Abstract
Purpose
To assess the efficacy of transcatheter arterial embolization (TAE) plus propranolol treatment for infantile hepatic hemangioma (IHH).
Methods
A retrospective study of symptomatic IHH and hemodynamic changes in IHH was conducted between 2016 and 2019.
Results
There were five boys and seven girls with diffuse lesions (n = 7) and multifocal lesions (n = 5). Hepatomegaly and abdominal distension (n = 6) were the predominant clinical presentations. Seven patients (58.3%) had multiple cutaneous hemangiomas. Pulmonary arterial hypertension, heart failure (n = 4), and hypothyroidism (n = 4) were observed. A total of 17 TAE procedures were performed in 12 IHH cases, with a technical success rate of 100%. All patients received standard propranolol orally, and one patient was orally administered metacortandracin. Two patients died of heart failure and multiple organ dysfunction caused by an enlarged liver. In addition, one patient was not reexamined after discharge. Of the remaining nine children, the average follow-up time was 10.78 months (range 2–28 months), and they all responded well to TAE combined with oral propranolol.
Conclusion
TAE combined with propranolol is safe and effective for the treatment of IHH, demonstrating low complication rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infantile hepatic hemangioma (IHH) is the most common benign vascular tumor of the liver in neonates. It has been used to describe a variety of hepatic vascular anomalies or hypervascular tumors, such as venous malformations, hereditary hemorrhagic telangiectasia, hepatic arteriovenous malformations, hepatic adenomas, and portal vein aneurysms [1]. IHHs are different from vascular lesions in the liver in adults and are rare angiogenic tumors with a variety of clinical presentations ranging from spontaneous regression to life-threatening complications [2]. Τhe true incidence of IHH remains undetermined, as many small lesions are asymptomatic and unidentifiable [3]. Approximately 90% of IHH cases are diagnosed within the age of 6 months, and 30% are detected 3 months prior [4].
Most cases of IHH may present as asymptomatic and are only occasionally detected on abdominal ultrasound or present as hepatomegaly or abdominal distention. Although IHH is benign, it can result in life-threatening complications [5]. The presence of an arteriovenous shunt within an IHH lesion may lead to life-threatening congestive heart failure in 50–60% of patients [1]. The mortality rate is estimated at 11–18% because of acute congestive heart failure and abdominal compartment syndrome, which are severe complications of IHH [6].
Observations are used for most asymptomatic in multifocal IHH [3]. Propranolol has replaced corticosteroids as the current pharmacotherapy gold standard for the treatment of IHHs [7,8,9]. However, first-line pharmacotherapy with propranolol has reduced, but not abolished, the need for surgical intervention [10]. Diffuse lesions invariably have a significant effect on systematic hemodynamics [10], and most untreated diffuse and multifocal IHH cases progress to high-output congestive heart failure [11, 12]. Transcatheter arterial embolization (TAE), a method of reducing shunts and counteracting cardiac failure, can theoretically be used as an effective complementary therapy to propranolol in the treatment of severe IHH. In this report, we retrospectively reviewed the outcomes of TAE and oral administration of propranolol for IHH, which could be useful for improving the management of IHH and patient outcomes. All the patients agreed to publish their case details and images.
Materials and methods
Patients
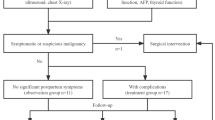
Sixty-eight patients with known multifocal and diffuse subtypes of symptomatic IHH were enrolled from October 2016 to December 2019 at our hospital. Hemangioma was diagnosed based on clinical presentations and preoperative ultrasound, spiral computed tomography, or magnetic resonance imaging. Of these, 56 patients with mild symptoms were treated with oral propranolol alone. A total of 12 patients diagnosed with IHH were included in our study. All of them had clinical symptoms or lesions that were more than half the size of the liver on imaging, with manifestations of hemodynamic changes such as accelerated blood flow and pulmonary hypertension (Fig. 1). Once they have common comorbidities, such as infection, they are more likely to develop serious complications, such as respiratory failure and heart failure. Therefore, the patient was treated with interventional embolization in combination with oral propranolol. This retrospective study was approved by the Ethics Committee of the Children’s Hospital affiliated with Shandong University.
Detection of patient complications
All patients underwent echocardiography to assess arteriovenous shunting, ventricular overload, and pulmonary hypertension. Consumption coagulopathy was evaluated using platelet levels and coagulation, including fibrinogen, d-dimer, activated partial thromboplastin time, and prothrombin time. The presence of hypothyroidism was assessed based on free triiodothyronine, free thyroxine, and thyroid-stimulating hormone levels.
Treatment protocol
TAE is indicated only after examination of patients with IHH. The pingyangmycin-lipiodol emulsion (PLE) used in the protocol included pingyangmycin (8–12 mg/m2) and lipiodol (20–33%, v/v), and the total amount of emulsion was 6–12 ml. It was performed by interventional radiologists under general anesthesia for all TAE. The femoral artery was punctured using the Seldinger technique, and 75–100 IU/kg heparin was administered to avoid thrombosis. The celiac artery was catheterized using a 4-F Cobra guide catheter (Terumo, Tokyo, Japan) under X-ray guidance. We obtained the location, number, size, staining characteristics, and blood supply of the IHH using arteriograms (Fig. 2). A 2.6-F microcatheter was selectively catheterized into the feeding artery under fluoroscopy, and an angiogram of the tumor was obtained. We then infused the PLE directly through the microcatheter until the periphery of the hemangioma was completely surrounded, and subsequently performed polyvinyl alcohol (PVA 300–500 µm) embolization of the feeding artery. Selective celiac arteriography performed once again is necessary to determine the degree of embolism of the supplying arteries. When there is an obvious arteriovenous shunt, gelatin sponge particles or spring coils should be used for embolization before the PLE injection.
Unlike liver malignancies, TAE for IHH provides more rapid resolution of potentially life-threatening arteriovenous shunt conditions. Therefore, elimination of the visible arteriovenous shunt is sufficient and complete IHH devascularization is not recommended to avoid unnecessary complications. In our study, complete or partial resolution of the arteriovenous shunt, with > 75% IHH devascularization on the completion angiogram, defined TAE treatment as successful.
Oral propranolol at 2 mg/kg/day for three doses, which was changed to two times after 2 weeks, was started in all patients. In patients with heart failure, propranolol was started at a dose of 1 mg/kg/day plus oral metacortandracin at 3.0 of 5 mg/kg every other day. We have a similar patient who experienced cardiac arrest after 2 mg/kg/day of propranolol orally. If the clinical situation was stable, we gradually increased the propranolol dose to 2 mg/kg/day and discontinued oral metacortandracin therapy.
Clinical evaluation
Detailed clinical examinations including liver function, thyroid function, and echocardiography were performed to assess the patient's condition. Ultrasonography is routinely performed to assess the regression of hemangioma. Computer tomography (CT) or magnetic resonance imaging (MRI) was performed every 3–6 months to observe changes in tumor size. In patients whose lesions disappeared, treatment was discontinued. Otherwise, treatment was ended after 1.5 years of duration in all patients.
Efficacy evaluation criteria for IHH are divided into the following categories [13, 14]: 1. Complete response, defined as the complete disappearance of either the lesion and/or symptoms; 2. partial response (PR), defined as a reduction of > 20% in lesion size and improvement in symptoms and disappearance of imaging signs of hemodynamic disturbance; 3. progressive disease, defined as an enlargement of > 20% in the size of the lesion or appearance of new lesions, 4. stable disease was defined based on none of the above criteria.
We recorded data including age, sex, clinical presentations, laboratory examination, imageological examination (ultrasound, spiral CT, or MRI), treatment, and prognosis.
Results
Patient characteristics
This study retrospectively reviewed 12 patients with IHH (7 patients (58.3%) were female and 5 (41.7%) were male). The median age of the patients was 4.01 months (range 0.63–8.77 months) and the average weight of patients was 5.85 kg (range 3.0–10.0 kg). The important clinical features are listed in Table 1.
Of the 12 infants, 7 had diffuse lesions with multiple lesions with almost complete parenchymal replacement, and another 5 had multifocal lesions with intervening segments of normal parenchyma. Seven cases (58.3%) were accompanied by multiple cutaneous hemangiomas, and as many as eight lesions were found in Case #5. Six patients demonstrated symptoms of hepatomegaly or abdominal distension. Three of the children had no obvious clinical symptoms and were detected during physical ultrasound examination because of cutaneous hemangiomas. In addition, two children presented with respiratory distress and one patient presented with vomiting. Four patients had pulmonary arterial hypertension and heart failure (HF). There were four cases of hypothyroidism and no patients with abdominal compartment syndrome.
Treatment outcome
A total of 17 TAE procedures were performed in 12 IHH cases, with a technical success rate of 100%. Gelatin sponge particle (350–560 µm) embolization of the feeding artery was performed in one case because the blood supply to the artery was faster. In the other case, which presented with a very severe arteriovenous shunt, as shown by angiography, the artery was embolized with a spring coil. All patients received standard propranolol orally and one case had propranolol treatment combined with oral metacortandracin. No serious therapy-related complications were observed.
Two patients died of HF and multiple organ dysfunction caused by an enlarged liver. In addition, one patient was not reexamined after discharge. For the remaining nine children, the average follow-up time was 10.78 months (range 2–28 months). Six children presented with complete remission of lesions and three cases presented with PR whose imaging signs of hemodynamic disturbance disappeared. There was sparse vascular density in the lesions of the two cases on Doppler ultrasonography, and we treated them clinically as a cure and stopped the follow-up propranolol orally. The mortality rate for diffuse lesions was 33.3% (2/6), which was higher than that for multifocal lesions (0%, 0/5). However, the mortality rate in IHH with pulmonary arterial hypertension and HF is as high as 66.7% (2/3). In addition, the physical examination results of the remaining nine cases were normal in all children, and hypothyroidism returned to normal.
Discussion
IHH is the most common benign tumor of the liver in infancy, with three variants identified on the basis of imaging characteristics: focal, multifocal, and diffuse [14]. However, focal lesions are not true IHHs because they test negative for glucose transporter 1 (GLUT-1), but are analogous to a rapidly involuting congenital hemangioma lesion [14]. Unlike focal lesions, the multifocal and diffuse subtypes test positive for GLUT-1 and resemble true IHH cases [14]. The natural history of IHHs and their cutaneous counterparts is characterized by a period of rapid postnatal proliferation followed by a plateau and eventual spontaneous involution [10]. Many infants with hepatic hemangiomas also have multiple cutaneous hemangiomas. In our study, 58.3% of IHH cases exhibited this phenomenon. A recent prospective study suggested that abdominal ultrasonography is recommended for children younger than 9 months of age who present with five or more cutaneous IHHs [15].
Although asymptomatic lesions spontaneously regress, symptomatic lesions require aggressive treatment because they pose potential risk of death [16]. Multifocal IHH is usually asymptomatic and demonstrates arteriovenous shunts on angiography, and high-output cardiac failure can be seen in some patients [17]. Furthermore, excessive arteriovenous shunts resulted in severe pulmonary congestion, which marked the interstitial fluid increase and raised the alveolar and airway mucosa edema, which was subjected to secondary infection, making patients vulnerable to severe pneumonia [18]. In addition, diffuse lesions may cause hepatomegaly, which compresses the inferior vena cava, diaphragm, and surrounding tissues, and can result in abdominal compartment syndrome [17]. IHH can cause hypothyroidism due to the overproduction of iodothyronine deiodinase type 3 [19], an enzyme that deiodinates thyroxin and converts it into the biologically inactive form, triiodothyronine [16]. If left untreated, hypothyroidism can lead to ineffective myocardial contractility and HF in the early stages, and may potentially to mental retardation and developmental delays later on in life [17]. The 12 cases in this study had a variety of clinical manifestations. Hepatomegaly and abdominal distension (n = 6) were the predominant clinical presentations. Of the four cases with pulmonary arterial hypertension and HF, two patients had severe pulmonary congestion. Finally, two patients died of four IHHs with pulmonary arterial hypertension and HF. Hypothyroidism (n = 4) was also observed among a few cases.
Most multifocal and diffuse HHs can be managed satisfactorily by propranolol orally [10, 20]. Varrasso et al. [7] found that IHH showed a slight reduction in size at the 6th week, a significant regression at 12 months, and a complete regression at 24 months of treatment with oral propranolol at 2 mg/kg/day. Tasseh et al. [21] reported that the IHH tumor was reduced by 20% after oral propranolol at 2 mg/kg/day for 1 month and 48% for 8.5 months, and there were no propranolol-related complications during the entire duration of treatment. Since propranolol was introduced to treat IHHs in 2008, the rate of surgical intervention has decreased by nearly 90% [14]. Some patients who present with a significant hemodynamic shunt and severe hypothyroidism should initially receive propranolol orally [3]. Propranolol is regarded as therapeutic and not contraindicated in patients with HF [17]. However, in our study, Case #2 developed cardiac arrest after the oral administration of propranolol. Nine post-TAE patients achieved an encouraging prognosis except for the other patients who died because of severe IHH complications. No significant adverse effects related to propranolol were observed, regardless of whether it was combined with IHH complications.
In addition to propranolol, Faik et al. [17] administered a single 7-day course of prednisolone to all patients with IHH. They suggested that steroids may increase the activity of propranolol. The combination of oral steroids and propranolol can rapidly improve clinical symptoms and prevent complications associated with systemic arteriovenous shunting [11]. Özdemir et al. [16] reported that their patients responded to combined therapy with steroids and propranolol, and considered it useful in patients with severe symptoms. Aly et al. [22] also reported the superiority of propranolol in combination with prednisolone treatment. Propranolol and prednisone were also administered orally to patient #4 in this study; however, the child died due to the severity of the condition.
Multimodal therapy is necessary to achieve satisfactory symptom control in selected cases [10]. Thus, therapy for severe IHH aims at remission of the primary tumor and rapid resolution of life-threatening systemic hemodynamics. Selective hepatic artery ligation to stabilize infants by reducing arteriovenous shunting was first reported in 1967, and provided time for tumor regression [23]. It has become a promising treatment method for symptomatic hepatic hemangiomas because of the minimally invasive nature of interventional radiology [24]. Warmann et al. [25] performed TAE to block the blood-supplying artery using spring coils for four IHH infants with symptomatic hepatic hemangioendothelioma, and three of them showed significant improvement after TAE for focal lesions at 54 months. IHH treated with TAE has a low incidence of complications, especially in infants with lesions involving two liver lobes and those in relatively poor condition. Superselective angiography can clearly and accurately show an IHH and the culprit vessel of the tumor [24]. It does not lead to hepatic necrosis because of adequate hepatic oxygenation, and perfusion is maintained via portal venous flow [10]. Pingyangmycin can induce apoptosis of endothelial cells in the splenic sinus through the caspase-3 activation pathway, resulting in endothelial cell necrosis and fibroblast proliferation [26]. Lipiodol has been widely used in medical practice for emulsification and embolization of tumor microcirculation [27]. Moreover, staged procedures are prudent in minimizing the risk of hepatic necrosis and death [28]. In this study, all 12 children were treated with TAE, and 5 of them were treated with TAE twice. For two children with significant arteriovenous shunt, the block was first performed with spring-coil or gelatin sponge particles, and then effective embolization was performed by PLE and PVA during the 1st TAE. Encouragingly, the clinical condition was relieved in all the children, and no significant complications of TAE were observed.
Because IHH is a common infantile hemangioma, it tends to occur in younger infants. Small adults cannot be considered, and the differences are greater among younger children and adults. Infants and young children with critical illnesses may die suddenly due to mild symptoms. Attention should be paid to the following aspects of the TAE: 1. Infants have immature kidney function, and are prone to fluid and electrolyte disorders. The amount of contrast agent needed to be controlled during surgery, and renal function should be protected after surgery. 2. The femoral arteries are thinner in pediatric patients than in adults, and physicians should be proficient in puncture techniques. 3. The blood vessels of infants are prone to spasm, which brings certain difficulties to embolization, and the operation must be gentle. 4. Finally, it is important to maintain the child's body temperature during surgery.
Notably, IHH-induced hypothyroidism is resistant to normal doses of l-thyroxine and may require high doses within the range of 22–70 µg/kg/day [28]. Unfortunately, we do not have specific data on the dose of l-thyroxine because these children were regulated in the Department of Endocrinology, which is also a shortcoming of this article. However, it is important to note that they all ended up being cured. Our study was limited by its small retrospective design. Notably, the clinical value of additional TAE remains unknown and must be weighed against the potential risk of intra-arterial embolization in infants. At this point, TAE cannot be routinely recommended for IHH treatment; however, if embolization is performed for IHH with high arteriovenous shunting, patients should be managed with systemic therapy immediately after achieving a good prognosis.
Conclusions
Through the retrospective study which patients with IHH undergoing TAE and propranolol orally at our hospital in China, we describe a minimally invasive procedure with promising results for the treatment of IHH with a very low complication rate. Successful treatment with TAE and oral propranolol appears promising and deserves further attention among physicians.
References
Iacobas I et al (2018) Guidance document for hepatic hemangioma (infantile and congenital) evaluation and monitoring. J Pediatr 203:294-300 e2
Sondhi V et al (2012) Successful management of multi-focal hepatic infantile hemangioendothelioma using TACE/surgery followed by maintenance metronomic therapy. BMJ Case Rep. https://doi.org/10.1136/bcr.12.2011.5456
Zavras N et al (2020) Infantile hepatic hemangioma: current state of the art, controversies, and perspectives. Eur J Pediatr 179(1):1–8
Razon MJ et al (1998) Increased apoptosis coincides with onset of involution in infantile hemangioma. Microcirculation 5(2–3):189–195
Lerut J, Iesari S (2018) Vascular tumours of the liver: a particular story. Transl Gastroenterol Hepatol 3:62
Rialon KL et al (2015) Risk factors for mortality in patients with multifocal and diffuse hepatic hemangiomas. J Pediatr Surg 50(5):837–841
Macdonald A et al (2020) Historical and contemporary management of infantile hepatic hemangioma: a 30-year single-center experience. Ann Surg 275(1):e250–e255
Chatmethakul T et al (2016) Infantile hepatic hemangioendothelioma: an uncommon cause of persistent pulmonary hypertension in a newborn infant. AJP Rep 6(3):e260–e263
Varrasso G et al (2017) Propranolol as first-line treatment for life-threatening diffuse infantile hepatic hemangioma: a case report. Hepatology 66(1):283–285
Tsai MC, Liu HC, Yeung CY (2019) Efficacy of infantile hepatic hemangioma with propranolol treatment: a case report. Medicine (Baltimore) 98(4):e14078
Krowchuk DP et al (2019) Clinical practice guideline for the management of infantile hemangiomas. Pediatrics 143(1):e20183475
Wang L et al (2020) Infantile hepatic hemangioendothelioma associated with pulmonary artery hypertension and cardiac insufficiency successfully treated with transcatheter arterial embolization and propranolol: a case report. Medicine 99(24):e20728
Adams DM et al (2016) Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics 137(2):e20153257
Tian R et al (2020) Propranolol for infantile hepatic hemangioendothelioma: clinical evaluation of drug efficacy and safety using a single-center patient cohort. Ann Hepatol 19(5):530–534
Lekwuttikarn R, Josephs S, Teng JM (2019) Successful medical management of life-threatening hepatic hemangioma in neonates. Pediatrics 144(4):e20191339
Ji Y, Chen S, Yang K, Xiang B, Jiang X, Xu X, Li L, Qiu T, Zhou J, Dai S, Zhang X, Lu G, Kong F, Yang G, Qiu Q (2021) Screening for infantile hepatic hemangioma in patients with cutaneous infantile hemangioma: a multicenter prospective study. J Am Acad Dermatol 84(5):1378–1384. https://doi.org/10.1016/j.jaad.2020.11.062
Ozdemir ZC et al (2017) Beta blocker and steroid therapy in the treatment of infantile hepatic hemangioendothelioma. Drug Discov Ther 11(3):161–164
Sarialioglu F et al (2017) A new perspective for infantile hepatic hemangioma in the age of propranolol: experience at Baskent University. Exp Clin Transplant 15(2):74–78
Wang T et al (2015) Infantile hepatic hemangioendothelioma associated with congestive heart failure: two case reports with different outcomes. Medicine 94(52):e2344
Brown J, Arora R, Sethuraman U (2018) Distributive shock in a neonate with diffuse infantile hepatic hemangioma. J Emerg Med 54(1):e1–e3
Yang K et al (2019) Efficacy of propranolol treatment in infantile hepatic haemangioma. J Paediatr Child Health 55(10):1194–1200
Al Tasseh F et al (2017) Diffuse hepatic hemangioma with single cutaneous hemangioma: an alerting occurrence. Clin Case Rep 5(6):887–890
Aly MM et al (2015) Therapeutic superiority of combined propranolol with short steroids course over propranolol monotherapy in infantile hemangioma. Eur J Pediatr 174(11):1503–1509
deLorimier AA et al (1967) Hepatic-artery ligation for hepatic hemangiomatosis. N Engl J Med 277(7):333–337
Dong W et al (2019) Invasive management of symptomatic hepatic hemangioma. Eur J Gastroenterol Hepatol 31(9):1079–1084
Warmann S et al (2003) Interventional treatment of infantile hepatic hemangioendothelioma. J Pediatr Surg 38(8):1177–1181
Huang Y et al (2014) Proapoptotic effect and the mechanism of action of pingyangmycin on cavernous hemangiomas. Exp Ther Med 7(2):473–477
Gaba RC, Schwind RM, Ballet S (2018) Mechanism of action, pharmacokinetics, efficacy, and safety of transarterial therapies using ethiodized oil: preclinical review in liver cancer models. J Vasc Interv Radiol 29(3):413–424
Acknowledgements
I would particularly like to acknowledge my team members for their wonderful collaboration and patient support. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; and made final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, L., Li, J., Song, D. et al. Clinical evaluation of transcatheter arterial embolization combined with propranolol orally treatment of infantile hepatic hemangioma. Pediatr Surg Int 38, 1149–1155 (2022). https://doi.org/10.1007/s00383-022-05143-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05143-w