and various clinical trials are underway.
Due to the lack of homogeneity of the groups compared or to the design limitations of previous studies, the dilemma and the debate are still open: Do patients benefit from the resection of the primary tumor in asymptomatic stage IV CRC with unresectable metastasis with regard to survival or quality of life, or is there no benefit?
The experience of the research group that includes Excellence Centers in Colorectal Surgery at the Spanish national level allows us to develop the present project. Considering the increase in incidence and prevalence of colorectal cancer and the important percentage of patients that are diagnosed at stage IV with unresectable metastases, the answer to the study question proposed seems very relevant. It could add evidence to a controversial area with a high impact from both clinical and societal perspectives.
Methods/design
This is a multicenter, parallel group, randomized trial. Eligible participants are randomized in a 1:1 allocation ratio to one of two arms: an intervention arm, in which the participants undergo surgical resection of the primary tumor before systemic chemotherapy, and a control arm, in which they receive systemic chemotherapy only.
Hypothesis and objectives
The conceptual hypothesis established is as follows: surgical resection of the primary tumor in patients with stage IV CRC with synchronous unresectable metastases can improve cancer-specific survival at 2 years as compared with treatment with systemic chemotherapy only without removal of the primary colorectal tumor. The operative hypothesis states that surgical resection of the primary tumor in patients with stage IV CRC with synchronous unresectable metastases will be associated with a 14% increase in 2-year cancer-specific survival rate in comparison to patients receiving systemic chemotherapy without primary tumor resection (2-year cancer-specific survival 34 vs. 20%).
The main objective of the study is to assess the impact on 2-year cancer-specific survival of two different strategies for the treatment of patients with stage IV CRC with unresectable metastases: resection of the primary tumor followed by systemic chemotherapy versus systemic chemotherapy alone without resection of the primary tumor. Secondary objectives include the following: (1) to assess the impact of the two different strategies for the treatment of patients with stage IV CRC with unresectable metastases on the quality of life and on the overall survival rate; (2) to report postoperative morbidity in patients assigned to the arm of surgical resection of the primary tumor; (3) to report complications and the need for surgery in patients assigned to the arm of systemic chemotherapy only; (4) to report systemic chemotherapy-related complications, including short- and medium-term toxicity; and (5) to assess overall survival and to identify prognostic factors for survival.
Study setting and participants
Patients will be recruited at 22 Colorectal Surgery Units and Medical Oncology Departments of acute-care tertiary hospitals and oncology centers throughout Spain. All institutions belong to the Spanish Public Health Care System.
Inclusion criteria
Eligible participants include (i) age ≥18 years; (ii) adenocarcinoma of the colon or rectum above 12 cm from the anal verge with histopathologic confirmation and radiologically resectable tumors assessed by computed tomography (CT) scan or magnetic resonance imaging (MRI) studies; (iii) radiological confirmation of synchronous unresectable metastases; (iv) absence of peritoneal carcinomatosis or central nervous system (CNS) or bone metastasis; (v) Eastern Cooperative Oncology Group (ECOG) performance status ≤2; (vi) absence of primary tumor-related complications requiring emergency surgery except for intestinal obstruction amenable to treatment using a self-expanding endoluminal stent; (vii) no contraindications for systemic chemotherapy with a leukocyte count ≥4.0 × 109/L, platelet count ≥100 × 109/L, renal clearance ≥50 mL/min, serum bilirubin <35 μmol/L, and clinically acceptable serum hemoglobin levels; (viii) not pregnant or breastfeeding; (ix) possibility of follow-up; and (x) signed informed consent.
Exclusion criteria
Patients with (i) rectal tumors below 12 cm from the anal verge or locally advanced tumors invading blood vessels, nerves, or bone; (ii) multiple bone or CNS metastases; (iii) other neoplastic disease in the 5 previous years, except squamous or basal cell skin carcinoma or cervical “in situ” carcinoma; (iv) significant heart disease (chronic congestive heart failure, symptomatic coronary disease) or myocardial infarction in the previous 6 months; (v) peripheral neuropathy; and (vi) patients who do not give informed consent will not be eligible to participate in the study.
Informed consent and legal considerations
The trial is conducted in accordance with the Declaration of Helsinki (7th revision) and the Spanish laws and regulations for biomedical research, with authorization from the Spanish Agency for Medicines and Medical Devices (Agencia Española del Medicamentos y Productos Sanitarios, AMPES). The trial protocol, patient information, and informed consent sheets have been approved by the competent Ethics Committees of all participating trial centers. The trial has been registered at the ClinicalTrials.gov database (NCT02015923; https://clinicaltrials.gov).
All eligible patients will individually be given an initial verbal description of the proposed study, and interested individuals will then be presented a written informed consent form. A signature will be obtained from all those who consent to participate by one of the investigators or a representative at each study center. During the trial, patients will be identified solely by an individual identification code. Trial findings will be stored in accordance with Spanish data protection law (Law 15/1999 on the protection of personal data) and will be handled in strictest confidence. For protection of these data, organizational procedures are implemented to prevent distribution of data to unauthorized people.
Trial interventions
Surgical resection of the primary tumor before systemic chemotherapy
Patients in the experimental arm will undergo complete resection of the primary tumor performed according to standard surgical techniques at the discretion of the executing surgeon, with achievement of a curative resection (R0 resection) prior to receiving systemic chemotherapy. Surgery has to be performed within 2 weeks after randomization. Systemic chemotherapy should be started after the patient’s discharge from the hospital following recommended regimens at each center. There is no predefined protocol of systemic chemotherapy.
Control arm: systemic chemotherapy without resection of the primary tumor
Patients in the control arm receive primary systemic chemotherapy without previous resection of the primary tumor. The executing medical oncologist at each center determines patient’s treatment. There is no predefined protocol of systemic chemotherapy.
Patients will be withdrawn from the study in two circumstances: if requested by the patient or if during treatment, the patient’s metastatic disease responds according to Response Evaluation Criteria in Solid Tumors (RECIST) [20]. In these cases, treatment of metastases will be reevaluated by the CRC multidisciplinary team.
Study endpoints
The primary efficacy endpoint is 2-year cancer-specific survival defined as the time from randomization date to the date of death due to CRC. Patients who have not died by the end of follow-up will be censored at their last contact data, as will be those patients who will be withdrawn from the study for a reason other than death.
The secondary endpoint was the patient’s quality of life. Quality of life is measured using questionnaires developed by the European Organization for Research and Treatment of Cancer (EORTC), including the EORTC QLQ-C30 instrument and the specific module CR29 [21].
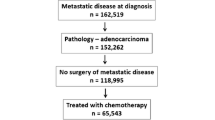
Trial implementation
Each Colorectal Surgery Unit of the participating hospitals treats between 150 and 300 cases of CRC patients a year, with a 20% probability of stage IV at initial clinical presentation. Recruitment period will last 1 year. The selection period will last a maximum of 21 days after diagnosis. Patients will be evaluated for eligibility by a multidisciplinary team composed of different specialists involved in the treatment of CRC. Before starting any procedure related to the study, written informed consent will be obtained. After screening for eligibility and informed consent is obtained, patients are randomized in a 1:1 ratio into the surgical resection plus systemic therapy arm, or systemic therapy alone (control arm). Patients will be randomized using computer-generated random numbers (R program; R Foundation for Statistical Computing). The patient will be informed of the results of randomization.
To assess patient’s inclusion in the study, the following data are necessary: medical history; complete physical examination including body weight, height, and blood pressure; ECOG performance status score; colonoscopy with tumor biopsy; thoracoabdominal CT examination with intravenous contrast and/or MRI of the liver and/or the pelvis; positron emission tomography-computed tomography (PET-CT) (only in case of doubt); and laboratory tests including complete blood count, coagulation tests, liver function tests, renal function tests, and tumor markers (CAE and CA 19.9). Patients assigned to the arm of surgical resection of the primary tumor are also evaluated by the anesthesiologist to assess American Society of Anesthesiologists (ASA) Physical Status classification.
Besides the baseline visit at the time the patient will start treatment according to random allocation to either study arm, eight follow-up visits are scheduled at 12, 26, 30, 52, 66, 80, 92, and 104 weeks after the baseline visit. In patients with favorable clinical or radiological response following the RECIST criteria [20], the CRC multidisciplinary team will reevaluate treatment possibilities, and the patient will be withdrawn from the study.
Sample size
Based on the results from the CAIRO study [14] in which resection of the primary tumor was a prognostic factor for survival, with a 2-year survival rate of 34% in the resection group versus 20% in the non-resection group, it was estimated that in the arm of tumor resection, the 2-year survival would increase approximately by 14% (from 20 to 34%). This increase is considered clinically relevant and achievable. Accepting a type I error of 0.05 and a type II error lower than 0.2 in a two-tailed test, a sample of 157 patients in each study group will be needed, with a total of 346 patients (173 in each group) to account for a lost to follow-up rate of 10%.
Statistical analysis
Analysis of the primary efficacy endpoint will be conducted in the intention-to-treat (ITT) data set, which includes all randomized patients analyzed in the treatment group in which they are allocated to by randomization. Analysis of the per-protocol (PP) data set will be performed as a secondary analysis. The safety analysis will be based on all randomized patients who will be treated with any of the interventions under investigation. Frequency and percentages of toxicity will be reported according to Common Terminology Criteria for Adverse Events (CTCAE) (version 4.0).
Descriptive methods will be used to present the distribution of variables in the study groups, with frequencies and percentages with the corresponding 95% confidence interval (CI) for categorical variables, and mean and standard deviation (SD) or median and interquartile range (25th–75th percentile) for quantitative variables. The chi-square test or the Fisher’s exact probability test will be used for the comparison of categorical variables, and the Student’s t test or the Mann-Whitney U test for the comparison of continuous variables according to the conditions of application (normal or non-normal distribution of data). For the primary efficacy endpoint, the difference in the proportion of survivors above 2 years between the study groups with the 95% CI will be calculated. For the secondary efficacy endpoint, differences in the mean scores of the quality of life questionnaires between the study groups at each follow-up visit will be calculated.
A binary logistic regression model will be adjusted, considering survival at ≥2 years (yes/no) as the dependent variable, and statistically significant variables (P < 0.05) in the bivariate analysis, clinically significant variables, and possible confounding factors as the independent variables. Cancer-specific and overall survival curves at 2 years will be calculated using the Kaplan-Meier method. Survival curves are compared with the log-rank test. Hazard ratios (HR) and 95% CI will be calculated using a Cox regression analysis.
Interim analysis
An interim analysis of safety data at 1 year after beginning of the study is planned. This analysis will include chemotherapy-related toxicity, morbidity after resection of the primary tumor, and mortality during treatment, which will be also extended to other variables considered to be of interest. Statistically significant differences in the interim analysis will determine premature discontinuation of the trial. All analyses will be done using Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 15.0 for Windows.
Discussion
The present clinical trial is designed to provide evidence of the effectiveness of two treatment approaches in patients with stage IV CRC with synchronous unresectable metastases (excluding bone and CNS metastases), that is, systemic chemotherapy alone versus resection of the primary tumor followed by systemic chemotherapy. Despite impressive progress in the use of chemotherapy with targeted agent and radical surgical procedures [22], the optimal management of CRC patients with metastatic disease not amenable to curative surgery, presenting without severe symptoms related to the primary tumor, remains controversial. It has been recognized that prospective randomized trials are required to define the oncologic outcome of resection versus no resection prior to systemic therapy in the setting of IV CRC synchronous metastatic disease [8, 9, 23, 24]. Results obtained in the present randomized multicenter trial together with those of other ongoing trials [25] will add evidence to clarify the most adequate treatment strategy in terms of patient-centered benefits and to form a budget perspective to the healthcare systems and the society in general.
Stage IV CRC with synchronous unresectable metastasis disease is a relevant problem with high social impact. According to the International Agency for Research on Cancer, in the year 2015 in Spain there will be over 3800 patients with this disease, and therefore, an increasing health problem due to the increase in survival of these patients already observed in the last few years may be foreseeable. Scientific evidence for decisions regarding treatment is currently based on data provided by a number of retrospective and non-randomized studies with limited external validity due to bias in the selection of patients and lack of homogeneous study groups. Therefore, the benefits obtained by the present randomized multicenter study, defining better treatment standards in this heterogeneous patient population and in which management is still controversial, are clinically relevant. In addition, results of randomized studies are necessary to build solid scientific evidence for the design of systematic reviews, meta-analyses, and cost-effectiveness studies, as well as to develop consensus recommendations and clinical practice guidelines.
Conclusion
The present randomized multicenter study evaluates the efficacy of primary tumor resection as compared with no resection in patients with stage IV CRC with synchronous unresectable metastatic disease. These patients do not suffer from local symptoms of the primary tumor. Results of this trial will contribute to define whether surgical removal of the primary tumor before systemic therapy is a better treatment strategy for these patients, and will help to optimize the management of CRC patients who are not amenable to any treatment modality with curative intent.
References
Poultsides GA, Paty PB (2011) Reassessing the need for primary tumor surgery in unresectable metastatic colorectal cancer: overview and perspective. Ther Adv Med Oncol 3:35–42. doi:10.1177/1758834010386283
Treatment of colon cancer, by stage. American Cancer Society. Available at: https://www.cancer.org/cancer/colon-rectal-cancer/treating/by-stage-colon.html. Accessed date: April 17, 2017
Gervaz P, Rubbia-Brandt L, Andres A, Majno P, Roth A, Morel P, Mentha G (2010) Neoadjuvant chemotherapy in patients with stage IV colorectal cancer: a comparison of histological response in liver metastases, primary tumors, and regional lymph nodes. Ann Surg Oncol 17:2714–2719. doi:10.1245/s10434-010-1056-6
Poultsides GA, Servais EL, Saltz LB, Patil S, Kemeny NE, Guillem JG, Weiser M, Temple LK, Wong WD, Paty PB (2009) Outcome of primary tumor in patients with synchronous stage IV colorectal cancer receiving combination chemotherapy without surgery as initial treatment. J Clin Oncol 27:3379–3384. doi:10.1200/JCO.2008.20.9817
Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Alberts SR (2004) A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 22:23–30
Giantonio BJ, Catalano PJ, Meropol NJ, O’Dwyer PJ, Mitchell EP, Alberts SR, Schwartz MA, Benson AB 3rd (2007) Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol 25:1539–1544
Saltz LB, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzén F, Cassidy J (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26:2013–2019. doi:10.1200/JCO.2007.14.9930
Stillwell AP, Buettner PG, Ho YH (2010) Meta-analysis of survival of patients with stage IV colorectal cancer managed with surgical resection versus chemotherapy alone. World J Surg 34:797–807. doi:10.1007/s00268-009-0366-y
Stillwell AP, Ho YH, Veitch C (2011) Systematic review of prognostic factors related to overall survival in patients with stage IV colorectal cancer and unresectable metastases. World J Surg 35:684–692. doi:10.1007/s00268-010-0891-8
Sarela AI, Guthrie JA, Seymour MT, Ride E, Guillou PJ, O’Riordain DS (2001) Non-operative management of the primary tumour in patients with incurable stage IV colorectal cancer. Br J Surg 88:1352–1356
Scoggins CR, Meszoely IM, Blanke CD, Beauchamp RD, Leach SD (1999) Nonoperative management of primary colorectal cancer in patients with stage IV disease. Ann Surg Oncol 6:651–657
Stelzner S, Hellmich G, Koch R, Ludwig K (2005) Factors predicting survival in stage IV colorectal carcinoma patients after palliative treatment: a multivariate analysis. J Surg Oncol 89:211–217
Karoui M, Roudot-Thoraval R, Mesli F, Mitry E, Aparicio T, DesGuetz G, Luvet C, Landi B, Tiret E, Sobhani I (2011) Primary colectomy in patients with stage IV colon cancer and unresectable distant metastases improves overall survival: results of a multicentric study. Dis Colon rectum 54:930–938. doi:10.1097/DCR.0b013e31821cced0
Venderbosch S, de Wilt JH, Teerenstra S, Loosveld OJ, van Bochove A, Sinnige HA, Creemers GJM, Tesselaar ME, Mol L, Punt CJA, Koopman M (2011) Prognostic value of resection of primary tumor in patients with stage IV colorectal cancer: retrospective analysis of two randomized studies and a review of the literature. Ann Surg Oncol 18:3252–3260. doi:10.1245/s10434-011-1951-5
Koopman M, Antonini NF, Douma J, Wals J, Honkoop AH, Erdkamp FL, de Jong RS, Rodenburg CJ, Vreugdenhil G, Loosveld OJ, van Bochove A, Sinnige HA, Creemers GJ, Tesselaar ME, Slee PH, Werter MJ, Mol L, Dalesio O, Punt CJ (2007) Sequential versus combination chemotherapy with capecitabine, irinotecan, and oxaliplatin in advanced colorectal cancer (CAIRO): a phase III randomised controlled trial. Lancet 370:135–142
Tol J, Koopman M, Rodenburg CJ, Cats A, Creemers GJ, Schrama JG, Erdkamp FL, Vos AH, Mol L, Antonini NF, Punt CJ (2008) A randomised phase III study on capecitabine, oxaliplatin and bevacizumab with or without cetuximab in first-line advanced colorectal cancer, the CAIRO2 study of the Dutch Colorectal Cancer Group (DCCG). An interim analysis of toxicity. Ann Oncol 19:734–738. doi:10.1093/annonc/mdm607
Frago R, Kreisler E, Biondo S, Salazar R, Dominguez J, Escalante E (2010) Outcomes in the management of obstructive unresectable stage IV colorectal cancer. Eur J Surg Oncol 36:1187–1194. doi:10.1016/j.ejso.2010.09.005
National Surgical Adjuvant Breast and Bowel Project (NSABP) 2010. Federally-Supported Clinical Trials: Protocol C-10,9/10 update. Available at: http://www.nsabp.pitt.edu/C10_Information.asp. Accessed date: April 17, 2017.
Chemotherapy with or without surgery in treating patients with metastatic colorectal cancer that cannot be removed by surgery. ClinicalTrials.gov Identifier: NCT01086618. Available at: https://clinicaltrials.gov/. Accessed date: April 17, 2017.
Miller AB, Hoogstraten B, Staquet M, Winkler A (1981) Reporting results of cancer treatment. Cancer 47:207–214
Arraras JI, Suárez J, Arias de la Vega F, Vera R, Asín G, Arrazubi V, Rico M, Teijeira L, Azparren J (2011) The EORTC Quality of Life questionnaire for patients with colorectal cancer: EORTC QLQ-CR29 validation study for Spanish patients. Clin Transl Oncol 13:50–56. doi:10.1007/s12094-011-0616-y
Nordlinger B, Van Cutsem E, Gruenberger T, Glimelius B, Poston G, Rougier P, Sobrero A, Ychou M (2009) Combination of surgery and chemotherapy and the role of targeted agents in the treatment of patients with colorectal liver metastases: recommendations from an expert panel. Ann Oncol 20:985–992. doi:10.1093/annonc/mdn735
Clancy C, Burke JP, Barry M, Kalady MF, Calvin Coffey J (2014) A meta-analysis to determine the effect of primary tumor resection for stage IV colorectal cancer with unresectable metastases on patient survival. Ann Surg Oncol 21:3900–3908. doi:10.1245/s10434-014-3805-4
Eisenberger A, Whelan RL, Negut AI (2008) Survival and symptomatic benefit from palliative primary tumor resection in patients with metastatic colorectal cancer: a review. Int J Color Dis 23:559–568
Rahbari NN, Lordick F, Fink C, Bork U, Stange A, Jäger D, Luntz S, Englert S, Rossion I, Koch M, Büchler M, Kieser M, Weitz J (2012) Resection of the primary tumor versus no resection prior to systemic therapy in patients with colon cancer and synchronous unresectable metastases (IUCC stage IV): SYNCHRONOUS—a randomised controlled trial (ISRCTN30964555). BMC Cancer 12:142
Acknowledgments
We thank Marta Pulido, MD, for editing the manuscript and editorial assistance and Bernat Miguel, project manager of the study.
The study is monitored by Scienco Klinico http://www.sciencoklinico.com/
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
The trial is conducted in accordance with the Declaration of Helsinki (7th revision) and the Spanish laws and regulations for biomedical research, with authorization from the Spanish Agency for Medicines and Medical Devices (Agencia Española del Medicamentos y Productos Sanitarios, AMPES). The trial protocol, patient information, and informed consent sheets have been approved by the competent Ethics Committees of all participating trial centers. The trial has been registered at the ClinicalTrials.gov database (NCT02015923; https://clinicaltrials.gov).
Funding
Instituto Carlos III, FIS PI12/02246 Ministry of Economy Industry and Competitiveness. Government of Spain.
Appendix
Appendix
CR4 Spanish study group:
Mercedes Villacampa, Instituto Catalan de Oncología
Eduardo Garcia-Granero Hospital La Fe
Laura Mora López, Corporació Sanitària Parc Taulí
Ignasi Camps, Hospital Germans Trias i Pujol
Miguel Pera, Hospital del Mar
Lorenzo Viso, Hospital Moisès Broggi
Elena Córdoba , Hospital Clínico Lozano Blesa
David Julià, Hospital Josep Trueta
Nieves Cáceres, Complejo Hospitalario de Vigo
Mario Álvarez, Hospital La Paz
José María Enríquez Navascués, Adelaida La Casta, Hospital Donostia
Fernando de la Portilla, Ana M García , Hospital Virgen del Rocío
Miguel Ángel Ciga, Hospital Virgen del Camino
José Luís Sánchez, Hospital Vall d’Hebron
Manuel Ferrer, Complejo Hospitalario Torrecárdenas
Jesús Abrisqueta, Hospital Virgen de la Arrixaca
Alberto Parajó, Complejo Hospitalario Ourense
Carlos Moreno, Complejo Hospitalario La Mancha Centro
Alejandro Espí, Hospital Clínico de Valencia
Rights and permissions
About this article
Cite this article
Biondo, S., Frago, R., Kreisler, E. et al. Impact of resection versus no resection of the primary tumor on survival in patients with colorectal cancer and synchronous unresectable metastases: protocol for a randomized multicenter study (CR4). Int J Colorectal Dis 32, 1085–1090 (2017). https://doi.org/10.1007/s00384-017-2827-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2827-3