Abstract
Background and aims
The value of surgery for patients with incurable colorectal cancer is controversial. This study evaluated outcomes in patients undergoing non-curative surgery for colorectal cancer and aimed to identify patients who would benefit from palliative surgery.
Patients and methods
Demographics, tumour characteristics, operating details and outcomes were reviewed for 180 patients undergoing surgery for incurable colorectal cancer; palliative resection was performed in 150 cases. Seventeen patients died in the postoperative period. Risk factors for postoperative mortality and poor survival were analysed with univariate and multivariate analysis.
Results
Multivariate analysis showed that operative mortality was significantly higher in patients with non-resection surgery and in those with ascites. Median survival of patients with resection was significantly longer than in those without resection (30 vs. 17 weeks). Other independent factors that were significantly associated poor survival were the presence of ascites, presence of bilobar liver metastasis and absence of chemotherapy and/or radiation therapy.
Conclusion
Non-curative surgery is associated with high mortality in patients without resection and in the presence of ascites. These two factors, together with the presence of bilobar liver metastasis and the absence of chemotherapy and/or radiation therapy, are associated with poor survival. In the presence of these factors the balance between the benefit and risk of surgery should be carefully considered before decision for operative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is one of the most common malignancies in developed countries. Despite the increased public awareness of the disease and the endeavors of screening programs to detect early colorectal cancer, about 30% of patients present with incurable disease [1]. Inability to cure may be due to locally advanced tumours or the presence of unresectable distant metastases. The primary cancer can lead to chronic symptoms such as anaemia and to acute complications such as bowel obstruction and perforation. Whether surgical palliation, which can be achieved by resection, bypass or proximal diversion, is indicated in these patients is controversial. Most of these patients have been debilitated by the advanced malignancy, and many are also elderly patients with concomitant medical diseases. Thus they are poor risk candidates for surgery. The survival of these patients, on the other hand, is seldom improved by surgical treatment. The identification of factors that predict the outcomes of surgery would help to select patients who would benefit from palliative surgery. This study reviewed the results of non-curative surgery for patients with primary colorectal cancer and analysed factors that might influence the operative mortality, postoperative morbidity and the survival of these patients.
Patients and methods
Data from 180 patients (99 men, 81 women; median age 70 years, range 30–91) undergoing non-curative surgery for primary colorectal cancers were entered prospectively into a database of colorectal malignancy in the Department of Surgery, Queen Mary Hospital, University of Hong Kong Medical Centre between January 1996 and December 1999. Patients’ main presenting symptoms are listed in Table 1; rectal bleeding was the main symptom in 24% of patients. Urgent presentation with intestinal obstruction or perforation occurred in 28%. Concomitant medical diseases were present in 86%, particularly in elderly patients. Six patients had synchronous tumours. Table 2 presents the sites of the primary index cancer. Tumours distal to the splenic flexure were found in 60%. The type of surgery is shown in Table 3. Resection of the cancer was performed in 150 of the 180 patients. Surgery was elective in 130 patients, and the remaining 50 were operated on as urgent surgery. Median hospital stay was 9 days (range 4–52).
Patients’ demographics, their presentations, the locations of primary cancers and metastases, operative details, postoperative outcomes, and survival data were reviewed. Non-curative surgery was defined as the presence of residual local disease in the operative field and/or the presence of unresectable distant metastases. Patients with synchronous metastases which could be completely resected at the same setting or in subsequent operations were not classified as non-curative surgery, and they were excluded in this study. Operative mortality was defined as death that occurred within 30 days from the surgery. Morbidity was defined as any postoperative complication that led to the increased hospital stay, additional procedures or postoperative mortality.
Categorical variables were analysed by the χ2 test or Fisher’s exact test when appropriate. Continuous variables were presented in median values and range; they were analysed by the Mann-Whitney U test. Survival was calculated from the time of surgery. Analysis of survival excluded patients who died during the postoperative period. Survival data were analysed by the Kaplan-Meier method. Factors were compared by log-rank test. Multivariate analysis used the Cox proportional hazard model, and factors with P values less than 0.05 in univariate analysis were included in the multivariate analysis. Presentation of results includes hazard ratio (HR) and 95% confidence interval (CI). P values less than 0.05 were considered statistically significant.
Results
The characteristics of patients with resection and non-resection are shown in Table 4. Elderly patients (aged over 75 years) were more likely to have non-resection, and patients had rectal cancer also tended to have non-resection although this did not reach statistical significance (P=0.076, Fisher’s exact test). In 109 patients there were unresectable distant metastases and in 61 residual locoregional disease without distant spread.
Seventeen patients died in the postoperative period and the causes of death are shown in Table 5. The median age of these patients was 78 years (range 41–85). Eleven had undergone elective surgery while six had emergency operations. The operative mortality rates of patients with resection and non-resection were 6.7% and 21%, respectively (P=0.01, Fisher’s exact test). Other significant factors that affected the postoperative mortality were old age (>75 years) and the presence of ascites. The only independent factors associated with significant operative mortality in multivariate analysis were performance of non-resection surgery (P=0.03, HR 4.6, 95% CI 0.09–0.90) and the presence of ascites (P=0.02, HR 5.1, 95% CI 0.10–0.85). Postoperative morbidity occurred in 33 patients (Table 6). Postoperative therapy (19 chemotherapy, 6 radiation therapy, 7 combined chemoradiation) was given to 31 paitents, particularly to those who were younger in age or had a lower incidence of comorbid medical diseases (Table 7).
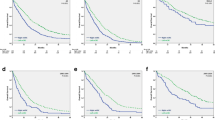
Five patients left Hong Kong shortly after the surgery. Their follow-up data were incomplete, and they were excluded from the survival analysis. The median survival of patients with resection and without resection was 30.3 and 17.1 weeks, respectively (P<0.001;(Fig. 1). The analysis of risk factors that might affect the survival is shown in Table 8. Multivariate analysis showed poor survival to be associated with non-resection surgery (P<0.001, HR 2.39, 95% CI 1.52–3.73), the presence of ascites (P=0.018, HR 1.6, 95% CI 1.08–2.35), presence of bilobar liver metastases (P=0.022, HR 1.47, 95% CI 1.06–2.04) and absence of other therapies (P=0.016, HR 1.68, 95% CI 1.14–2.54).
Discussion
Surgical treatment for patients with incurable colorectal cancer is controversial. Improvement in survival is usually not possible in the majority of these patients except in those presenting with life-threatening emergencies. Palliation of symptoms and avoiding complications such as obstruction, perforation and profuse bleeding are the main objectives of the operative treatment. However, these patients are usually compromised by the presence of advanced malignancies, and many of them also suffer from concomitant medical diseases, rendering surgical treatment an option with high risk. Surgery is worthwhile only if a reasonable length of survival can be achieved, and the operative risk is acceptable. There have been only a few studies with detailed analysis of the results of palliative surgery for primary colorectal cancer [2, 3, 4]. The present study included a sizable number of patients within a short period. Thus major differences in the surgical decision and surgical techniques as well as postoperative care in the study period are not significant.
The most common main presentation of patients was bleeding. Overt bleeding or anaemia accounted for 36% of main symptoms. Urgent presentation of obstruction or perforation occurred in for 27.8% of the patients. Liu et al. [2] and Joffe and Gordon [5] have also reported that bleeding and obstruction to be the main presenting symptoms in patients with palliative surgery. Patients presenting with obstruction or perforation usually require urgent decision for surgery. Until recently surgery remained the only means to relieve obstruction, and creation of a stoma is usually inevitable. In recent years self-expanding metallic stents have proven an effective non-operative means to relieve acute colonic obstruction, and urgent surgery with can be avoided [6, 7]. On the other hand, bleeding from the tumour is rarely severe. There is usually no urgency to palliate the symptom, and the benefit of operative treatment should be weighed against the risk of surgery and the likelihood of a reasonable duration of survival.
We adopt an aggressive approach in non-curative surgery, aiming at resection of the primary tumour except in situations when resection is hazardous or when the patient is in very poor condition. An aggressive approach is also advocated by other authors [3, 8] as it was regarded a better palliation. Resection was achieved in 83.3% of patients in our series. Other series report resection rates ranging from 69% [4] to 90% [2]. We found that resection was less likely to be performed in elderly patients. There is tendency to perform non-resection in patients with rectum or rectosigmoid cancer as surgery in the pelvis is likely to carry high morbidities.
The operative mortality of all the patients was 9.4%. This is comparable to data from other series reporting non-curative surgery [2, 4]. Most of the patients died of pulmonary causes or advanced malignancy. Three patients died of intra-abdominal sepsis; two had perforated tumours with faecal peritonitis, and the other one had a subhepatic collection not due to anastomotic leakage. Non-resection surgery, old age and presence of ascites were identified as risk factors associated with a high mortality rate. In the multivariate analysis only non-resection and the presence of ascites were independent factors for high postoperative mortality. Although no radical procedures were performed in patients with non-resection surgery, high mortality is usually reported in non-resection surgery. Both Liu et al. [2] and Makela et al. [4] reported operative mortality of 17% in patients without resection, while rates in those with resection were 9% and 5%, respectively. However, it should be emphasized that in most series the patients who did not receive resection were those with advanced diseases, severe comorbidities or unstable haemodynamic status during surgery. Surgical resection, which involved longer operating time and more blood loss, were considered more hazardous.
The morbidity rate was 18.3%, which is comparable to others’ reports [2, 8]. Although Joffe and Gordon [5] reported a morbidity rate of 50%, the majority of complications were wound infections. The relative uncommon occurrence of major surgical complications reflects the philosophy in palliative surgery. With the objective for palliative treatment, oncological resection is usually not performed and radical multi-organ resection such as exenteration is usually avoided. Moreover, approach to dangerous areas such as the root of the mesentery is usually not attempted. This is true particularly in urgent surgery. In our series anastomotic leakage occurred only in one patient. Moran et al. [8] also advocated anastomosis in palliative surgery for rectal cancer, and they reported one case of anastomotic leakage in 60 patients with palliative anterior resection. Thus restoring the bowel continuity is not a hazardous procedure and can improve quality of life. Four patients had intra-abdominal sepsis in our series. All except one presented with a perforated cancer.
Palliative resection is therefore a safe procedure with acceptable mortality and morbidity. However, in situation when resection is deemed impossible, or when there is ascites, operative mortality is high. In the presence of these factors surgery should be carefully considered and should be performed only in those who can benefit from surgical palliation. Having said this, non-resection surgery, which is associated with similar morbidity and hospital stay as resection surgery, may be the only option to palliate complications such as obstruction or perforation so that the patient can be discharged to enjoy a mediocre quality of life in the remaining days. This option, however, should be considered in individual patient, and good clinical judgment to balance the benefit and risk of surgery is definitely important.
Other authors have identified the factors associated with poor survival in surgery for incurable colorectal cancer [2, 3]. Liu and colleagues [2] found that extensive liver involvement and poorly differentiated tumours were associated with poor survival. Joffe and Gordon [5] reported poor risk factors to be age over 75 years, the presence of extensive liver metastases and cardiovascular disease. In the study of stage IV disease Rosen et al. [3] found that carcinomatosis and bilobar liver involvement were associated with poor survival. In our study non-resection surgery, bilobar liver metastasis, the presence of ascites, and the absence of other therapies were independent significant factors for poor survival in the multivariate analysis. These three factors, which are quite similar to those in others’ reports, indicate the advanced stage of the disease. The poor survival associated with these factors does not make surgical treatment worthwhile if the patients do not have severe symptoms. In the case of life threatening complications such as obstruction, however, it is usually a dilemma to decide the mode of management. Surgery may be the only effective option to palliate the symptoms and to provide a mediocre quality of life of the patients in the short remaining life. Obviously the decision may need individual consideration, and the potential benefit and risk should be balanced carefully. The possible of other means of palliation such as insertion of stents should also be considered.
We also found that the use of therapeutic chemotherapy and/or radiation therapy was associated with better survival. Admittedly this was a selected group with better general condition, and they can tolerate the potential side effects of chemotherapy or radiation therapy. The response rate of traditional 5-fluorouracil based chemotherapy for metastatic colorectal cancer is about 30% [9, 10]. Improved survival and better quality of life have been demonstrated in patients with chemotherapy than in those with the best supportive treatment [11]. The newer chemotherapeutic agents such as irinotecan and oxaliplatin have been shown to produce survival benefit and to improve quality of life in patients not responding to 5-fluorouracil based chemotherapy [12]. Improved survival is likely to be achieved in current chemotherapeutic regimens. However, there is no consensus on whether it is necessary to resect the primary cancer before the initiation of chemotherapy. Surgery, with its potential complications, may in fact delay the treatment. Further study, preferably by randomized trials, of this aspect is required to better define the role of palliative resection.
In conclusion, non-curative surgery for colorectal cancer is associated with high mortality, especially in patients without resection and in the presence of ascites. In addition to these two factors, the presence of bilobar liver metastasis and the absence of chemotherapy and/or radiation are also associated with poor survival. In the presence of these poor risk factors, good clinical judgment and careful balance between the risk and benefit are necessary before embarking on surgical palliation.
References
Devesa JM, Morales V, Enriquez JM, Nuno J, Camunas J, Hemandez MJ et al (1988) Colorectal cancer. The bases for a comprehensive follow-up. Dis Colon Rectum 31:636–652
Liu SK, Church JM, Lavery 1C, Fazio VW (1997) Operation in patients with incurable colon cancer—is it worthwhile? Dis Colon Rectum 40:11–14
Rosen SA, Buell JF, Yoshida A, Kazsuba S, Hurst R, Michelassi F et al (2000) Initial presentation with stage IV colorectal cancer: how aggressive should we be? Arch Surg 135:530–534
Makela J, Haukipuro K, Laitinen S, Kairaluoma MI (1990) Palliative operations for colorectal cancer. Dis Colon Rectum 33:846–850
Joffe J, Gordon PH (1981) Palliative resection for colorectal carcinoma. Dis Colon Rectum 24:355–360
Law WL, Chu KW, Ho JW, Tung HM, Law SY, Chu KM (2000) Self-expanding metallic stent in the treatment of colonic obstruction caused by advanced malignancies. Dis Colon Rectum 43:1522–1527
Tejero E, Femandez-Lobato R, Mainar A, Montes C, Pinto I, Femandez L et al (1997) Initial results of a new procedure for treatment of malignant obstruction of the left colon. Dis Colon Rectum 40:432–436
Moran MR, Rothenberger DA, Lahr CJ, Buls JG, Goldberg SM (1987) Palliation for rectal cancer. Resection? Anastomosis? Arch Surg 122:640–643
Petrelli N, Herrera L, Rustum Y, Burke P, Creaven P, Stulc J et al (1987) A prospective randomized trial of 5-fluorouracil versus 5-fluorouracil and high-dose leucovorin versus 5-fluorouracil and methotrexate in previously untreated patients with advanced colorectal carcinoma. J Clin Oncol 5:1559–1565
Doroshow JH, MulthaufP, Leong L, Margolin K, Litchfield T, Akman S et al (1990) Prospective randomized comparison of fluorouracil versus fluorouracil and high-dose continuous infusion leucovorin calcium for the treatment of advanced measurable colorectal cancer in patients previously unexposed to chemotherapy. J Clin Oncol 8:491–501
Scheithauer W, Rosen H, Komek GV, Sebesta C, Depisch D (1993) Randomised comparison of combination chemotherapy plus supportive care with supportive care alone in patients with metastatic colorectal cancer. BMJ 306:752–755
Cunningham D, Pyrhonen S, James RD, Punt CJ, Hickish TF, Heikkila R et al (1998) Randomised trial of irinotecan plus supportive care versus supportive care alone after fluorouracil failure for patients with metastatic colorectal cancer. Lancet 352:1413–1418
Acknowledgements
These findings were presented at the 18th World Congress of the International Society of Digestive Surgery held in Hong Kong in December 2002.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Law, W.L., Chan, W.F., Lee, Y.M. et al. Non-curative surgery for colorectal cancer: critical appraisal of outcomes. Int J Colorectal Dis 19, 197–202 (2004). https://doi.org/10.1007/s00384-003-0551-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-003-0551-7