Abstract
Purpose
Frequent post-operative cholangitis in biliary atresia (BA) affects the long-term native liver survival. This study assessed the characteristics of early cholangitis and their influence on the prognosis.
Methods
Forty-three patients with BA who underwent surgery between 2000 and 2020 were analyzed for routine inflammatory markers. Early cholangitis characteristics were compared between native liver survivor (NLS) and living donor liver transplant (LDLT) patients.
Results
Among the 43 patients, 30 (69.8%) experienced 130 episodes of cholangitis. In the area under the receiver operating characteristics curve (AUROC) analysis, the cutoff value of the total cholangitis episodes was 3, with an area under the AUROC curve of 0.695 (95% confidence interval 0.522–0.868). Before 3 years old, 113 episodes (86.9%) of cholangitis were observed. The white blood cell, C-reactive protein, and alanine aminotransferase values at cholangitis onset did not markedly differ between the LDLT and NLS groups. Conversely, the neutrophil-to-lymphocyte ratio in the NLS group was significantly lower than in the LDLT group (0.85 vs. 1.63, p < 0.001).
Conclusions
Cholangitis in the NLS group was lymphocyte-dominant and atypical in its pathogenesis. Lymphocyte-dominant cholangitis is non-suppurative, and future research should clarify its pathogenesis to improve the treatment and prognosis of BA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Repeated episodes of cholangitis after Kasai portoenterostomy (KPE) adversely affect the outcome of patients with biliary atresia (BA) [1]. Possible predisposing factors for cholangitis include an insufficient volume of bile flow due to inherent hepato-cholangiopathy of the BA liver, temporary dehydration with reduced bile flow, and infection of the intrahepatic bile ducts due to bacteria ascending via the bilioenteric conduit with or without its obstruction [2].
Postoperative prophylactic intravenous antibiotic therapy did not decrease the incidence of cholangitis, even when administered for relatively long periods [3]. Previously adopted cholangitis-preventing surgical procedures, such as exteriorization of the Roux-en-Y limb or anti-reflux valve placement in the limb, have failed to decrease the number of cholangitis episodes [4]. Thus, the pathogenetic mechanism underlying post-operative cholangitis in BA may not be simple suppurative cholangitis due to ascending bacteria; rather, it may involve a more complex cholangiopathy.
This study assessed the characteristics of cholangitis in the early post-operative period and their role in the prognosis.
Methods
Study population
The medical records of 43 patients with BA (male: female = 20:23) who underwent KPE at our institution from 2000 to 2020 were reviewed to investigate the relationship between inflammatory biomarkers and outcomes at the onset of cholangitis. Biomarkers included the white blood cell (WBC) count, neutrophil-to-lymphocyte ratio (NLR), lymphocyte ratio (lymphocytes in the total WBC count), and C-reactive protein (CRP), total bilirubin (TB), alanine aminotransferase (ALT), and γ-glutamyl transferase (γ-GTP) levels.
First, we focused on the number of cholangitis episodes in each patient in all episodes of cholangitis occurring in the native liver. Then, we focused on the inflammatory biomarkers of cholangitis before three years old. Each parameter at the onset of all episodes of cholangitis was compared between patients with native liver survival (NLS) and living-donor liver transplant (LDLT).
Surgical and post-operative management
The KPE procedure performed in this series included reconstruction with a long Roux-en-Y jejunal limb (60 cm) following portal dissection. Postoperative management included the administration of ursodeoxycholic acid and methylprednisolone (initial dose: 4 mg/kg/day) starting intravenously on post-operative day (POD) 2 for 5 days, followed by 2 mg/kg/day for 5 days, followed by oral prednisone (2 mg/kg/day) every other day for 2 months.
In addition to this regimen, the patients received sulbactam sodium 80 mg/kg/day intravenously postoperatively. After the initiation of oral intake, the regimen was switched to cefdinir (10 mg/kg/day) to further reduce the risk of post-operative cholangitis.
Definition and treatment for cholangitis
We focused on inflammatory biomarkers of cholangitis. Cholangitis was defined as a febrile episode with a body temperature of ≥ 38 °C without other obvious clinical sources of infection, as well as a combination of clinical findings. Clinical findings included the elevation of direct bilirubin at least > 1 mg/dL above the previous baseline and an ALT or γ-GTP level increase to ≥ 2 or 1.5 times the upper limit of normal, respectively [5]. Blood culture tests were not included in the results of this study because they were rarely performed in this study period. Cholangitis was treated by fasting and intravenous cefoperazone sodium/sulbactam. Antimicrobial agents were used until symptoms associated with cholangitis, such as fever and abdominal pain resolved, WBC and CRP were within reference values, and liver enzymes (TB, ALT, and γ-GTP) tended to decrease. No drainage was performed for the bile lake.
Statistical analyses
The predictive ability of the total number of cholangitis cases for the post-operative outcome over 10 years was assessed by area under the receiver operating characteristic (AUROC) curve analyses. The cutoff value was determined based on sensitivity and specificity. The Kaplan–Meier method was used to calculate the NLS. Other statistical analyses were performed using the Mann–Whitney U test for paired comparisons of serial inflammatory parameters between the NLS and LDLT groups. Statistical significance was set at p < 0.05. Continuous variables were summarized as medians and ranges.
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of the R commander designed to add statistical functions frequently used in biostatistics [6].
Ethical approval
A retrospective chart review and data collection were performed after obtaining institutional review board approval in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects by the Ministry of Health, Labor, and Welfare of Japan in 2014. This study complied with the 1964 Declaration of Helsinki (revised in 2013). It was approved by the Research Ethics Committee of Kagoshima University Hospital (registration number: 27–133). All participants and their parents provided their informed consent for registration in this study. The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Results
Clinical characteristics
The 43 patients were divided into 2 prognostic groups based on their outcomes: the NLS group (n = 30, 69.8%) and the LDLT group (n = 13, 30.2%). clinical characteristics of the NLS and LDLT groups are shown in Table 1. None of the patients had undergone primary LDLT and deceased donor liver transplant. There were no significant differences in the age at KPE between the two groups. LDLTs were performed at a median age of 1.6 years (range; 0.9–10.4). The follow-up period was significantly longer in the LDLT group than in the NLS group (17.5 vs 11.6 years, p < 0.05). Thirteen (30.2%) of the 43 patients had no episodes of cholangitis during the post-operative period, and none of these patients subsequently required LDLT.
Total episodes of cholangitis and the outcomes
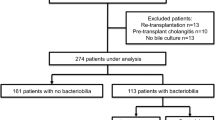
Among the 43 patients, 30 (69.8%) experienced 130 episodes of cholangitis (Fig. 1). The number of cholangitis episodes per person was significantly higher in the LDLT group than that in the NLS group (4.5 vs 2.4, p < 0.05) (Table 1).
We analyzed the NLS rate using the AUROC curve of the total number of patients with post-operative cholangitis. In the AUROC curve analysis, the cutoff value of the total number of cholangitis episodes experienced was 3, with an AUROC curve of 0.695 (95% confidence interval 0.522–0.868) (Fig. 2a). This result showed that those who had more than 3 episodes of cholangitis were likely to receive LDLT (p < 0.05) (Fig. 2b).
Comparisons of laboratory data at the time of cholangitis between the NLS and LDLT groups
Before 3 years old, 113 episodes (86.9%) of cholangitis were recognized (Fig. 3): 19 patients with 71 cholangitis episodes in the NLS group and 10 patients with 42 cholangitis episodes in the LDLT group. Table 2 illustrates the characteristics of laboratory data at the time of cholangitis occurrence before three years old. The NLR in the NLS group was approximately half that in the LDLT group (0.85 vs. 1.63, p < 0.001). Similarly, the lymphocyte ratio was significantly higher in the NLS group than in the LDLT group (47.75 vs. 33.30, p < 0.001).
The TB and γ-GTP levels in the NLS group were significantly lower than those in the LDLT group (1.2 vs. 3.0, p < 0.001, 436 vs. 668, p < 0.01, respectively). However, there was no marked difference between the groups in the WBC, CRP, or ALT values at the onset of cholangitis.
Discussion
We investigated the prognostic impact and characteristics of post-operative cholangitis in patients who underwent KPE for BA at our institution over approximately 20 years. The major findings of this study were as follows: (1) among the 43 patients, 30 experienced a total of 130 episodes of cholangitis; (2) those who had more than 3 episodes of cholangitis were more likely to undergo LDLT than those with fewer episodes; (3) cholangitis after KPE occurred before 3 years old in 86.9% of cases; and (4) the NLR at the time of cholangitis in the NLS group was about half that in the LDLT group.
Recurrent cholangitis is considered a major prognostic factor affecting the outcomes of KPE for BA. According to a recent national database study in the USA, the median number of cholangitis episodes within two years was two [7]. Similarly, in our series, episodes of cholangitis most frequently occurred before three years old, and patients with more than three episodes of cholangitis were likely to undergo LDLT. Therefore, we focused on short- to mid-term episodes of cholangitis. Multiple studies have revealed that recurrent cholangitis episodes cause progressive liver injury and fibrosis, leading to cirrhosis and liver failure [8,9,10]. This is likely due to repeated inflammation and cell damage induced by cholangitis spreading from the biliary tree [9, 11]. However, the detailed mechanism underlying the frequent incidence of cholangitis in the early post-operative period is unclear.
Several possible causes of post-operative cholangitis have been reported [2, 3, 12]. Cholangitis caused by cholestasis due to obstructive adhesions is a type of cholangitis with a clear and easily understood mechanism. In post-operative patients with good bile excretion who suddenly develop repeated episodes of cholangitis with neutrophilia, it is our clinical experience to rule out stasis in the jejunal limb [13] by hepatobiliary scintigraphy using technetium 99 m-N-pyridoxyl-5-methyl tryptophan (PMT) to evaluate the transition of bile through the Roux-en-Y limb to the upper jejunum. If there is abnormal limb retention, adhesiolysis of the limb should be recommended.
Our study suggests that cholangitis with neutrophilia is not the only cause of post-operative cholangitis. Cholangitis in the NLS group was lymphocyte-dominant and atypical in its pathogenesis. We propose the term "non-suppurative cholangitis" to describe this pathological entity more accurately. Recognizing the concept of non-suppurative cholangitis seems to provide us with insight into the etiopathogenesis of BA as well as the daily clinical management of cholangitis in BA from a different aspect.
Davenport et al. reported that the outcome of BA was predicted by six months post-KPE [14,15,16] using various immunological biomarkers, including T helper 17 (Th17) and regulatory T (Treg) cells, and serum levels of adhesion molecules. These markers, all of which are accentuated by IL-6, are not always available in daily clinical practice. In our previous report, we showed that CRP and lymphocyte counts were related to the prognosis of BA [17]. In the present study, the NLR was focused on characterizing episodes of post-operative cholangitis in addition to CRP, which is associated with elevation of IL-6. The NLR of the peripheral blood is an ordinary product of ubiquitous biomarkers that underlies the complex pathophysiological processes of systemic inflammation and immune balance and has recently been reported in patients with systemic inflammatory diseases, including cardiovascular diseases, cancer, and liver transplant patients [18,19,20].
Episodes of non-suppurative cholangitis seem to reflect an activated inflammatory environment in the BA liver, represented by elevated CRP levels, which may also potentially lead to suppurative cholangitis. This concept corresponds to a previous report on cholangitis cases that were refractory to simple antibiotic administration, which noted that clinical improvement was achieved in 60% of patients following high-dose, short-duration intravenous steroid pulse therapy [21]. The more aggressive use of steroids in the early post-operative period might interrupt the latent condition of immune-mediated flare-up, preventing diminution of bile flow, which potentially allows bacterial overgrowth in the bile duct, leading to suppurative cholangitis. Based on this context, our post-operative protocol, in which all patients receive long-term post-operative prophylactic antibiotics, was not effective.
In the present study, we demonstrated for the first time that the NLR is involved in the pathogenesis of cholangitis in BA and affects its outcome. A major limitation of our study was that the definitive diagnosis of cholangitis was symptomatic and difficult to differentiate from other viral infections. Although we evaluated episodes of cholangitis, we found that the NLR as a ubiquitous laboratory biomarker could discriminate between the two types of cholangitis and may allow us to modify our management accordingly, such as antibiotics, aggressive corticosteroid therapy, or lysis of adhesion of the Roux-en-Y limb. A prospective study is warranted to investigate lymphocyte dynamics, including regulatory T cells, to support our concept of defining suppurative and non-suppurative cholangitis, as the Th17/Treg ratio is increased in BA, as seen in autoimmune diseases and graft-versus-host disease [15, 16].
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Ernest van Heurn LW, Saing H, Tam PK (2003) Cholangitis after hepatic portoenterostomy for biliary atresia: a multivariate analysis of risk factors. J Pediatr 142(5):566–571
Luo Y, Zheng S (2008) Current concept about postoperative cholangitis in biliary atresia. World J Pediatr 4(1):14–19
Wu ET, Chen HL, Ni YH, Lee PI, Hsu HY, Lai HS, Chang MH (2001) Bacterial cholangitis in patients with biliary atresia: impact on short-term outcome. Pediatr Surg Int 17(5–6):390–395
Nio M (2017) Japanese Biliary Atresia Registry. Pediatr Surg Int 33(12):1319–1325
Venkat V, Ng VL, Magee JC, Ye W, Hawthorne K, Harpavat S, Molleston JP, Murray KF, Wang KS, Soufi N, Bass LM, Alonso EM, Bezerra JA, Jensen MK, Kamath BM, Loomes KM, Mack CL, Rosenthal P, Shneider BL, Squires RH, Sokol RJ, Karpen SJ, Childhood Liver Disease Research N (2020) Modeling outcomes in children with biliary atresia with native liver after 2 years of age. Hepatol Commun 4(12):1824–1834
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458
Chen G, Liu J, Huang Y, Wu Y, Lu X, Dong R, Shen Z, Sun S, Jiang J, Zheng S (2021) Preventive effect of prophylactic intravenous antibiotics against cholangitis in biliary atresia: a randomized controlled trial. Pediatr Surg Int 37(8):1089–1097
Madadi-Sanjani O, Schukfeh N, Uecker M, Eckmann S, Dingemann J, Ure BM, Petersen C, Kuebler JF (2021) The intestinal flora at kasai procedure in children with biliary atresia appears not to affect postoperative cholangitis. Eur J Pediatr Surg 31(1):80–85
Baek SH, Kang JM, Ihn K, Han SJ, Koh H, Ahn JG (2020) The epidemiology and etiology of cholangitis after kasai portoenterostomy in patients with biliary atresia. J Pediatr Gastroenterol Nutr 70(2):171–177
Cheng K, Molleston JP, Bennett WE Jr (2020) Cholangitis in patients with biliary atresia receiving hepatoportoenterostomy: a national database study. J Pediatr Gastroenterol Nutr 71(4):452–458
Houben C, Phelan S, Davenport M (2006) Late-presenting cholangitis and Roux loop obstruction after Kasai portoenterostomy for biliary atresia. J Pediatr Surg 41(6):1159–1164
Ecoffey C, Rothman E, Bernard O, Hadchouel M, Valayer J, Alagille D (1987) Bacterial cholangitis after surgery for biliary atresia. J Pediatr 111(6 Pt 1):824–829
Muraji T, Tsugawa C, Nishijima E, Satoh S, Takamizawa S, Ise K, Maekawa T (2002) Surgical management for intractable cholangitis in biliary atresia. J Pediatr Surg 37(12):1713–1715
Narayanaswamy B, Gonde C, Tredger JM, Hussain M, Vergani D, Davenport M (2007) Serial circulating markers of inflammation in biliary atresia–evolution of the post-operative inflammatory process. Hepatology 46(1):180–187
Hill R, Quaglia A, Hussain M, Hadzic N, Mieli-Vergani G, Vergani D, Davenport M (2015) Th-17 cells infiltrate the liver in human biliary atresia and are related to surgical outcome. J Pediatr Surg 50(8):1297–1303
Yang Y, Liu YJ, Tang ST, Yang L, Yang J, Cao GQ, Zhang JH, Wang XX, Mao YZ (2013) Elevated Th17 cells accompanied by decreased regulatory T cells and cytokine environment in infants with biliary atresia. Pediatr Surg Int 29(12):1249–1260
Harumatsu T, Muraji T, Sugita K, Murakami M, Yano K, Onishi S, Yamada K, Yamada W, Matsukubo M, Kawano T, Muto M, Kaji T, Ieiri S (2022) The preoperative lymphocyte ratio and postoperative C-reactive protein are related to the surgical outcome in biliary atresia: an analysis of serial ubiquitous markers of inflammation. Pediatr Surg Int 38(12):1777–1783
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS (2008) Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol 102(6):653–657
Meng XY, Guo XG, Wang HQ, Pan ZY, Lu YG, Yu WF (2020) Baseline neutrophil-lymphocyte ratio is associated with survival for infant living donor liver transplantation for biliary atresia. Pediatr Transplant e13933
Lorente D, Mateo J, Templeton AJ, Zafeiriou Z, Bianchini D, Ferraldeschi R, Bahl A, Shen L, Su Z, Sartor O, de Bono JS (2015) Baseline neutrophil-lymphocyte ratio (NLR) is associated with survival and response to treatment with second-line chemotherapy for advanced prostate cancer independent of baseline steroid use. Ann Oncol 26(4):750–755
Rothenberg SS, Schroter GP, Karrer FM, Lilly JR (1989) Cholangitis after the Kasai operation for biliary atresia. J Pediatr Surg 24(8):729–732
Acknowledgements
We thank Mr. Brian Quinn for his comments and assistance with this manuscript. This study was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS: 23K08052, 23K11934, 22K02859, 22K02918, 22K07848, 22K07894, 22K08719, 22K08757, 22K08758, 22K12888, 22K15925, 21H00908, 21K07867, 21K08623, 21K12754), a research grant from The Mother and Child Health Foundation, and a research grant from the Kawano Masanori Memorial Public Interest Incorporated Foundation for Promotion of Pediatrics.
Author information
Authors and Affiliations
Contributions
H.T., M.T. and I.S. wrote the manuscript. T.Y., I.Y., O.M., K.C., M.M., and Y.K. prepared tables and figures. M.R., N.A., S.K., O.S., and M.M. reviewed the literature. K.T., K.T., and I.S. provided conceptual advice. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harumatsu, T., Muraji, T., Masuya, R. et al. Inflammation patterns in early post-operative cholangitis predict long-term outcomes in biliary atresia: a potential role of non-suppurative cholangitis. Pediatr Surg Int 40, 190 (2024). https://doi.org/10.1007/s00383-024-05774-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-024-05774-1