Abstract
Background and aims
There is controversy about the effect of the influence of hyperthermia and chemotherapeutic agents on the healing of intestinal anastomosis. The effects of hyperthermic intraperitoneal chemoperfusion (HIPEC) of wound healing after colonic anastomosis were investigated in a rat model.
Materials and methods
Thirty-six Wag/Rija rats were randomized into three groups of 12 animals each: group I: control (only colonic anastomosis was performed) (n = 12); group II: HIPEC (mitomycin C in a concentration of 20 mg/m2 (n = 12) colonic anastomosis was performed before HIPEC; group III: HIPEC (mitomycin C in a concentration of 20 mg/m2 (n = 12) colonic anastomosis was performed after HIPEC. Bursting pressure and bursting sites were recorded 4 and 10 days after intervention. Collagen deposits, inflammation and foreign body reactions were evaluated.
Results
Lower bursting pressure and lost of collagen were found in both HIPEC groups and compared with the control group. There was almost no difference between both HIPEC groups. They were noted overwhelmingly at the anastomosis in the HIPEC group. The degree of collagen accumulation was well-correlated with bursting pressure.
Conclusion
These results have shown that hyperthermic intraperitoneal chemoperfusion (HIPEC) impairs wound healing in colonic anastomosis in rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most wounds, including gastrointestinal anastomosis, follow the same series of events characterized at first by inflammation, then by proliferation of collagen accumulation and reorganization of the scar tissue.
Experimental evidence indicates that wound strength is very low in the first days after colonic anastomotic construction [1, 2].
Anastomotic dehiscence after colorectal surgery is a significant cause of mortality and morbidity [3–5]. The incidence of anastomotic dehiscence in colonic surgery varies greatly, ranging from 0% to 35% [1, 3, 5, 6]. Because anastomotic leakage and dehinscence continue to be an important problem in gastrointestinal tract surgery, a proximal diverting colostomy is advised for patients at risk. It was recognized that cytostatics and/or hyperthermia can inhibit wound healing [6–9].
Several factors were associated with anastomotic leakage such as surgical technique, intestinal integrity, tension across the anastomosis, drugs and patients factors predisposing to poor healing such as concurrent illness. Under optimal conditions, there still remains a risk of dehiscence, which particularly applies to the left colon and rectal anastomosis [10].
Peritoneal seeding from colorectal cancer is relatively resistant to systemic chemotherapy. A treatment strategy for these patients would be hyperthermic intraperitoneal chemoperfusion (HIPEC). This therapeutic design is regarded as one of the best options for the therapy for peritoneal metastasis from gastrointestinal carcinoma. The feasibility of intraperitoneal therapy was demonstrated by several groups, which used this technique in combination with cytoreductive surgery to treat peritoneal carcinomatosis [11–13].
Macroscopic complete resection of PC followed by HIPEC is potentially capable of curing selected patients presenting with disease confined to the peritoneum [14]. The goal of cytoreductive surgery is to achieve a nearly total resection of all tumour tissue. In selected patients, HIPEC may lead to an overall survival in PC [11, 14, 15].
It would be desirable to perform HIPEC synchronously to the resection of the primary tumour. One of the common complication of HIPEC is the anastomotic leak [16, 17].
This study has investigated the effects of hyperthermic intraperitoneal chemoperfusion (HIPEC) on the healing of experimental colon anastomosis.
Materials and methods
Animals
Thirty-six inbred male pathogen-free Wag rats weighing 180 to 220 g obtained from Charles River, Germany were used in this study. The animals were kept separately during the experiment with 12 h of light per day. They were fed a standard laboratory diet and tap water ad libitum. Maintenance and care of all experimental animals were carried out according to the guidelines of the local responsible Animal Protection Commission and carried out in compliance with the national guidelines (National Institute of Health for Use of Laboratory Animals).
Experimental design
The animals were operated by the same investigator. The animals were anesthetized with isoflurane (Baxter, Unterschleißheim, Germany) in a mixture of oxygen and nitrous oxide. Under semi-sterile conditions, the abdomen was opened by median laparotomy of approximately 6 cm.
Thereafter, the animals were randomized into three different operative groups of 12 animals each. Every group were subdivided into two subgroups:
Group I: control (abdomen was open for 30 min).
Group II: HIPEC with mitomycin C (MMC) 20 mg/m2, anastomosis was performed before HIPEC.
Group III: HIPEC with mitomycin C (MMC) 20 mg/m2, anastomosis was performed after HIPEC.
All treatments were performed by the same investigator (J.P.) who has a high experience in these settings.
A 1 cm control colon segment was resected 3 cm proximal to the peritoneal reflection and the colonic continuity was restored by constructing an end to end anastomosis by using eight single layer inverting inter-ruptured sutures (Ethicon 7/0; Ethicon, Norderstedt, Germany).
Perfusion model
The perfusion model was performed as described previously [18]. The equipment consisted of a miniature heat exchanger and a roller pump. The HIPEC system is a closed circuit allowing perfusate circulation with a variable dynamic flow of 10–15 ml/min. The warmed perfusate (500 ml saline) was driven by a roller pump with two synchronously running pump heads on a single axis for the inflow and the outflow lines (Masterflex®). An inflow catheter was inserted into the upper abdomen between the hepatic and diaphragmatic surface and an outflow catheter was placed within the pouch of Douglas.
The intraperitoneal temperature was maintained between 40.5°C and 41°C. Baseline temperature was recorded for 5 min before treatment. For temperature measurement during perfusion, a nickel–chrome–nickel thermocouple of 0.6 mm in diameter (Standard Integrated Thermocouple Thermocoax, Phillips, Hamburg, Germany) was placed near the anastomosis. Perfusion was performed over 90 min (like the clinical situation) from the point when the perfusion fluid reached the required temperature. Then, in groups II and III MMC was added to the system in a drug dose of 20 mg/m2. The body surface of the animals was calculated with the Dubois formula [19] \({\left( {A{\left( {m^{2} } \right)} = m^{{0.425}}_{{\text{k}}} \times 1^{{0.725}}_{{\text{K}}} \times 0.007184;\,m^{2} = body\,surface;\,m_{{\text{k}}} = body\,length;\,1_{{\text{K}}} = body\,weight} \right)}.\) MMC was added in three divided doses with a 30 min interval to the perfusate. The first dose contained 50% and the following administrations contained 25% of the total dose.
After perfusion, the perfusate was aspirated and the abdomen was closed into two layers running 3-0 silk suture. No perioperative antibiotics were applied.
Evaluation
The animals were kept under standard conditions and were killed by an overdose of anesthetic and cervical dislocation 4 or 10 days after treatment.
The animals were autopsied and the abdomen was explored for signs of inflammation. The abdomen and anastomosis were evaluated for abscess and adhesion formation.
The following grading system was used for adhesion assessment:
The mean of the specimens were calculated.
Abscess formation was scaled as present or absent. The colonic anastomosis was removed and was evaluated qualitatively and quantitatively. The intestinal segment with the anastomosis (margins of 2 cm on each side) with the sutures left in place was attached to an infusion pump filled with saline.
Wound strength and microscopic analysis
One end of the colon segment was cannulated with a pressure recorder. Then a cannula was inserted into the intestinal lumen of the other end. The cannula was connected with an infusion pump. The intra-colonic pressure was raised with an infusion rate of 49.9 ml/h and recorded. The bursting pressure recorded immediately before the sudden loss of pressure and the localisation of the rupture—anastomosis or colonic wall—were noted. This procedure was described previously [20].
Thereafter, the anastomotic segment was cleaned from adhering tissue and a 10 mm sample containing the complete suture line in the middle was opened at the mesenteric side and fixed in 4% formaldehyde. These specimens were dehydrated and embedded in paraffin. From each specimen, paraffin sections of 4 μm in thickness were stained with hematoxilin–eosin (H & E) and with elastica van Gieson (EvG) to identify collagen fibers. Sections were analysed semi-quantitatively by two independent observers by using a binocular light microscope.
Anastomosis were graded histologically in a blind fashion using the following morphologic criteria reported by Salm et al. [21]: Edema, fibrin and collagen were subjectively rated on a scale of 0–3 according to an increasing amount. Granulocytes, lymphocytes, histiocytes, plasma cells, giant cells and fibroblasts were scored from 0 to 3 on the basis of the cell number per square unit.
Statistical analysis
Data were analysed using the SPSS/PC+ statistical software. The mean scores and the standard error of mean were calculated. The significance of the differences was assessed by the Kruskal–Wallis test. Differences were considered significant at a calculated p value of less than 0.05.
Results
One animal in group II died of sepsis after 6 days.
Intra-abdominal complications were more common in groups II and III than in the control group. Peri-anastomotic adhesions were subjectively more common in HIPEC groups than in group I. There were four animals in group II and five animal in group III with abscesses. All animals with intestinal obstruction (group I: n = 0; group II: n = 2; group III: n = 2) also presented with adhesions.
The clinical outcome of all groups are showed in Table 1.
Anastomotic strength
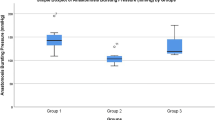
Individual measurements of bursting pressure are depicted in Figs. 1 and 2 . Bursting occurred at the anastomosis in four of six animals in group I and in all animals in group II and III 4 days after intervention. After 10 days, the bursting sites were observed on the anastomotic line in one of six animals in group I and in three of six and four of six animals in groups II and III, respectively.
Anastomotic strength post-operatively. The median are given for bursting pressure. (Group I: control without treatment; group II: anastomosis was performed before HIPEC; group III: anastomosis was performed before HIPEC) (§: group III vs group I, p = 0.028; *: group II vs group I, p = 0.03; $: group II and group III vs group I, p = 0.24; Kruskal–Wallis)
In all groups, the bursting strength increased between days 4 and 10 after the intervention. The average bursting pressure in groups II and III (HIPEC) was significantly reduced vs the control group I, 4 and 10 days after the operation. The bursting pressure in group I was found as 202 ± 16 and 356 ± 24 mmHg, 4 and 10 days after intervention. Bursting pressure was significantly reduced to 74 ± 24 and 98 ± 18 mmHg after 4 days in groups II and III, respectively. Bursting pressure was also significantly reduced to 243 ± 121 and 278 ± 29 mmHg 10 days post-operatively in groups II and III, respectively.
In addition, the bursting site was more often within the suture line in the treatment groups than in the control group. The anastomosis ruptured all outside the anastomotic area 10 days postoperatively in group I indicating that anastomotic healing had progressed beyond the values of normal bowel wall resistance.
No significant differences in breaking strength were observed between both HIPEC groups after 4 or 10 days (groups II and III) (p < 0.05).
Histologic studies
Inflammatory reaction in all groups was seen but more in groups II and III than in group I 4 days after intervention.
Restoration of mucosal integrity seemed better without treatment (control group). Staining of collagen fibers with van Gieson presented more collagen density after 10 days. Collagen density in group I was low 4 days post-interventionally but in the H & E staining, the granulation tissue was well and the anastomosis was closed.
The colonic anastomosis healed worse when treatment with HIPEC was administered and apart from more inflammatory tissue, a low number of vessels in the granulation tissue were discerned at histology. A comparison of wound histology after 4 and 10 days did not indicate essential differences between the two HIPEC groups. Semi-quantitative analysis of the number of granulocytes, fibroblasts, lymphocytes and macrophages and degree of necrosis, wound area surface and sub-mucosa bridging showed a similarity between groups II and III. Anastomosis was irregular and in most cases not closed (Fig. 3a). Van Gieson staining showed comparable collagen deposition in both HIPEC groups as a reason for the mechanical instability of the wound tissue (Fig. 3b).
Comparison of granulation tissue in colonic wound healing in HIPEC treated rats 10 days after intervention. H & E staining demonstrates the abundance of macrophages and granulocytes in the granulation tissue, more prominent in the both HIPEC groups. Incomplete epithelialization and a huge ulcer in the mucosa
Semi-quantitative results of the histology are shown in Table 2.
Discussion
Hyperthermic intraperitoneal chemoperfusion (HIPEC) is a new development in the treatment of peritoneal metastasis originating from gastrointestinal tumours. Clinical studies conducted by several groups clearly showed prolonged survival times compared to patients treated by a conventional therapy [22–24].
In many cases, HIPEC is performed in the same session as the resection of the primary tumour. In these cases, the colorectal cancer is resected first, followed by surgical cytoreduction and heated chemoperfusion. Even though patients have promising longer survival times after HIPEC, this procedure does suffer from higher morbidity and mortality [25]. The mortality figure rises up to 20% particularly in patients older than 70 years [25].
Surgical complications, in some cases with very notable rates, after HIPEC were reported in many literature sources. The most common complication related to surgery was anastomosis leakage. Reported rates of anastomosis leakage vary between 8% and 20% depending on the site of anastomosis, size of resection and individual risks after HIPEC [25, 26]. High risk anastomosis such as anterior resection of the rectum appears to be particularly endangered. As reported by Averbach et al., the incidence of anastomosis leakage after double-stapled low colorectal resection without additional therapy was 6% compared to 20% after heated peritoneal chemotherapy [27].
Some authors have described the influence of hyperthermia and/or cytostatic treatment on the healing of gastrointestinal anastomoses [8, 9, 21, 28, 29]. This commonly promotes anastomosis leakage, which may lead to severe clinical complications. As HIPEC therapy includes both hyperthermia and cytostatics and is administered at the time of performing an anastomosis, this raises the question whether HIPEC has a detrimental effect on the healing of the anastomosis. Another controversial issue is whether the anastomosis is to be performed before or after HIPEC. These experiments were designed to demonstrate the possible differences in healing regarding the times of anastomosis.
The natural course of anastomotic healing is characterized by a slow increase in bursting strength during the first 4 post-operative days and a rise thereafter. So, we chose the time points of evaluation after 4 and 10 days.
In the clinical settings, HIPEC is performed for 90 min from most authors [22–24] and they use MMC in a concentration of 20–35 mg/m2. So, we took these settings in our experiments.
Our own investigations showed a significant decrease in bursting pressure in both HIPEC groups. Two cases of anastomosis leakage with serious complications such as faecal peritonitis were demonstrated. The clinical picture was confirmed histologically. After 4 days, healing of the anastomosis in groups II and III was severely delayed and after 10 days, no definite connective tissue linking at the site of the anastomosis was histologically visible. On the other hand, the control group showed regular anastomosis healing after 4 and 10 days, respectively.
No difference could be found between the two HIPEC groups. Neither the number of clinical complications nor the bursting pressures showed significant differences. Histological examination after 4 and 10 days was virtually identical in groups II and III with both H & E and EvG staining. Therefore, it is not important whether HIPEC is performed before or after performing the anastomosis.
Instances of delayed healing of animal intestinal anastomosis after cytostatic therapy were reported [7, 29]. As with our own studies, these also showed a decrease in collagen formation. In studies where alternative cytostatics such as 5-flurouracil were used, considerably higher leakage rates and anastomosis complications were also observed [9, 21, 29]. Wound healing is distinctly more compromised than after hyperthermic treatment [8]. Individually, neither form of treatment appears to have grave effects on anastomosis healing [6]. Since the effects of hyperthermia and MMC as monotherapy in animal experiments have already been comprehensively described, the study design deliberately omitted these two groups.
In contrast to the control group, neither of the HIPEC groups in our own studies showed the normal formation of collagen or connective tissue, which points to HIPEC as the likely cause of decrease in synthesis nor was any adequate collagen synthesis apparent after 4 days in the control group. This is explained by the observation of Brasken, i.e. that the highest expression of collagen-associated genes is first noted after a week [28]. However, normal wound healing with connective tissue bridge formation was observed, which was not apparent in groups II and III.
Another point of interest is the possibility of local recurrence in tumour growth in the anastomotic area. From a theoretical point of view, it could be that the sequence HIPEC and then performing anastomosis may prevent the growth from residual tumour cells. To answer these questions further experimental settings must follow.
Conclusion
Overall, the animal model described here clearly showed delayed healing of the colon anastomosis after HIPEC with a subsequent significant increase in complications compared to the control group.
As these clinical data also show an increase of complications post HIPEC, protective measures should be taken when high risk anastomosis, for instance anterior resection of the colon or performing of three anastomosis or more, which are performed together with HIPEC.
References
Hendriks T, Mastboom WJ (1990) Healing of experimental intestinal anastomoses. Parameters for repair. Dis Colon Rectum 33:891–901
Simeon A, Monier F, Emonard H, Gillery P, Birembaut P, Hornebeck W et al (1999) Expression and activation of matrix metalloproteinase in wounds: modulation by the tripeptide-copper complex glycyl-l-histidyl-l-lysin-Cu2+. J Invest Dermatol 112:957–964
Nesbakken A, Nygaard K, Lunde OC, Blucher J, Gjertsen O, Dullerud R (2005) Anastomotic leak following mesorectal excision for rectal cancer: true incidence and diagnostic challenges. Colorectal Dis 7(6):576–581
Mann B, Kleinschmidt S, Stremmel W (1996) Prospective study of hand-sutured anastomosis after colorectal resection. Br J Surg 83:29–31
Pakkastie TE, Luukkonen PE, Jarvinen HJ (1994) Anastomotic leakage after anterior resection of the rectum. Eur J Surg 160:293–297
Biert J, Seifert W, de Man B, Wobbes T, Hoogenhout J, Hendriks T (1996) Combined preoperative irradiation and local hyperthermia delays early healing of experimental colonic anastomoses. Arch Surg 131(10):1037–1042
Uzunkoy A, Bolukbas C, Horoz M, Bolukbas FF, Kocyigit A (2005) The optimal starting time of postoperative intraperitoneal mitomycin-C therapy with preserved intestinal wound healing. BMC Cancer 5:31
Mansson P, Zhang XW, Jeppsson B, Thorlacius H (2002) Anastomotic healing in the rat colon: comparison between a radiological method, breaking strength and bursting pressure. Int J Colorectal Dis 17(6):420–425
Kanellos I, Mantzoros I, Demetriades H, Kalfadis S, Kelpis T, Sakkas L, Betsis D (2004) Healing of colon anastomoses covered with fibrin glue after immediate postoperative intraperitoneal administration of 5-fluorouracil. Dis Colon Rectum 47(4):510–515
Khoury GA, Waxman BP (1983) Large bowel anastomosis. I. The healing process and sutured anastomosis. A review. Br J Surg 70:61–63
Moran BJ, Meade B, Murphy E (2006) Hyperthermic intraperitoneal chemotherapy and cytoreductive surgery for peritoneal carcinomatosis of colorectal origin: a novel treatment strategy with promising results in selected patients. Colorectal Dis 8(7):544–550
Liberale G, Pocard M, Manganas D, Ducreux M, Lasser P, Elias D (2006) Hyperthermic intraperitoneal chemotherapy in the treatment of peritoneal carcinomatosis of digestive and peritoneal origin: rationale. Acta Chir Belg 106(3):291–296
Sugarbaker PH (2006) New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome? Lancet Oncol 7(1):69–76
Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H, Zoetmulder FA (2003) Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 21(20):3737–3743
Glehen O, Kwiatkowski F, Sugarbaker PH, Elias D, Levine EA, De Simone M, Barone R, Yonemura Y, Cavaliere F, Quenet F, Gutman M, Tentes AA, Lorimier G, Bernard JL, Bereder JM, Porcheron J, Gomez-Portilla A, Shen P, Deraco M, Rat P (2004) Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol 22(16):3284–3292
Esquivel J, Vidal-Jove J, Steves MA, Sugarbaker PH (1993) Morbidity and mortality of cytoreductive surgery and intraperitoneal chemotherapy. Surgery 113(6):631–636
Jacquet P, Stephens AD, Averbach AM, Chang D, Ettinghausen SE, Dalton RR, Steves MA, Sugarbaker PH (1996) Analysis of morbidity and mortality in 60 patients with peritoneal carcinomatosis treated by cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy. Cancer 77(12):2622–2629
Pelz JO, Doerfer J, Hohenberger W, Meyer T (2005) A new survival model for hyperthermic intraperitoneal chemotherapy (HIPEC) in tumor-bearing rats in the treatment of peritoneal carcinomatosis. BMC Cancer 5(1):56
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition (5):303–311
Fumagalli U, Trabucchi E, Soligo M, Rosati R, Rebuffat C, Tonelli C, Montorsi M (1991) Effects of intraperitoneal chemotherapy on anastomotic healing in the rat. J Surg Res 50(1):82–87
Salm R, Wullich B, Kiefer G, Fiebig HH, Farthmann EH (1991) Effects of a three-drug antineoplastic protocol of wound healing in rats: a biomechanical and histologic study on gastrointestinal anastomoses and laparotomy wounds. J Surg Oncol 47(1):5–11
Shen P, Levine EA, Hall J, Case D, Russell G, Fleming R, McQuellon R, Geisinger KR, Loggie BW (2003) Factors predicting survival after intraperitoneal hyperthermic chemotherapy with mitomycin C after cytoreductive surgery for patients with peritoneal carcinomatosis. Arch Surg 138(1):26–33
Sugarbaker PH, Stuart OA, Yoo D (2005) Strategies for management of the peritoneal surface component of cancer: cytoreductive surgery plus perioperative intraperitoneal chemotherapy. J Oncol Pharm Pract 11(3):111–119
Verwaal VJ, van Ruth S, Witkamp A, Boot H, van Slooten G, Zoetmulder FA (2005) Long-term survival of peritoneal carcinomatosis of colorectal origin. Ann Surg Oncol 12(1):65–71
Smeenk RM, Verwaal VJ, Zoetmulder FA (2005) Toxicity and mortality of cytoreduction and intraoperative hyperthermic intraperitoneal chemotherapy in pseudomyxoma peritonei—a report of 103 procedures. Eur J Surg Oncol 32(2):186–90
Piso P, Dahlke MH, Loss M, Schlitt HJ (2004) Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in peritoneal carcinomatosis from ovarian cancer. World J Surg Oncol 2(1):21
Averbach AM, Chang D, Koslowe P, Sugarbaker PH (1996) Anastomotic leak after double-stapled low colorectal resection. Dis Colon Rectum 39(7):780–787
Brasken P (1991) Healing of experimental colon anastomosis. Eur J Surg Suppl (566):1–51
el-Malt M, Ceelen W, Van den Broecke C, Cuvelier C, Van Belle S, de Hemptinne B, Pattyn P (2003) Influence of neo-adjuvant chemotherapy with 5-fluorouracil on colonic anastomotic healing: experimental study in rats. Acta Chir Belg 103(3):309–314
Acknowledgements
This study was supported by grants from the ELAN (Erlanger Leistungsbezogene Anschubfinanzierung und Leistungsförderung).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pelz, J.O.W., Doerfer, J., Decker, M. et al. Hyperthermic intraperitoneal chemoperfusion (HIPEC) decrease wound strength of colonic anastomosis in a rat model. Int J Colorectal Dis 22, 941–947 (2007). https://doi.org/10.1007/s00384-006-0246-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-006-0246-y