Abstract
Purpose
Although we generally perform thoracoscopic lobectomy for congenital lung cysts (CLCs), we recently began performing thoracoscopic-limited pulmonary resection (segmentectomy or small partial lung resection) on relatively small lesions and on lesions involving multiple lobes. Our study aimed to determine the therapeutic outcomes of thoracoscopic CLC surgery.
Methods
We retrospectively reviewed patients aged ≤ 18 years who underwent their first CLC surgery at our facility between 2013 and 2020.
Results
A comparison between patients < 4 months old and those ≥ 4 months old showed no significant difference in operating time or incidence of complications. Blood loss volume (mL/kg) was significantly greater in patients < 4 months old and in patients who had undergone semi-urgent or urgent surgery. Operating time and postoperative complications were not increased in semi-urgent or urgent surgeries. There was no significant difference in operating time, blood loss volume, or postoperative complications between patients with a preoperative history of pneumonia and patients with no such history.
Conclusion
In most patients, thoracoscopic surgery for CLC was safely performed. Limited pulmonary resection is considered difficult to perform thoracoscopically in children, but can be safely performed using new devices and navigation methods.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
When a patient presents without critical cardiorespiratory dynamics, thoracoscopic surgery is the preferred treatment choice especially for congenital lung cysts (CLCs) as it is minimally invasive, tends not to result in thoracic deformities, and has a quick postoperative recovery time. Generally, we perform thoracoscopic lobectomy for the treatment of CLCs, as the commonly used devices are not suitable in small working spaces and due to peculiar anatomical characteristics of children, such as incomplete lobulation. However, in adults, reduction surgery based mainly on segmentectomy is gradually becoming the standard operative procedure, even for lung cancer cases, and research is ongoing concerning less-invasive surgical procedures [1, 2]. Reduction surgery requires a surgeon to differentiate between pulmonary segments and to have a good knowledge of the anatomy of complex blood vessels and bronchi. It also requires detailed preoperative assessment, high-level surgical techniques, and suitable devices in terms of size and methodology. Almost all cases of CLC are benign disorders in children who have a longer postoperative lifespan than adults. Therefore, it is important to conserve as much healthy lung tissue as possible, and thus, reduction surgery is more beneficial.
After acquiring a 5 mm automatic anastomotic device and introducing an indocyanine green (ICG) navigation method, we began to attempt thoracoscopic-limited pulmonary resection on relatively small lesions and on lesions spanning multiple lobes. This study aimed to determine the therapeutic outcomes of thoracoscopic surgery for CLC and to assess the use of this surgical technique at our hospital.
Materials and methods
This study was approved by the Ethics Committee at our institution (approval number 2019-0429) and written informed consent was obtained from the patients or their parents/caregivers. Patient characteristics, surgical procedures, perioperative complications, and postoperative course were investigated retrospectively in patients aged ≤ 18 who had undergone their first surgery for CLC at our facility between December 1, 2013, and January 31, 2020. Patients for whom we attempted thoracoscopic surgery were included in our data analysis. One patient who first opted for thoracotomy was excluded from the analysis of operative data. For categorical variables, statistical comparisons were made using Fisher’s exact or Chi-square tests, and continuous variables were compared using Wilcoxon’s signed-rank test. We used JMP Pro® version 15 software (SAS Institute Inc., Cary, NC, USA) to analyze the data. A p value < 0.05 was considered statistically significant.
Thoracoscopic surgery for congenital lung cysts
Surgery was performed under general anesthesia with intubation, generally without one-lung ventilation, and with 3–8 mm of induced pneumothorax. Surgery was performed with the patients in the lateral decubitus position with a 5 mm camera port, two 5 mm ports for the surgeon, and one or two 3 mm ports for the assistant. Resected lung tissue was removed by widening the least noticeable wound to 1–2 cm. A 10–12 mm camera port was also occasionally used for larger bodied patients aged between 10 and 18 years. ICG fluorescence navigation was performed using 1–5 intravenous 0.01–0.02 mg/kg injections of ICG; then blood flow was assessed using a near-infrared fluorescent camera (OPAL1®ICG/NIR system, Karl Storz). In 2019, we acquired a 5 mm automatic anastomotic device and began resecting bronchi and lungs. We also started to perform segmentectomies.
Results
Characteristics of patients who underwent thoracoscopic resection
Thoracotomy was planned for only one patient preoperatively due to severe respiratory failure (Case 1, Table 8). All other patients underwent thoracoscopic surgery as the first surgery. The patients in this study comprised 32 males and 33 females (total, n = 65). Patient diagnoses were congenital pulmonary airway malformation (CPAM) (n = 37), bronchial atresia (n = 9), intralobar pulmonary sequestration (n = 8), and extralobar pulmonary sequestration (n = 11) (Table 1).
The following operative procedures were performed: lobectomy (39 patients), lobectomy plus partial lung resection (7 patients), lobectomy plus segmentectomy (1 patient), sequestrectomy (11 patients), partial lung resection (4 patients), segmentectomy (2 patients), and pneumonectomy (1 patient). Out of the 65 patients in this study, the procedure was converted to a thoracotomy in 1 patient due to difficulties in maintaining anesthesia and in another patient, it converted to thoracotomy due to hemorrhage. Both patients’ case notes indicated that securing a visual field was difficult due to hyperinflation of the lungs. Forty-five patients (69%) were diagnosed prenatally. The remaining 20 patients were diagnosed due to early postnatal pneumothorax or respiratory failure (n = 6), pneumonitis (n = 9), sequestrated lung torsion (n = 2), and incidentally (n = 3). Urgent surgery was required for 8 patients, semi-urgent surgery was required for 6 patients, and 51 patients underwent scheduled surgery. Urgent surgery was required due to respiratory failure early postnatally in 7 infants and torsion of extralobar sequestration in 1 10-year-old patient. Semi-urgent surgery was required due to progression of respiratory problems postnatally in 6 infants and torsion of extralobar sequestration in 1 patient (age, 5 years; transferred after diagnosis of a lung tumor from another hospital) (Table 1).
Operative profile of patients who underwent thoracoscopic surgery
Congenital lung cysts without extralobar sequestration
Among 54 patients (excluding those who had undergone extralobar sequestration), the median age at surgery was 0 years (quartile points, 0–0)/168 days (quartile points, 40–315 days), the median weight at surgery was 6.76 kg (quartile points, 3.98–8.56), the median operating time was 193 min (quartile points, 155–237 min), the median blood loss volume was 1.4 mL (quartile points, 0.28–7.4 mL), and the median postoperative duration of hospitalization was 7 days (quartile points, 4–17 days) (Table 2).
Extralobar sequestration only
Among 11 patients who had undergone extralobar sequestration, the median age at surgery was 0 years (quartile points, 0–5)/257 days (quartile points, 173–1922 days), the median weight at surgery was 8.08 kg (quartile points, 7.63–18.0), the median operating time was 70 min (quartile points, 58–102), the median blood loss volume was 0.0 mL (quartile points, 0.0–0.5), and the median postoperative duration of hospitalization was 4 days (quartile points, 3–6) (Table 3).
Postoperative complications of thoracoscopic surgery
Follow-up surgeries for postoperative complications were performed on 2 patients with bronchial fistula, 1 patient with middle-lobe torsion after right inferior lobectomy, and 1 patient with postoperative bleeding. In the patient who underwent further surgery, the hemorrhage was a complication of a third scheduled surgery rather than the first surgery. Using the Clavien–Dindo classification (grade III or higher), postoperative complications comprised subcutaneous emphysema (n = 1 patient) and pneumothorax (n = 1 patient), and a thoracostomy tube was placed in both patients. One patient with subcutaneous emphysema was readmitted for observation; however, this patient did not require any further surgical treatment (Table 4).
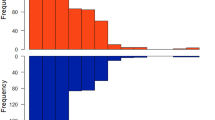
Comparison of ages, scheduled operations, and a diagnosis of pneumonia
Excluding 11 patients who had undergone sequestrectomy for extralobar sequestration, we evaluated the operating time, blood loss, and postoperative complications in the remaining 54 patients. A comparison between 18 patients aged < 4 months and 36 patients aged ≥ 4 months showed no significant difference in operating time (p = 0.797) nor in the incidence of postoperative complications (p = 0.651); however, the volume of blood loss per body weight was found to be significantly greater in patients aged < 4 months than in those ≥ 4 months (p = 0.0281) (Table 5). A comparison between 12 patients who underwent semi-urgent or urgent surgery and 42 patients who underwent scheduled surgery showed that patients who underwent semi-urgent/urgent surgery were significantly younger (p = 0.0001) and had significantly greater blood loss per body weight compared to those that underwent scheduled surgeries (p = 0.00098); however, no significant difference was found in operating times (p = 0.942) or the incidence of postoperative complications (p = 0.729) (Table 6). A comparison between 9 patients with preoperative histories of pneumonia and 45 patients without such histories revealed no significant difference in operating time (p = 0.451), blood loss volumes per body weight (p = 0.529), or postoperative complications (p = 1.0000) between these two groups of patients. Patients with a history of pneumonia were significantly older (p = 0.0001) (Table 7).
Affected lesions spanning multiple lobes (n = 9 patients)
The 9 patients with affected lesions spanning multiple lobes had the following operative procedures: lobectomy plus partial lung resection (n = 7 patients), partial lung resection (n = 1 patient; Case 2), and lobectomy plus segmentectomy (n = 1 patient; Case 9). At primary surgery, the median age was 101 days, the median weight was 3.71 kg, the median operating time was 218 min, the median blood loss volume was 5 mL, and none of these patients developed surgical complications. In 2 patients, residual lesions were suspected following postoperative computed tomography (CT) scans (Table 8).
Case 1 was the only one in which thoracoscopic surgery was not attempted. This was an extremely low birth weight male infant born at a gestational age of 25 weeks and 2 days, and weighed 679 g. After the age of 70 days, the respiratory status of this patient deteriorated and he was transferred to our hospital due to difficulties in managing his condition. At the age of 249 days, we performed a right lower lobectomy and partial resection of the superior lobe via thoracotomy. There were no postoperative complications and nor residual lesions.
In Case 2, CLCs had spread to almost the entire left lung, and respiration remained irregular after birth. A strategy of early surgery was adopted due to persistent chest retractions. At the age of 27 days, a thoracoscopic partial lung resection was performed to reduce mediastinal shift. Although there was a large and grossly visible area indicating a residual lesion, we opted to wait for the patient to grow and planned a staged surgery. Respiration stabilized postoperatively and the patient was discharged on postoperative day 21. A second surgery (thoracotomy segmentectomy of S1 + 2, 4, 9 + 10) was performed when the patient was 2 years old (811 days), and a third surgery (thoracotomy segmentectomy plus cystectomy S1 + 2 of residual lesion, S3 cyst and S8 segment removal) was performed at 3 years of age (1098 days). The chest was reopened for hemostasis due to postoperative bleeding during the third surgery. A residual lesion was found after the third surgery; however, due to the small size of the lesion, this patient continues to be observed during follow-up visits (Fig. 1).
Case 2: Pre-and postoperative evaluation using computed tomography scans. At 27 days of age, thoracoscopic partial resection was performed to improve mediastinal shift. A second surgery (thoracotomy segmentectomy of S1 + 2, 4, 9 + 10) was performed at the age of 2 years, and a third surgery (thoracotomy segmentectomy plus cystectomy S1 + 2 of residual lesion, S3 cyst, and S8 segment removal) was performed at the age of 3 years. A small residual lesion was identified following the third surgery (in a circle)
The remaining 7 patients (cases 3–9) underwent thoracoscopic surgery involving either lobectomy plus partial lung resection or segmentectomy, with the aim of complete lesion removal during the first surgery. Comparing these 7 patients with another 39 patients who had undergone simple lobectomy for lesions that were isolated to a single lobe revealed no difference in operating time (p = 0.130), blood loss in mL/kg (p = 0.502), or in the incidence of postoperative complications (p = 0.570) (Table 9).
Case 8 (Table 8) was prenatally diagnosed with CPAM. There were no postnatal respiratory issues; therefore, the patient was observed at home, but was admitted for pneumonitis 6 months after birth. At 235 days of age, we performed a thoracoscopic left superior lobectomy plus partial lung resection of S6. A small residual lesion found in S6 postoperatively showed no signs of growth 6 years later and the patient continues to be observed through regular follow-up visits (Fig. 2).
For our most recent patient (Case 9, Table 8) who had lesions in multiple lung lobes, we performed a lobectomy plus segmentectomy. This patient was not diagnosed prenatally; however, CPAM was diagnosed incidentally when being evaluated for pneumonitis. At 5 years of age, the patient underwent thoracoscopic right middle lobectomy and S7 segmentectomy. During the surgery, the A7 artery was clamped, and then, ICG navigation was used and the section with reduced blood flow was resected. Although an emphysema-like area remained postoperatively, no obvious residual lesions were found and the patient continues to be observed through regular follow-up visits (Fig. 3).
Case 9: Preoperative and postoperative evaluation using computed tomography scans and ICG navigation. a A lower right lobe after excision of the right middle lobe. b ICG navigation revealed segment 7 with reduced blood flow. c Before operation. d Although an emphysema-like area remained postoperatively (in a circle), no obvious residual lesions were observed
Discussion
We perform thoracotomy on patients with unstable hemodynamics and respiratory status who cannot be maintained on anesthesia under artificial pneumothorax in the lateral decubitus position. For other cases, we perform thoracoscopic surgery not only during routine surgery but also in atypical situations such as during emergency surgery or neonatal surgery and for patients with a history of pneumonia. Thoracoscopic lobectomy is performed more frequently in children and particularly in infants, with many studies reporting its safe use regardless of the patient’s age [3, 4]. However, some studies have shown that thoracotomy and blood transfusion are needed more frequently in patients < 3 months of age, and these studies also revealed that postoperative outcomes are better in patients ≥ 12 months of age or in those that weigh ≥ 10 kg [5, 6]. Usually, we schedule surgery for patients > 4 months old, hence, in this study, our comparisons were made based on the age of 4 months. In this study, our comparison between patients < 4 months old and those aged ≥ 4 months old during surgery showed that younger patients had greater blood loss per weight than older patients; however, no patient required blood transfusion among the younger patients. The volume of blood loss appeared to be high in semi-urgent or urgent surgery cases. Frequent emergency surgery in younger patients may have influenced this outcome. There was no difference in operating time or postoperative complications between any of the patients aged < 4 months and those aged ≥ 4 months. According to the previous report, we compared the ages of patients less than 3 months and above, blood loss volumes per body weight was significantly greater in the younger patients, but no patient required a blood transfusion. There was no difference in operation time and complications between the two groups.
In our cohort, only 2 cases (3%) were converted to thoracotomy and fewer postoperative complications were observed compared to those of previous studies [4, 5, 7, 8]. Unless there are difficulties in maintaining anesthesia, we suggest that thoracoscopic surgery can be adopted for most patients. However, in the 2 cases that were converted to thoracotomies in our study, it was difficult to secure the field of view due to the distension of the affected lesions. Opting early to perform open surgery may therefore be necessary in such cases.
In this study, 2 patients required blood transfusion due to significant intraoperative blood loss. One patient underwent total pneumonectomy after conversion to thoracotomy and the other patient underwent thoracoscopic lobectomy as planned. No other complications occurred during surgery in any patient. A history of pneumonitis is predicted to make surgery more difficult due to adhesion and other factors; however, many studies have shown that a history of pneumonia does not affect the rate of postoperative complication [6, 9]. We also found no correlation between a history of pneumonitis and operating time, blood loss volumes, or postoperative complications.
For pediatric cases of CLC, there is still no consensus on the best surgical procedure for multilobar lesions. The principle of surgery for CLC is to completely remove the lesion and leave as much normal lung tissue as possible.
We began to attempt thoracoscopic-limited pulmonary resection for children, but the indications still need to be considered. It is necessary to select the surgical method according to the site and size of the lesion. In the case of multi-stage surgery in our facility (Table 8, case 2), it was difficult to decide what kind of treatment should be performed to preserve the normal lungs. Since the lesion was very large and the normal lung was compressed, we decided to perform resection multiple times while increasing the capacity of the normal lung. In the initial surgery, the cyst was removed as much as possible under thoracoscopic surgery to eliminate respiratory failure. From the second time onward, it was judged that thoracoscopic-limited pulmonary resection was difficult, and thoracotomy was performed. If lobectomy can be avoided and pulmonary resection was limited in patients with lesions involving multiple lobes, a greater quantity of healthy lung tissue can be conserved. Few studies on thoracoscopic segmentectomy in children have been undertaken; however, Bagrodia et al. reported no residual lesions and no difference in postoperative complications between lobectomy and segmentectomy procedures [10]. Fascetti-Leon et al. also reported performing segmentectomies in 54 patients, out of whom thoracoscopic surgery was attempted in 26 patients. However, the procedure in 18 patients was converted to thoracotomy, which indicates that they might have encountered difficulties during thoracoscopic segmentectomy [7]. There have also been reports of residual lesions post-segmentectomy. Future studies are needed to determine more accurate preoperative assessments, appropriate devices, and improved perioperative navigation methods to facilitate safe and accurate segmentectomies [11,12,13].
Limitations
This study had some limitations. First, there were differences between patients with CLC in terms of incomplete lobulation and body size. Second, a precise comparison of surgical outcomes was difficult due to the substantial variation in size and location of lesions, which is characteristic of this disease. Previous reports have suggested excluding extralobar sequestration when the operating procedure was clearly different. More cases of segmentectomy need to be investigated as the number of patients who underwent segmentectomy at our hospital was small.
Conclusions
Thoracoscopic surgery for CLC was performed safely in most patients, even during infancy. Semi-urgent/urgent surgery was not found to have longer operating time nor more postoperative complications. Patients < 4 months of age and patients who had undergone semi-urgent/urgent surgery tend to bleed more. Limited pulmonary resection is usually considered difficult to undertake thoracoscopically in children; however, it can be performed safely using new devices and navigation methods. We plan to continue the careful assessment of these techniques.
References
Wen CT, Liu YY, Fang HY, Hsieh MJ, Chao YK (2018) Image-guided video-assisted thoracoscopic small lung tumor resection using near-infrared marking. Surg Endosc 32:4673–4680
Sun Y, Zhang Q, Wang Z, Shao F, Yang R (2019) Is the near-infrared fluorescence imaging with intravenous indocyanine green method for identifying the intersegmental plane concordant with the modified inflation-deflation method in lung segmentectomy? Thorac Cancer 10:2013–2021
Kunisaki SM, Powelson IA, Haydar B, Bowshier BC, Jarboe MD, Mychaliska GB, Geiger JD, Hirschl RB (2014) Thoracoscopic vs open lobectomy in infants and young children with congenital lung malformations. J Am Coll Surg 218:261–270
Jelin EB, O’Hare EM, Jancelewicz T, Nasr I, Boss E, Rhee DS (2018) Optimal timing for elective resection of asymptomatic congenital pulmonary airway malformations. J Pediatr Surg 53:1001–1005
Wagenaar AE, Tashiro J, Satahoo SS, Sola JE, Neville HL, Hogan AR, Perez EA (2016) Resection of pediatric lung malformations: national trends in resource utilization & outcomes. J Pediatr Surg 51:1414–1420
Sueyoshi R, Koga H, Suzuki K, Miyano G, Okawada M, Doi T, Lane GJ, Yamataka A (2016) Surgical intervention for congenital pulmonary airway malformation (CPAM) patients with preoperative pneumonia and abscess formation: “open versus thoracoscopic lobectomy.” Pediatr Surg Int 32:347–351
Fascetti-Leon F, Gobbi D, Pavia SV, Aquino A, Ruggeri G, Gregori G, Lima M (2013) Sparing-lung surgery for the treatment of congenital lung malformations. J Pediatr Surg 48:1476–1480
Polites SF, Habermann EB, Zarroug AE, Thomsen KM, Potter DD (2016) Thoracoscopic vs open resection of congenital cystic lung disease- utilization and outcomes in 1120 children in the United States. J Pediatr Surg 51:1101–1105
Yamataka A, Koga H, Ochi T, Imashimizu K, Suzuki K, Kuwatsuru R, Lane G, Nishimura K, Inada E, Suzuki K (2017) Pulmonary lobectomy techniques in infants and children. Pediatr Surg Int 33:483–495
Bagrodia N, Cassel S, Liao J, Pitcher G, Shilyansky J (2014) Segmental resection for the treatment of congenital pulmonary malformations. J Pediatr Surg 49:905–909
Mun M, Okumura S, Nakao M, Matsuura Y, Nakagawa K (2017) Indocyanine green fluorescence-navigated thoracoscopic anatomical segmentectomy. J Vis Surg 3:80
Jin Y, Wang M, Xue L, Zhao X (2019) Clinical application of near-infrared thoracoscopy with indocyanine green in video-assisted thoracoscopic anatomical segmentectomy. Surg Innov 26:473–477
Rothenberg S (2016) Thoracoscopic lobectomy in infants and children utilizing a 5 mm stapling device. J Laparoendosc Adv Surg Tech A 26:1036–1038
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflicts of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Research involving human and/or animal participants
All procedures performed in this study were in accordance with the ethical standards of the Ethics Review Board at Nagoya University Graduate School of Medicine (Approval no. 2019-0429).
Informed consent
Written informed consent was obtained from the parents or caregivers of all patients that participated in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shirota, C., Tainaka, T., Sumida, W. et al. Thoracoscopic surgery for congenital lung cysts: an attempt to limit pulmonary resection in cases of lesions involving multiple lobes. Pediatr Surg Int 37, 213–221 (2021). https://doi.org/10.1007/s00383-020-04793-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04793-y