Abstract
Introduction
The aim of this study was to assess the impact of diabetes mellitus, Crohn’s disease, HIV/aids, and obesity on the prevalence and readmission rate of perianal abscess.
Methods
The study cohort was based on the Swedish National Patient Register and included all patients treated for perianal abscess in Sweden 1997–2009. The prevalence and risk for readmission were assessed in association with four comorbidity diagnoses: diabetes mellitus, Crohn’s disease, HIV, and/or AIDS and obesity.
Results
A total of 18,877 patients were admitted during the study period including 11,138 men and 4557 women (2.4:1). Crohn’s disease, diabetes, and obesity were associated with a significantly higher prevalence of perianal abscess than an age- and gender-matched background population (p < 0.05). In univariate analysis, neither age nor gender had any significant impact on the risk for readmission. In a multivariate Cox proportional hazard analysis, Crohns disease was the only significant risk factor for readmission of perianal abscess.
Conclusion
Crohn’s disease, diabetes, and obesity increase the risk for perianal abscess. Of these, Crohn’s and HIV has an impact on readmission. The pathogenesis and the influence of diabetes and obesity need further research if we are to understand why these diseases increase the risk for perianal abscess but not its recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perianal abscess is a benign but common condition that may cause patients substantial discomfort. It seems reasonable to believe that recurrence of abscess and readmission are preventable if the disease is adequately treated at the initial intervention [1].
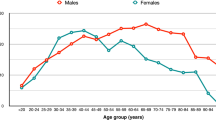
Previous studies have identified a number of risk factors for perianal abscess including smoking, HIV, and other conditions known to compromise the immune system such as inflammatory bowel disease, and patients with diabetes and obesity [2, 3]. The prevalence of perianal abscess is higher in men, and younger people have a higher risk than older [2]. Age under 40 has been suggested as a risk factor for recurrence [4]. Crohn’s disease is highly associated with intersphincteric abscess formation [5]. Perianal abscess is a relatively common condition, but in the field of research, it is not well explored, and the literature provides only few relatively dated studies.
One Swedish study has shown an annual incidence of 20/100 000 [6], and a similar incidence level has been reported from Germany [7]. The true incidence may be higher as patients with this condition probably do not always seek medical advice, and smaller abscesses may regress or drain spontaneously. We need more knowledge about perianal abscess and its risk factors if we are to provide optimal evidence-based treatment.
The aim of this study was to assess the prevalence and recurrence rate for perianal abscess in the Swedish population with special focus on the following risk factors: diabetes, Crohn’s disease, HIV, and obesity.
Material and methods
The study cohort constituted all patients diagnosed and treated for perianal abscess in Sweden 1997–2009, identified with the ICD code K61.0 in the NPR (The National Patient Register). The NPR includes all medical diagnoses according to ICD 10 at all hospitals in Sweden (http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish ). Registration during the study period was only complete for in-patient episodes and thus in-hospital care was a requisite for inclusion. This study was approved by the regional ethics committee in Stockholm, 2009/1787-31.
The prevalence and risk for readmission were assessed with regard to four comorbidity diagnoses: diabetes mellitus (ICD codes E10-E14), Crohn’s disease (K50), HIV and/or AIDS (B20-B24), and obesity (E66). Obesity is not specified in the ICD-code system but the WHO definition of obesity is a body mass index (BMI) exceeding 30. The prevalence was calculated by dividing the total number of primary perianal abscesses by the size of the population over the years 1997–2009. Population data were taken from Statistics Sweden.
Statistics
The relative risk for being admitted with a perianal abscess was determined by the ratio between the percentage of persons with an ICD code for each disease explored (diabetes mellitus, Crohn’s disease, HIV/AIDS, and obesity) among in-patients with the diagnosis perianal abscess (based on the ICD code), and the percentage of persons with an ICD code for those diseases (diabetes mellitus, Crohn’s disease, HIV/AIDS and obesity) in the Swedish background population stratified for gender and age in 5-year strata.
All patients were followed from their first admission for perianal abscess (ICD code K61.0-K61.4) until a second admission for recurrence or death. Patients were censored at the end of follow-up (December 31, 2009). The risk for recurrence (readmission) was assessed using Cox proportional hazards analysis. Age, gender, and comorbidity were included in the analysis as covariates. Age was dichotomized as above or below median (42 years). Readmission for perianal abscess was analyzed as an event and death or end of follow-up as censoring events. All analyses were performed with SPSS 17.0 (Chicago, Ill).
Results
Incidence
A total of 18,877 patients were admitted during the study period, including 11,138 (59 %) men and 4557 (24 %) women (2.4:1). Data on gender were missing in 3182 (17 %) cases. The incidence was 16.1 per 100,000 Swedish inhabitants per year. Mean age was 42 years for men (SD 18 years) and 42.5 years for women (SD 17 years). The difference was significant, p = 0,004.
Comorbidity
Diabetes was recorded prior to or at the time of the first admission for perianal abscess in 755 (6 %) of the patients, Crohn’s disease in 547 (4.3 %), HIV and/or AIDS in 26 (0.21 %), and obesity in 187 (1.5 %) of the patients. The prevalence of diabetes mellitus, Crohn’s disease, and obesity was significantly higher among patients with perianal abscess than in the general population (Table 1).
Risk for readmission
Only Crohn’s disease was seen as a significant risk factor for readmission (Table 2). The cumulative readmission rates for perianal abscess for each disease investigated are shown in Figs. 1, 2, 3, 4 and 5.
Discussion
This population-based study showed that diabetes, obesity, and Crohn’s disease are risk factors for developing a perianal abscess. It was confirmed that abscesses are more common among men, and that they are more common among younger than among older people. The reason for the association with gender and age is still unknown, but could be explained either by anatomical differences in the anal glands or hormonal factors. Even if the incidence was higher among men and younger people, there was no association between age or gender and recurrence rate. The cohort includes 17 % where data on gender is not known. This is mainly explained by the fact that immigrants are still not registered as residents and visiting guests who are not Swedish citizens do not have a complete personal number (possible to use for gender identification).
Previous studies have failed to show any association with environmental factors apart from smoking [3], it is therefore reasonable to believe that the predominance in males and younger people is caused either by smoking habits or is related to anatomical circumstances or hormones, rather than exposure to external factors such as lifestyle.
A weakness in this study is that it is based on registry data on medical diagnoses according to ICD 10. The results are therefore dependent on the accuracy of the register. However, the NPR has been reviewed, showing a high validity for most of the inpatient diagnoses [8]. All patients can be traced from the first admission, regardless of which unit recurrent admissions are registered. The national coverage with almost 100 % completeness of the NPR makes the present study population-based [8].
The Patient Registry at the National Board of Health and Welfare has been confirmed to have a very high validity for the main diagnosis and for the accuracy of secondary diagnoses whereas the completeness of registration of secondary diagnosis is somewhat lower and partly dependent on the dignity.
A group of patients with increased risk of perianal abscess are those with acute leukemia [9, 10] and those with hematological diseases who undergo stem cell transplantation [11]. This alteration in the immune system may be of the same principle as in the risk groups identified in this present study [12]. Whether it is just an unspecific suppression of the immune system or an alteration in a specific T cell subgroup cannot be answered in this study.
Diabetes
The present data demonstrate that patients with diabetes have an increased risk for perianal abscess but not for recurrent disease. There are several possible explanations why diabetic patients are prone to develop a primary abscess, without an increased risk for recurrence. One might be the influence of lifestyle. When patients are diagnosed with diabetes, a specialized treatment team gives advice on suitable changes in lifestyle. If successful, patients may, for example, lose weight and thus the risk for recurrence might decrease as a result of this intervention. It is also possible that the pathophysiology behind the index and recurrent abscess differs [4].
Previous studies indicate that the relationship between diabetes and perianal abscess is complex. It has been demonstrated that perianal abscesses are associated with a risk for developing type 2 diabetes within 5 years of diagnosis [7]. It could be possible that perianal abscess predisposes to diabetes. Another study found that non-diabetic patients actually have a higher risk than diabetics for recurrent perianal complaints [4]. There may thus be confounders related to lifestyle such as obesity and smoking [2, 3] that partly explain the association between diabetes and perianal abscess.
Hyperglycaemia is a well-known risk factor predisposing to soft tissue infection. Poor immunological response, impaired microcirculation due to atherosclerosis, and fibroblast dysfunction are some possible mechanisms for the increased risk for soft tissue infection in patients with poor glycemic control [13]. It cannot be ruled out that the autoimmune component in diabetes type 1 may act as confounder. Since it was impossible to distinguish between type 1 and type 2 diabetes due to the design of our database, we cannot rule out overrepresentation of patients with type 1 diabetes in this study.
Obesity
Obese patients have an increased risk for developing a perianal abscess when compared to the general population. Many questions regarding the relationship between obesity and perianal abscesses remain unanswered. The present results show that the initial risk for recurrence is equivalent to the background population, but with time (about 3 years), there is a rather dramatic increase in the frequency of perianal abscess recurrence among obese patients (Fig. 2). Type 2 diabetes and obesity are conditions highly associated with lifestyle [14]. The second graph (Fig. 3) illustrates what happens when patients with diabetes in this study are excluded from the obesity group. The curve appears completely different with no increase in recurrence rate over time. This implies that it is not obesity per se but the diabetic condition behind that explains the increase in recurrence after 3–5 years.
This result is congruent with previous findings that there is an increased risk for developing diabetes if a person is admitted to hospital with a perianal abscess [2]. The period required for obesity to have an impact on overall health might be somewhat longer. The possibility remains, therefore, that obesity is an important risk factor. The fact that obesity impairs wound healing and predisposes to subcutaneous infection is well known. However, as pointed out by Pierpont [15], knowledge is lacking about the mechanisms involved with regard to obesity-related disease. General wound healing is impaired among obese patients, but it is not known if this is also true for the occurrence of perianal abscess.
Crohn’s disease
Patients with Crohn’s disease had a higher risk than the background population for developing a perianal abscess (Table 1, Fig. 4). Furthermore, the risk for recurrence of perianal abscess is higher among patients with Crohn’s disease. There is a documented and strong association between inflammatory bowel disease and perianal abscess and/or fistula [5]. Vigano et al., using anal ultrasound, showed that patients with Crohn’s disease often have abscesses that can be diagnosed early during the course of their illness. In some cases, these abscesses rapidly develop into fistulae. It is known that the perianal manifestation of Crohns disease gets worse when the disease is badly treated. We do not know if this is also true regarding perianal abscess.
The pathogenesis of anorectal abscess in patients with Crohn’s disease is not fully understood. Development of perianal abscess may have a different cause for patients in the general population than for patients with Crohn’s disease where an autoimmune component is more likely. There are also reasons to believe that such patients may develop anal fissures that penetrate the anorectal wall and eventually spread to the perirectal tissues. One conclusion following this might be that patients with Crohn’s disease should be treated more aggressively for anal fissure than others.
HIV
Patients in this group are immunocompromised and often in a poor condition due the treatment of the HIV infection. The prevalence of HIV is fairly low in Sweden (0.06/100,000). This makes it difficult to draw conclusions regarding HIV as a risk factor for perianal abscess. Most patients with HIV today are under medication, and the disease is under control; AIDS is thus not as common as 10–15 years ago. However, these patients are immunocompromised and it could be that the risk for recurrence is proportional to their immune status. As shown in Fig. 5, the re-occurrence rate is most frequent during the first 2 years after diagnosis.
Conclusion
In this population-based study, Crohn’s disease, diabetes, and obesity were found to be risk factors for the development of perianal abscess whereas HIV/aids was not. The association between perianal abscess and diabetes needs further research if it is to be understood. Crohn’s disease was associated with a higher risk for recurrence whereas diabetes and obesity were not. An important question is, to what extent are lifestyle and possible autoimmune mechanisms relevant and how do they interact in diabetic patients with a perianal abscess?
References
Benign Anorectal Diseases (2006) Diagnosis with endoanal and endorectal ultrasound; redigerad av Giulio Aniello Santoro, Giuseppe Di Falco. Springer-Verlag Italia, Turin
Po-Li Wei JJK, Kuo L-J, Lin H-C (2013) Increased risk of diabetes following perianal abscess: a population-based follow-up study. Int J Color Dis 28:235–240, 2012:235-40
Devaraj B, Khabassi S, Cosman BC (2011) Recent smoking is a risk factor for anal abscess and fistula. Dis Colon Rectum 54:681–685
Hamadani A, Haigh PI, Liu I-LA, Abbas MA (2009) Who is at risk for developing chronic anal fistula or recurrent anal sepsis after initial perianal abscess? Dis Colon Rectum 52(2):217–221
Vigano C, Losco A, Caprioli F, Basilisco G (2011) Incidence and clinical outcomes of intersphincteric abscesses diagnosed by anal ultrasonography in patients with Crohn’s disease. Inflamm Bowel Dis 17:2102–2108
Hamberger B, Kir HU (2009) Liber AB, 113 98 Stockholm
Andreas Ommer AH, Berg E, Furst A, Sailer M, Schiedeck T (2012) German S3 guideline: anal abscess. Int J Color Dis 27:831–837
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450
North JH Jr, Weber TK, Rodriguez-Bigas MA, Meropol NJ, Petrelli NJ (1996) The management of infectious and noninfectious anorectal complications in patients with leukemia. J Am Coll Surg 183:322–328
Chen CY, Cheng A, Huang SY, Sheng WH, Liu JH, Ko BS, Yao M, Chou WC, Lin HC, Chen YC, Tsay W, Tang JL, Chang SC, Tien HF (2013) Clinical and microbiological characteristics of perianal infections in adult patients with acute leukemia. PLoS One 8:e60624
Anabtawi I, Abdel-Rahman F, Al MM (2011) Surgical complications related to hematopoietic stem cell transplantation. Eur J Surg Oncol 37:576–582
Salazar R, Sola C, Maroto P, Tabernero JM, Brunet J, Verger G, Valenti V, Cancelas JA, Ojeda B, Mendoza L, Rodriguez M, Montesinos J, Lopez-Lopez JJ (1999) Infectious complications in 126 patients treated with high-dose chemotherapy and autologous peripheral blood stem cell transplantation. Bone Marrow Transplant 23:27–33
Casqueiro J, Casqueiro J, Alves C (2012) Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab 16(Suppl 1):S27–S36
Schwandner O (2011) Obesity is a negative predictor of success after surgery for complex anal fistula. BMC Gastroenterol 11
Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, Payne WG (2014) Obesity and surgical wound healing: a current review. ISRN Obes 2014:638936
Acknowledgments
The study was supported by a grant from the Olle Engqvist Research Foundation.
Author’s contribution
Karin Strigård and Karin Adamo contributed to the conception, design, and interpretation of data. Fredrik Brännström and Gabriel Sandblom contributed to the acquisition, analysis, and interpretation of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The manuscript does not contain clinical studies or patient data. The study was approved by the ethics review board of Stockholm, Sweden, 2009/1787-31.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Adamo, K., Sandblom, G., Brännström, F. et al. Prevalence and recurrence rate of perianal abscess—a population-based study, Sweden 1997–2009. Int J Colorectal Dis 31, 669–673 (2016). https://doi.org/10.1007/s00384-015-2500-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2500-7