Abstract
Objective
Ventral rectopexy is a validated treatment for rectal prolapse with a low morbidity rate but a risk of intrarectal mesh migration. The purpose of this study was to report the results of local transanal mesh excision for intrarectal mesh migration after ventral rectopexy.
Methods
Between January 2004 and March 2011, 312 patients underwent laparoscopic ventral rectopexy in two hospitals. Six patients were treated for intrarectal mesh migration.
Results
Delay between ventral rectopexy and the onset of symptoms was 53 months (4–124 months). All patients have symptoms. Imaging revealed a pelvic abscess in two cases. Intrarectal mesh migration was confirmed by anorectoscopy or clinical examination. Five patients were only treated by local transanal partial mesh excision, and one required a colostomy. Morbidity and mortality were zero. The median hospitalization time was 5 days (3–8 days). After a median postoperative follow-up period of 9 months (1–40 months), one recurrence was observed 2 months after surgery.
Conclusion
Local transanal mesh excision for intrarectal mesh migration after laparoscopic ventral rectopexy is a feasible conservative treatment. This simple treatment produced a cure of the pelvic inflammation and closure of the fistula without compromising a more aggressive secondary treatment which was not necessary in our series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Complete rectal prolapse (RP) is the circumferential full-thickness protrusion of the rectal wall through the anal orifice [1]. Ventral rectopexy (VR) improves fecal incontinence, with low recurrence, in patients suffering from these conditions [2]. This procedure involves mobilization of the anterior wall of the rectum and anterior placement of a mesh on the rectum with fixation to the sacrum. The complication rate fluctuates from 1.4 to 47 % in the literature and includes mainly urinary tract infections and port site incisional hernias [2]. After VR, mesh related complications—mesh detachment [3, 4], mesh infection [5], and erosion of the posterior vaginal wall—are rare [6]. In apical vaginal prolapse, mesh erosion is the single most frequent complication in 4.6 to 10.7 % of cases, depending on the different prosthetic materials used [7]. Ouaissi et al. [8] reported good results for mesh ablation, proctectomy with primary colorectal anastomosis, omental patch interposition, and temporary ileostomy in cases of high rectovaginal fistulas after prosthetic material repair for pelvic organ prolapse. When confronted with intravaginal mesh migration after VR without clinical signs for a rectovaginal fistula, treatment by local excision of the mesh has been reported [6], but it is not known whether this conservative approach is effective for intrarectal migration.
The databases of two French surgical centers performing laparoscopic rectal RP surgery were pooled. The purpose was to report the results of local transanal mesh excision for intrarectal mesh migration after laparoscopic VR for RP.
Methods
Between January 2004 and March 2011, 312 patients (273 women, 39 men) with a median age of 60 years (range 18 to 90 years) underwent laparoscopic VR for RP in two surgical centers. The operative technique was standardized in the two centers to the following principles, initially described by D'Hoore and Penninckx [3]: all surgical procedures were performed by surgeons expert in laparoscopy. Four ports were generally used, with a 10 to 12 mmHg pneumoperitoneum. A 0 or 45° laparoscope was used according to the surgeon's preference. Briefly, the dissection was exclusively anterior to the rectum, preserving the lateral ligaments, and dissection was extended to the levator ani muscles. Then a polyester mesh (Parietex, TycoTM) was used for rectal fixation. The mesh was fixed with an endo-stapler (4.0 mm, TycoTM, Norwalk, Connecticut, USA) or suture (Vicryl 3/0, EthiconTM) (204 vs. 108 patients). Patients were commenced on Movicol twice a day from day 1 postoperatively and were weaned of this after discharge over a period of 4–6 weeks. All patients should be reviewed in the outpatient clinic at 1, 3, and 12 months postoperatively and assessed for morbidity.
Management of intrarectal mesh migration
Six (1.9 %) of the female patients with a median age of 67 years (range: 42 to 84 years) had intrarectal mesh migration.
An abdominal CT scan was performed as was gadolinium enhanced magnetic resonance imaging (MRI) of the pelvis using T1- and T2-weighted sequences, plus an anorectoscopy or endorectal ultrasound examination, to evaluate the anal sphincter.
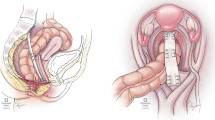
All patients were operated on. Local transanal partial mesh excisions were made in the gynecologic position with a Parks' retractor (Fig. 1) under general anesthesia with an antibiotic cover.
For postoperative follow-up, all patients underwent an initial clinical control at 1 month, then anorectoscopy and an MRI of the pelvis 6 months after local excision.
Results
Patient characteristics, details of surgery, and follow-up are summarized in Table 1. An endo-stapler (n = 2) or suture (n = 4) was used for initial surgical fixation. The median time interval between VR and the onset of symptoms was 53 months (range 4 to 124 months). Three patients complained about anorectal discharge with rectal bleeding or mucus in the stools, one patient had fecal incontinence due to RP recurrence, one patient had sepsis with a rectocutaneous fistula, and one patient just had anal pain. CT scanning and pelvic MRI revealed a pelvic abscess in two cases (Fig. 2). Intrarectal mesh migration was confirmed by anorectoscopy or clinical examination in all cases. All the patients were treated by local transanal partial mesh excision, except for one patient with a rectocutaneous fistula, in whom a colostomy was also performed. The pre- and postoperative course was uneventful in all patients. The median hospitalization time was 5 days (range 3 to 8 days). After a median postoperative follow-up period of 9 months (range 1 to 40 months), only one mesh migration was observed 2 months following the initial partial mesh resection. Local transanal partial mesh excision was performed once again, and the patient is now symptom free with no recurrence of mesh migration. One patient underwent Altemeier's procedure a few months after mesh excision due to recurrence of the RP.
Discussion
Several techniques have been reported in RP surgery including abdominal approaches (pexy, resection, fixation, or combinations thereof) and perineal approaches. The use of prosthetic material has recently become more frequent. VR reduces postoperative constipation and fecal incontinence, with a low rate of recurrence and few complications in patients suffering from RP. Most of the complications after VR are minor [2]. We have reported here a possible severe complication that was treated in six patients by a conservative approach with good results.
With the more frequent use of mesh in pelvic organ prolapse surgery, new complications or adverse effects have been reported. The type of prosthetic material used, the shape of the mesh, and the surgical technique probably has an effect on those possible complications. However, the supremacy of one mesh over another has not been clearly demonstrated in the literature [9, 10]. In our series, the intrarectal mesh migration was always related to the use of a polyetser mesh, secured to the rectal wall using an endo-stapler in two cases and by suturing in four cases.
After pelvic organ prolapse surgery, the incidence of rectovaginal fistula is less than 1 % [11]. Information in the literature concerning intrarectal mesh migration after VR is scarce, and the exact incidence of this complication is unknown. Hernandez et al. [12] reported intraluminal migration of the mesh, which was expulsed via the rectum 2 years after surgery. In our study, migration was found for up to 10 years following the initial surgery. Patients complained of anorectal discharge, fecal incontinence, constipation, pelvic sepsis, or persistent abdominal pain, etc. These symptoms, even several years after surgery, should prompt clinicians to look for intrarectal mesh migration.
Erosion of the posterior vaginal wall has been reported, and in this case, treatment by local excision of the mesh is a possible approach [6]. This conservative treatment has never been described for intrarectal mesh migration, however. In cases of mesh infection after pelvic organ prolapse surgery, ablation of the mesh is classically recommended as a first treatment option, with or without temporary colostomy. If a high rectovaginal fistula occurs, management of the patient can include mesh ablation, proctectomy with primary colorectal anastomosis, omental patch interposition, and temporary ileostomy [8]. The ongoing pelvic inflammatory process and the fistula could be encouraged by the mesh, but in our study, only the intraluminal part of it was excised, the major part of the mesh is still staying in contact with the rectal wall. This led to the complete cure of the pelvic inflammation with a good functional result of the VR.
So far, it is impossible to determine the exact frequency of this complication. We have recognized only the symptomatic patients coming postoperatively. We do not know if some patient can be symptom free with a mesh migration.
In conclusion, local transanal mesh excision for intrarectal mesh migration after laparoscopic VR for RP is a feasible conservative treatment in selected cases. This simple treatment produced a cure of the pelvic inflammation and closure of the fistula without compromising a more aggressive secondary treatment.
Abbreviations
- EUS:
-
Endorectal ultrasound
- MRI:
-
Magnetic resonance imaging
- RP:
-
Rectal prolapse
- VR:
-
Ventral rectopexy
References
Karulf RE, Madoff RD, Goldberg SM (2001) Rectal prolapse. Curr Probl Surg 38:771–832
Samaranayake CB, Luo C, Plank AW et al (2010) Systematic review on ventral rectopexy for rectal prolapse and intussusception. Colorectal Dis 12:504–512
D'Hoore A, Cadoni R, Penninckx F (2004) Long-term outcome of laparoscopic ventral rectopexy for total rectal prolapse. Br J Surg 91:1500–1505
Boons P, Collinson R, Cunningham C, Lindsey I (2010) Laparoscopic ventral rectopexy for external rectal prolapse improves constipation and avoids de novo constipation. Colorectal Dis 12:526–532
Marchal F, Bresler L, Ayav A et al (2005) Long-term results of Delorme's procedure and Orr-Loygue rectopexy to treat complete rectal prolapse. Dis Colon Rectum 48:1785–1790
Portier G, Iovino F, Lazorthes F (2006) Surgery for rectal prolapse: Orr-Loygue ventral rectopexy with limited dissection prevents postoperative-induced constipation without increasing recurrence. Dis Colon Rectum 49:1136–1140
Feiner B, Jelovsek JE, Maher C (2009) Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG 116:15–24
Ouaissi M, Cresti S, Giger U et al (2010) Management of rectovaginal fistulas after prosthetic reinforcement treatment for pelvic organ prolapse. World J Gastroenterol 16:3011–3015
Caliskan C, Denizli A, Makay O et al (2009) Experimental comparison of meshes for rectal prolapse surgery. Eur Surg Res 43:310–314
Jakus SM, Shapiro A, Hall CD (2008) Biologic and synthetic graft use in pelvic surgery: a review. Obstet Gynecol Surv 63:253–266
Dwyer PL, O'Reilly BA (2004) Transvaginal repair of anterior and posterior compartment prolapse with Atrium polypropylene mesh. BJOG 111:831–836
Hernandez P, Targarona EM, Balague C et al (2008) Laparoscopic treatment of rectal prolapse. Cir Esp 84:318–322
Conflicts of interest
None of the authors has any financial or other kind of personal conflicts of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tranchart, H., Valverde, A., Goasguen, N. et al. Conservative treatment of intrarectal mesh migration after ventral laparoscopic rectopexy for rectal prolapse. Int J Colorectal Dis 28, 1563–1566 (2013). https://doi.org/10.1007/s00384-013-1740-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-013-1740-7