Abstract
Introduction
Emergency surgery for colorectal cancer has been associated with high mortality. The aim of this study is to determine factors predictive of undergoing emergency surgery, of 30-day mortality, and explore the role of screening in patients undergoing emergency surgery.
Methods
All patients at our unit, undergoing surgery for colorectal cancer between 2004 and 2014 were included. Data on patient demographics, tumour staging, admission type, comorbidity score, mortality data, and screening data were analysed. Multivariable analyses were carried out to determine predictors of undergoing emergency surgery as well as mortality postoperatively.
Results
A total of 1911 consecutive patients underwent elective and emergency surgery for colorectal cancer. Of the 263 patients who underwent emergency surgery for CRC, 37.3 % (n = 98) had right-sided colonic cancers. Multivariable analyses determined right-sided cancers (OR 2.92, 95 % CI 2.03–4.20, p < 0.001) and stage IV tumours to be independently associated with undergoing emergency surgery (OR 6.64, 95 % CI 2.86–15.42, p < 0.001). Undergoing emergency surgery was an independent predictor of 30-day mortality (OR 9.62, 95 % CI 5.96–15.54, p < 0.001). Of the 50 patients that died within 30 days in the emergency surgery group, 32 % were in patients with right-sided colon cancers. Cancer detection through guaiac faecal occult blood testing (gFOBT) amongst this group is low with six out of nine patients having a false negative gFOBT test.
Conclusion
Emergency CRC surgery is associated with high mortality. Alternative screening strategies that improve detection of proximal colon cancers may reduce the number of patients undergoing emergency surgery for right-sided cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What does this paper add to the literature?
The number of patients with colorectal cancer attending hospital for emergency CRC surgery is high as is the 30-day mortality in this patient group. A large proportion of these patients have a right-sided cancer that is poorly detected through gFOBT.
Introduction
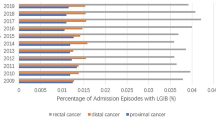
According to the 2012 National Bowel Cancer Audit, a quarter of Colorectal Cancer (CRC) patients are diagnosed following emergency presentation [1]. There is strong evidence that colorectal cancer patients presenting as an emergency have a high incidence of morbidity and tend to have poor long-term survival [2–4]. In various healthcare systems, colorectal cancer screening programmes have been established with the aim of identifying cancer patients at an early stage in the disease process. If successful, this strategy is likely to reduce the number of patients presenting as emergencies.
Despite such a screening programme in the UK, the proportion of patients presenting as an emergency has largely remained stable [1]. Several reasons for this have been proposed including impaired access to healthcare in remote areas, ethnicity, poor patient education, low participation rates in screening programs, as well as other lifestyle and health behavioural factors [5–7]. The aim of this study is to determine factors predictive of undergoing emergency surgery in CRC and explore the role of screening in this patient group.
Methods
An institutional colorectal cancer database of consecutive patients diagnosed between 2004 and 2014 was used to identify patients who had undergone primary surgical resection for colorectal cancer. Data were collected from medical coding, patient records, electronic pathology, and endoscopy and radiology reports. Relevant data variables included were age, sex, tumour staging (using the Union for International Cancer Control classification), admission type (elective or emergency), ethnicity and Charlson Comorbidity Score. Postcodes were used to obtain Indices of Multiple Deprivation (IMD) scores from the UK Office for National Statistics (ONS). The Office for National Statistics is a UK governmental body that is recognised as the official national statistics institute of the UK (http://www.ons.gov.uk/).
Emergency surgery was defined as patients undergoing unplanned surgery after admission through the Emergency Department or same day referral through primary care. Patients with a diagnosis of carcinoid tumour of the appendix, intestinal lymphoma, anal cancer or presentation with metachronous tumours from ovarian, bladder and prostate cancer were excluded. Data on complications (using the Clavien-Dindo classification [8]) and 30-day mortality rates were obtained.
Bowel cancer screening and cancer registry
In the UK, bowel cancer screening started as national program in 2006 and made available to all persons between the ages of 60 and 69 years. Our unit was one of the first to join the program and did so in October 2006. The modality for screening has been the guaiac Faecal Occult Blood Test (gFOBT). In this study, screening data was retrieved from our units Bowel Cancer Screening Centre. Data on tumour biology and survival data were corroborated with the regional cancer registry (Thames Cancer Registry). The Thames Cancer Registry covers a large area in south east England and is one of the largest cancer registries in the country. The registry contains data on tumour stage, tumour morphology, date of diagnosis, treatment modality, and mortality data. Data on all patients in this study were obtained via the registry, to corroborate the accuracy of our local data.
Statistical analysis
The independent variables of sex, age, Charlson Comorbidity Score, Union for International Cancer Control (UICC) tumour staging, tumour site (right colon, transverse colon, left colon, sigmoid colon, rectum, etc.), social deprivation and ethnicity were included in binary logistic univariable analysis. At the univariable level, variables that showed a significance level of <0.10 were entered into a multivariable model. Multivariable logistic regression models of the likelihood of emergency presentation, undergoing emergency surgery and death, were developed. A level of p ≤ 0.05 was considered significant. All statistics were calculated using IBM® SPSS®, Version 19.0.
Results
A total of 1911 patients (Table 1) were identified as having undergone surgery for colorectal cancer over the study period. The study population comprised of 1094 (57.2 %) males and 817 (42.8 %) females, with a median age of 68 years (range 18–96, interquartile range [IQR] 17). Between 2004 and 2014, 263 patients (13.8 %) underwent emergency (unplanned) surgery after being admitted through the hospital’s Emergency Department or referred the same day through primary care. Within the emergency surgery group (n = 236), patients with sigmoid tumours (37.3 %, n = 98/263) and right colon tumours (Ascending and Transverse colon, 35.4 %, n = 93/263) presented most frequently. In total, 16.4 % (n = 314/1911) of tumours were classified as stage I. Stages II, III and IV cancers accounted for 27.3 % (n = 521), 26.8 % (n = 513) and 5.3 % (n = 101), respectively. Tumour stage for a quarter of the patients (n = 462/1911) was unknown. The emergency surgery group had a higher rate of stage IV tumours (9.5 %, n = 25/264) compared with 4.6 % (n = 76/1648) in the elective surgery group (p < 0.001).
Social deprivation was measured using Indices of Multiple Deprivation (IMD) scores calculated from a patient’s postcode. IMD data were available on 1864 patients (97.5 % of the study population). There were 977 (51.1 %) patients in Q1 (affluent), 718 (37.6 %) in Q2, 146 (7.6 %) in Q3, and 23 in Q4 (1.2 %). There were no patients in the most deprived quintile (Q5), and in 2.5 % of the population (n = 47/1,911), the IMD score was unobtainable. Ethnicity data were available for 1631 patients (85.3 % of the population). The largest ethnic group in the database was ‘British & Irish White’, comprising 63.2 % (n = 698/1911) of the study population. Patients of ‘Asian’ (Indian/Pakistani/Bangladeshi) backgrounds were the second largest group (14.7 %, n = 280/1911) followed by ‘Afro-Caribbean/Black’ (n = 111, 5.8 %), ‘Middle Eastern/Arab’ (n = 22, 1.2 %) and ‘East Asian/Chinese’ (n = 11, 0.6 %). In 280 patients (14.7 %) of the population, the ethnicity was registered as ‘any other ethnic group’, or ethnicity data were unavailable.
Patients in the emergency surgery group were more likely to have bypass/defunctioning surgery only (i.e. patients that did not have a definitive surgical resection for cancer) compared with patients in the elective surgery group (16.0 % in emergency CRC surgery group compared with 4.8 % in the elective group, p < 0.001).
Predictors of undergoing emergency surgery
Univariable logistic regression was used to predict whether a colorectal cancer patient undergoing surgery had attended as an emergency (Table 2). Age, UICC tumour stage, tumour site and existing medical comorbidity (Charlson score) were statistically significant predictors in univariable analyses. These variables were included in multivariable analyses to produce a model predictive of emergency presentation and subsequent surgery for colorectal cancer.
At multivariable analysis, all of the above factors were independently associated with requiring emergency surgery for CRC. Elderly patients (80+ years) were more likely to require emergency CRC surgery (OR 1.65, 95 % CI 1.10–2.46, p = 0.015) compared with the reference group (18–59-year olds). Compared with the rectum, patients with right sided colon cancer (Ascending and Transverse colon) were nearly three times more likely to require emergency CRC surgery (OR 2.93, 95 % CI 2.03–4.20, p < 0.001). Increasing tumour stage was independently associated with undergoing emergency CRC surgery. Patients with stage IV tumours were over six times more likely to require emergency surgery than patients with stage I tumours (OR 6.65, 95 % CI 2.86–15.42, p < 0.001). Similarly, patients with more medical comorbidities (Charlson score >4) were 63 % more likely to undergo emergency surgery (OR 1.63, 95 % CI 1.63–1.81, p = 0.003).
Postoperative mortality (30 days)
The overall 30-day postoperative mortality was 4.3 % (n = 85/1911), although the rate was significantly higher in the emergency CRC group (19.0 %, n = 50/263) compared with the elective surgery group (2.0 %, n = 33/1,648, p < 0.001). Factors associated with postoperative mortality were surgery type (emergency or elective), age, ethnicity and comorbidity (Table 3). These variables were entered into a multivariable regression model. At multivariable analyses, emergency surgery, elderly age and existing medical comorbidity were independently associated with an increased risk of 30-day death. Patients undergoing emergency surgery were nearly 10 times more likely to die in the first 30 days postoperatively (OR 9.62, 95 % CI 5.96–15.54, p < 0.001) compared to patients undergoing elective surgery. Elderly patients (80+ years) were also at high risk of death (OR 3.23, 95 % CI 1.62–6.44, p = 0.001) compared to patients 18–59 years old. Having multiple comorbidities (Charlson comorbidity score >4) was associated with a 94 % increase (OR 1.94, 95 % CI 1.14–3.31, p = 0.015).
Screening
As part of the National Bowel Cancer Screening Programme (NBCSP), screening for CRC started at our unit in October 2006 and was available to all patients aged between 60 and 69 years of age. Screening was carried out using guaiac faecal occult blood testing (gFOBT) kits. Of the 263 patients that underwent emergency surgery, a total of 55 (20.9 %) were eligible for screening (Table 4). Of these 55, 81.8 % (n = 27/55) were invited for gFOBT screening, 7.3 % (n = 4/55) were not invited and 10.9 % (n = 6/55) were invited after having already attended and undergone emergency surgery. Amongst the 45 patients that were invited prior to attending as an emergency, 27 did not respond to the invitation and did not return their gFOBT sample (n = 27/45, 60.0 %).
Of the 18 patients that did respond, nine had a negative gFOBT and nine had a positive gFOBT. Of the nine that had a positive gFOBT, four went on to have colonoscopy (n = 4/9, 44.4 %) and were diagnosed with CRC. However, all were admitted as an emergency (two with bleeding, one with loose stools and one with bowel obstruction) before elective surgery could be undertaken. The other five that tested positive for gFOTB did not attend their colonoscopy invitation, and all attended with bleeding and/or obstruction within 9 months of screening date and had to have emergency CRC surgery. Of the nine that tested negative, six (n = 6/9, 66.7 %) were patients with caecal and proximal ascending colon. The remaining three that tested negative on gFOBT, one each, had descending, sigmoid colon and high rectal cancer (rectosigmoid junction).
Discussion
The main findings from this study are that elderly, comorbid patients as well as those with right-sided and advanced tumours are at increased risk of undergoing emergency CRC surgery. Furthermore, patients that undergo emergency surgery for CRC are at a 10-fold risk of dying within 30 days of surgery. We observed that patients with colonic tumours (especially right sided) were more likely to require emergency surgery compared with rectal tumours, a trend which has been observed in the literature. The study reiterates that the rate of emergency presentation remains a significant problem in the UK, with around 20–30 % of colorectal cancer being diagnosed during acute hospitalisation[9]. This patient group often presents in extremis, fluid deplete, physiologically unstable and overall at a poor baseline. The end result is a group of patients, often elderly, at high risk of poor perioperative outcome in terms of re-operation and 30-day mortality [10].
Emergency patients also tend to have a prolonged length of stay and lower overall 5-year survival compared with their age and tumour stage-matched counterparts [2]. Aside from the human cost, the financial burden on the healthcare services is substantial, with evidence to suggest that the relative cost of emergency surgery to be at least 1.5 times that of elective surgery [11]. One method that has been proposed to reduce the human and financial costs of emergency presentation is the use of self-expanding metal stents (SEMS) in the cases of bowel obstruction. Colonic stenting has been primarily used for distal colonic tumours, although in recent years, proximal colon stenting has also been carried out [12, 13]. However, reported results from SEMS vary in success, with reports of a 6–18 % failure rate quoted in the literature [14–16], as well as potential for serious complications [17]. While SEMS may reduce stoma rates, a meta-analysis by Tan and co-workers [18] has shown there to be no difference in rate of stoma formation, length of stay, surgical site infection or 30-day mortality compared with those who underwent emergency surgery without stenting. Importantly, SEMS was also found to have a significant rate of stent migration and perforation[19].
Detection of colorectal cancer through screening may lower or prevent poor outcome associated with late presentation. In 2006, the National HS rolled out the National Bowel Cancer Screening Program (NBCSP) with the primary goals of early diagnosis of colorectal cancer and reducing the proportion of emergency admissions. There is evidence that a well-functioning screening program has the potential to significantly lower the rate of emergency admissions [20]. However, data from the National Cancer Intelligence Network (NCIN) suggests that, despite screening, nearly a quarter (up to a third in those aged over 70 years) of colorectal cancer patients continue to be diagnosed upon attending as an emergency in England [21]. It seems logical that for a screening programme to be effective in this context, it should offer a population diagnosis of cancers at an earlier age when elective surgery carries lower mortality and morbidity risk. In our study, over half of the patients that presented as emergencies were over 75 years of age. Detecting colorectal cancer and treating patients earlier may confer significant population benefit if appropriate diagnostic screening tools are available. To this end, the usefulness of faecal occult blood testing in detecting right-sided cancer as well as the current age cut-off for screening demands questioning.
In the present study, over a third of the tumours in patients presenting as emergencies were either right-sided or transverse colonic tumours. A meta-analysis by Haug and colleagues has investigated whether gFOBT is useful in detecting right-sided colon cancers; patients suffering from this continue to make up one of the largest groups amongst emergency attenders [22]. Furthermore, work by the same author and colleagues has shown sensitivity of gFOBT in detecting right-sided cancers to be as low as 20 % [23] compared with 96 % detection rate with the use of colonoscopy [24]. For the population that currently present as emergencies to benefit from screening, it would be important to demonstrate that screening tests are able to detect proximal colonic tumours thereby permitting earlier intervention. One alternative may be the use of better techniques in the processing of gFOBT samples that would permit a greater capture of right-sided tumours. Blood-based screening tests, such as RNA biomarker panel tests, have been proven to be just as effective in detecting right-sided tumours compared with left-sided cancers [25] and could therefore provide an alternative approach.
In our study, 55 patients were eligible for screening; however, only 45 were invited. Lack of patient engagement with healthcare services (such as registering personal contact details with their local primary care General Practitioner) may offer some explanation as to why 10 patients were not invited. Another potential factor contributing to this seemingly low figure is that a further six patients were offered screening, albeit within a year after they presented as an emergency. Therefore, the timing of the invitation plays a role in capturing patients prior to their attendance. It must be stressed that the figures in our study must be interpreted with caution as the sample size is small. Our response rate to invitation for screening of 32.7 % (n = 18/55) is lower than the national average of 52 % [26]. Of the 45 patients offered screening, only 18 responded, nine of whom had a negative FOBT result only to present as an emergency within 14 months. Such ‘failures’ may occur due to a complex interaction of insensitivity of screening tool as well as social and differential healthcare access factors. In our study, the majority of the patients that did not participate in screening were male, a fact that is reflected in the literature [26]. Screening also continues to suffer from a relatively poor response rate amongst groups such as the elderly, ethnic minorities and the socially deprived [5]. A randomised control trial has demonstrated that rates of screening participation in both the socially deprived and ethnic minority groups can be increased through active public health intervention initiatives in the form of patient education [27]. The challenge may well be the initial capturing of the non-responding groups in the community, rather than difficulties in maintaining adherence to undergo additional investigations. Once screened, attendance for colonoscopy after a positive FOBT is generally good with little variation between different socioeconomic and ethnic groups [28].
Regardless of the particular screening technique used, a greater uptake of screening is required to reduce emergency presentations. Patient education, access to healthcare, cultural barriers and taboos to undergoing screening may offer some explanation as to why such a significant number of patients are still attending as emergencies [29]. In universal healthcare systems, such as the National Health Service (NHS) in the UK, it may be that the role of patient education, public awareness and patient health behaviours is a more important contributor to surveillance adherence than financial barriers. There is evidence to suggest that raising public awareness can increase participation in population screening [30].
Emergency presentation continues to make up a significant proportion of colorectal workload. Advanced tumour staging and site of colon remain important factors predicting emergency attendance. Given that colorectal cancer patients presenting in an emergency setting, in particular the elderly, have worse outcomes, an intensification of efforts to introduce and promote screening and surveillance, particularly amongst the elderly and socially deprived, is required.
References
Finan P., & Greenaway K. (2012). National Bowel Cancer Audit 2012
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. British J Surg 91(5):605–609. doi:10.1002/bjs.4456
Scott N. A., Jeacock J., & Kingston R. D. (1995) Risk factors in patients presenting as an emergency with colorectal cancer. British J Surg, 82(3), 321–3. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7795995
Anderson J. H., Hole D., & McArdle C. S. (1992) Elective versus emergency surgery for patients with colorectal cancer. British J Surg 79(7), 706–709. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1379508
Von Wagner C, Baio G, Raine R, Snowball J, Morris S, Atkin W, Wardle J (2011) Inequalities in participation in an organized national colorectal cancer screening programme: results from the first 2.6 million invitations in England. Int J Epidemiol 40(3):712–718. doi:10.1093/ije/dyr008
Whitaker KL, Good A, Miles A, Robb K, Wardle J, von Wagner C (2011) Socioeconomic inequalities in colorectal cancer screening uptake: does time perspective play a role? Health Psychol : Off J Division Health Psychol, Am Psychol Assoc 30(6):702–709. doi:10.1037/a0023941
Brouse CH, Basch CE, Wolf RL, Shmukler C (2004) Barriers to colorectal cancer screening: an educational diagnosis. J Cancer Educ : Off J Am Assoc Cancer Educ 19(3):170–173. doi:10.1207/s15430154jce1903_12
Dindo D., Demartines N., & Clavien P.-A. (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Anna Surg 240(2), 205–13. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1360123&tool=pmcentrez&rendertype=abstract
ACPGBI. (n.d.). National Bowel Cancer Audit 2012. Retrieved from http://www.hqip.org.uk/assets/NCAPOP-Library/NCAPOP-2012-13/Bowel-Cancer-Audit-National-Report-pub-2012.pdf
Clark AJ, Stockton D, Elder A, Wilson RG, Dunlop MG (2004) Assessment of outcomes after colorectal cancer resection in the elderly as a rationale for screening and early detection. British J Surg 91(10):1345–1351. doi:10.1002/bjs.4601
Jestin P, Nilsson J, Heurgren M, Påhlman L, Glimelius B, Gunnarsson U (2005) Emergency surgery for colonic cancer in a defined population. British J Surg 92(1):94–100. doi:10.1002/bjs.4780
Repici A, Adler DG, Gibbs CM, Malesci A, Preatoni P, Baron TH (2007) Stenting of the proximal colon in patients with malignant large bowel obstruction: techniques and outcomes. Gastrointest Endosc 66(5):940–944. doi:10.1016/j.gie.2007.04.032
Dronamraju SS, Ramamurthy S, Kelly SB, Hayat M (2009) Role of self-expanding metallic stents in the management of malignant obstruction of the proximal colon. Dis Colon Rectum 52(9):1657–1661. doi:10.1007/DCR.0b013e3181a8f4af
Williams D, Law R, Pullyblank AM (2011) Colorectal stenting in malignant large bowel obstruction: the learning curve. Int J Surg Oncol 2011:917848. doi:10.1155/2011/917848
Dauphine C. E., Tan P., Beart R. W., Vukasin P., Cohen H., & Corman M. L. (2002) Placement of self-expanding metal stents for acute malignant large-bowel obstruction: a collective review. Ann Surg Oncol 9(6), 574–9. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12095974
Keränen I, Lepistö A, Udd M, Halttunen J, Kylänpää L (2012) Stenting for malignant colorectal obstruction: a single-center experience with 101 patients. Surg Endosc 26(2):423–430. doi:10.1007/s00464-011-1890-z
Fernández-Esparrach G, Bordas JM, Giráldez MD, Ginès A, Pellisé M, Sendino O, Llach J (2010) Severe complications limit long-term clinical success of self-expanding metal stents in patients with obstructive colorectal cancer. Am J Gastroenterol 105(5):1087–1093. doi:10.1038/ajg.2009.660
Tan CJ, Dasari BVM, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. British J Surg 99(4):469–476. doi:10.1002/bjs.8689
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99(10):2051–2057. doi:10.1111/j.1572-0241.2004.40017.x
Scholefield J. H., Robinson M. H., Mangham C. M., & Hardcastle J. D. (1998) Screening for colorectal cancer reduces emergency admissions. Europ J Surg Oncol : J Europ Soc Surg Oncol British Assoc Surg Oncol 24(1), 47–50. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9542516
Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, Richards M (2012) Routes to diagnosis for cancer - determining the patient journey using multiple routine data sets. Br J Cancer 107(8):1220–1226. doi:10.1038/bjc.2012.408
Haug U, Knudsen AB, Brenner H, Kuntz KM (2011) Is fecal occult blood testing more sensitive for left- versus right-sided colorectal neoplasia? a systematic literature review. Expert Rev Mol Diagn 11(6):605–616. doi:10.1586/erm.11.41
Haug U, Kuntz KM, Knudsen AB, Hundt S, Brenner H (2011) Sensitivity of immunochemical faecal occult blood testing for detecting left- vs right-sided colorectal neoplasia. Br J Cancer 104(11):1779–1785. doi:10.1038/bjc.2011.160
Bressler B., Paszat L. F., Vinden C., Li C., He J., & Rabeneck L. (2004) Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology 127(2), 452–6. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15300577
Chao S, Ying J, Liew G, Marshall W, Liew C-C, Burakoff R (2013) Blood RNA biomarker panel detects both left- and right-sided colorectal neoplasms: a case–control study. J Experiment Clin Cancer Res : CR 32:44. doi:10.1186/1756-9966-32-44
Logan RFA, Patnick J, Nickerson C, Coleman L, Rutter MD, von Wagner C (2012) Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first 1 million tests. Gut 61(10):1439–1446. doi:10.1136/gutjnl-2011-300843
Lasser KE, Murillo J, Lisboa S, Casimir AN, Valley-Shah L, Emmons KM, Ayanian JZ (2011) Colorectal cancer screening among ethnically diverse, low-income patients: a randomized controlled trial. Arch Intern Med 171(10):906–912. doi:10.1001/archinternmed.2011.201
Morris S, Baio G, Kendall E, von Wagner C, Wardle J, Atkin W, Raine R (2012) Socioeconomic variation in uptake of colonoscopy following a positive faecal occult blood test result: a retrospective analysis of the NHS Bowel Cancer Screening Programme. Br J Cancer 107(5):765–771. doi:10.1038/bjc.2012.303
Whynes DK, Frew EJ, Manghan CM, Scholefield JH, Hardcastle JD (2003) Colorectal cancer, screening and survival: the influence of socio-economic deprivation. Public Health 117(6):389–395. doi:10.1016/S0033-3506(03)00146-X
Cram P, Fendrick AM, Inadomi J, Cowen ME, Carpenter D, Vijan S (2003) The impact of a celebrity promotional campaign on the use of colon cancer screening: the Katie Couric effect. Arch Intern Med 163(13):1601–1605. doi:10.1001/archinte.163.13.1601
Acknowledgments
Our thanks to all the staff at the St. Mark’s Hospital Bowel Screening Centre for their invaluable help in identifying screened patients, in particular Ms Sarah Marshall (Clinical Programme Manager) and Ms Jennifer Bartley. We would also like to thank the staff at Medical Records & Coding, in particular Mr Stephen Hiles for his help in obtaining the relevant patient data as well Mr Mannish Sankaran for his help in data procurement.
Conflict of interest
The authors have no competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Askari, A., Malietzis, G., Nachiappan, S. et al. Defining characteristics of patients with colorectal cancer requiring emergency surgery. Int J Colorectal Dis 30, 1329–1336 (2015). https://doi.org/10.1007/s00384-015-2313-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2313-8