Abstract
Purpose
Laparoscopy is being increasingly applied to pediatric inguinal hernia repair. In younger children, however, open repair remains preferred due to concerns related to anesthesia and technical challenges. We sought to assess outcomes after laparoscopic and open inguinal hernia repair in children less than or equal to 3 years.
Methods
A prospective, single-blind, parallel group randomized controlled trial was conducted at three clinical sites. Children ≤3 years of age with reducible unilateral or bilateral inguinal hernias were randomized to laparoscopic herniorrhaphy (LH) or open herniorrhaphy (OH). The primary outcome was the number of acetaminophen doses. Secondary outcomes included operative time, complications, and parent/caregiver satisfaction scores.
Results
Forty-one patients were randomized to unilateral OH (n = 10), unilateral LH (n = 17), bilateral OH (n = 5) and bilateral LH (n = 9). Acetaminophen doses, LOS, complications, and parent/caregiver scores did not differ among groups. Laparoscopic unilateral hernia repair demonstrated shorter operative time, a consistent finding for overall laparoscopic repair in univariate (p = 0.003) and multivariate (p = 0.010) analysis. No cases of testicular atrophy were documented at 2 (SD = 2.7) years.
Conclusion
Children ≤3 years of age in our cohort safely underwent LH with similar pain scores, complications, and recurrence as OH. Parents and caregivers report high satisfaction with both techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open inguinal hernia repair (OH) remains the standard approach to pediatric inguinal hernias since its initial description over 50 years ago [1]. Advantages include a low rate of recurrence, vas deferens injury and testicular atrophy (<1%) [2–4]. Pediatric laparoscopic inguinal hernia repair (LH) has now become routinely employed in several pediatric centers. Advantages of LH as reported by retrospective studies include better cosmesis, shorter length of stay (LOS), faster recovery, and greater ability to visualize and repair a contralateral hernia [5–21]. Randomized controlled trials, while limited in the pediatric population, support these findings, [18, 19, 21] while reporting similar complication [17–19, 22] and recurrence rates [17–20]. Results differ, however, regarding postoperative pain, [17, 18, 21] particularly in younger children. As the cord structures are not manipulated during LH, this approach may be more advantageous in smaller children, in which the risks of testicular injury and trapped testicles following OH are higher [23–25]. In younger children (≤3), however, open repair remains favored because of concerns related to anesthetic risks and the technical challenges of LH. The purpose of this study was to assess post-operative pain, outcomes and safety of LH compared to OH in children ≤3 years of age.
Methods
Study design
We conducted a prospective, single-blind, parallel group randomized controlled trial comparing postoperative pain medication requirements, parent/caregiver satisfaction, safety, and outcomes after OH and LH in children ≤3 years. This study was approved by the institutional review board (IRB) at three clinical sites. Written consent was obtained from each participant’s parent/guardian prior to enrollment. Patients were enrolled by clinical investigators at participating sites. The study is registered at ClinicalTrials.gov (NCT00716768).
Children ≤3 years of age at the time of scheduled surgery with reducible unilateral or bilateral inguinal hernias were screened for inclusion in the study. Patients were excluded if there was the need for a concomitant intra-abdominal procedure, history of prior inguinal hernia repair, liver disease or contraindication to acetaminophen, midazolam, fentanyl or bupivacaine use, or expected prolonged hospitalization due to active concurrent illness. Patients were recruited and enrolled by surgical staff from the outpatient clinics of three sites. Enrollment began January 1, 2008 and follow-up concluded on December 31, 2014. Trial design remained consistent throughout the study period.
A block stratified randomization (BSR) computer program was used to randomize patients to obtain balanced comparison groups of similar size [26]. The computer program created block stratified assignments with a user selected block size. The pseudorandom number generator is a linear congruential algorithm of Park and Miller with Bays-Durham shuffling and has a period of over 2 billion. The total number of open and laparoscopic repair assignments was equally distributed in both unilateral and bilateral groups prior to randomization. Two series of envelopes were created by a registered pharmacist prior to study initiation and labeled “U” (unilateral) or “B” (bilateral), and numbered sequentially The BSR program assignments were then placed into each envelope. Patients were sequentially assigned to a unilateral or bilateral envelope based on diagnosis.
Surgical procedure
The operating room was prepared with the required equipment for both OH and LH prior to patient arrival. Children received a dose of oral acetaminophen (15 mg/kg) prior to anesthesia induction. Children >1 year of age also received one dose of midazolam (0.5 mg/kg, maximum 15 mg). Patients were induced with sevoflurane or propofol; maintenance with sevoflurane. After induction the patient’s assigned envelope was opened, determining the procedure type to be performed. LH was performed via subcutaneous endoscopically assisted ligation of the internal ring (SEAL technique) [27]. Patients found to have bilateral inguinal hernias underwent bilateral repair. In patients undergoing unilateral OH, the contralateral side was visualized by inserting a laparoscope through the ipsilateral hernia sac. Intra-operative analgesia was provided with intravenous boluses of fentanyl of 0.5–1 µg/kg as clinically indicated. At procedure conclusion all patients received peripheral nerve blockade and wound infiltration with 0.25% bupivacaine. Patients were at no increased risk of harm as both open and laparoscopic inguinal hernia repair and the medications used for pain control are accepted therapies.
Postoperative care
Families and staff caring for patients were not informed of which procedure was performed. Operative wound dressings were applied at both open and laparoscopic sites regardless of procedure performed and remained in place throughout the hospital stay to ensure integrity of the blinding process. The Face, Legs, Activity, Cry, Consolability scale (FLACC) was used to record pain scores on an hourly basis for the first 6 h and then every 6 h thereafter. Patients were given oral acetaminophen (15 mg/kg) for FLACC scores >4, with intravenous fentanyl (0.5 mcg/kg/dose) for persistent/breakthrough pain. Term infants <48 weeks post-conceptual age, preterm infants <52 weeks post-conceptual age, or preterm infants <60 weeks post-conceptual age with comorbidities (e.g. anemia, cardiopulmonary disease) were admitted for overnight observation. Patients were discharged when pain was deemed adequately controlled with oral acetaminophen.
Outpatient data recording and caregiver surveys
Written discharge instructions for postoperative care and acetaminophen dosing were provided. Parents were instructed to give acetaminophen 15 mg/kg every 4 h as needed for FLACC scores >4. Parents were asked to record the number of days before the patient returned to full activity. A questionnaire was provided to record satisfaction and cosmetic appearance ("Appendix").
Outcomes
The primary outcome was the total number of doses of acetaminophen administered. Secondary short-term outcomes included operative time, incidence of intra-operative complications, conversion rate, requirement for re-operation, wound infection, hydrocele, and length of hospital stay. Long-term outcomes included hernia recurrence and testicular atrophy. All data was stored on a password protected server secured by the study team. Patient follow-up occurred via routine postoperative outpatient visits, telephone evaluation at a minimum of three and 12 months, and electronic medical record chart review. Patients lost to long-term follow-up whose parents/caregivers returned the post-operative surveys at 7 days were considered to have a follow-up time of 7 days for statistical analysis.
Statistical analysis
Target sample size was calculated based upon the estimated mean difference in the number of acetaminophen doses based upon previously published data [18]. Utilizing the two sample t test with a two-sided alpha of 0.05 and power of 80%, we calculated the need to recruit 38 children with unilateral hernias for the open repair group and 38 children with unilateral hernias for the laparoscopic repair group to statistically detect a difference of 0.70 doses/group.
The total number of postoperative acetaminophen doses, fentanyl doses, operative time, length of stay, and days before full activity were analyzed via a two-sided t test. Categorical variables were compared using Fisher’s exact test. Univariate and multivariate models were developed to determine the association of postoperative acetaminophen doses and operative time with pre-operative demographics, risk factors, and procedure specifics. Laterality, procedure type, gender, race, age, weight, and American Society of Anesthesiologists (ASA) class were included as independent variables. These variables were categorized where appropriate to fit the model.
A logistic regression model was performed using the Firth approach with robust variance estimators for binary outcome variables. For continuous outcome variables, linear regression with robust estimation was performed due to influential observations. If the normality assumption was not met by the outcome variable, then log-transformation was performed. Acetaminophen dosing was controlled for using the number of fentanyl doses. This correction was applied because in some cases, patients received fentanyl in lieu of acetaminophen, thus the total number of fentanyl doses was included in univariate and multivariate analyses to control for the confounding impact of fentanyl dosing on the number of acetaminophen doses received while inpatient. For statistical analyses, a p value of <0.05 was considered significant. Analyses were performed in Stata 13.0 (Stata Corporation, College Station. TX, USA).
Results
Study population
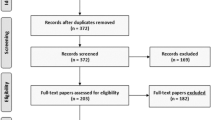
One hundred and thirty-six patients were screened for inclusion in the study. After exclusion criteria were applied and patient enrollment was stopped, 41 patients were included for analysis. Twenty-six patients were randomized to laparoscopic repair (n = 23 unilateral; n = 3 bilateral) and 15 to open repair (n = 14 unilateral, n = 1 bilateral). Intra-operatively, a patent processus vaginalis was found in four cases allocated to unilateral OH and in six cases allocated to unilateral LH, resulting in a postoperative group breakdown of unilateral OH (n = 10), unilateral LH (n = 17), bilateral OH (n = 5) and bilateral LH (n = 9) (Fig. 1). Baseline demographic data is provided in Table 1. Age, weight, sex, and race were available for all patients. ASA classification and GA at birth were available in 36/41 (87.8%) of patients.
Primary outcome
Complete pain medication data was provided by caregivers of 31/41 patients (75.6%). Patients with incomplete pain medication dosing were excluded from this portion of the analysis. The total number of postoperative acetaminophen doses did not differ among groups. Similarly, the number of patients requiring fentanyl and total fentanyl doses did not differ between groups (Table 2). Gender, race, age, weight, ASA class, laterality, type of operation, and number of fentanyl doses did not affect the number of acetaminophen doses received in either univariate or multivariate analysis (Table 3).
Secondary outcomes
Operative time was significantly shorter in those who underwent unilateral LH when compared with OH (27.9 (SD = 15) versus 53.2 (SD = 30.4) min; p = 0.007). Additionally, operative time was significantly shorter when laparoscopy was employed in univariate (p = 0.003), and multivariate analysis (p = 0.010), with 0.4 and 0.5 less hours required, respectively (Table 4). Length of stay was not significantly different between groups (Table 2).
Surveys were returned in 31/41 patients (75.6%). Forty percent of patients whose caregivers did not return the survey were contacted via telephone for over-the-phone survey completion, resulting in a 35/41 (85.4%) overall completion rate. Days to return to full activity were similar among groups (Table 2). Parents expressed high satisfaction with both types of hernia repair, with most reporting scores of 4 or 5, and no ratings of 1 or 2. These findings were not different between groups (Table 2).
There were no intraoperative complications and three postoperative complications (7.3%). One unilateral LH patient had minor bleeding at the incision site, one bilateral OH developed a wound infection requiring oral antibiotics, and one bilateral LH had a recurrence with incarceration, requiring urgent OH.
Follow-up
Three patients were lost to follow-up. These patients were excluded from both postoperative pain medication analyses and parent/caregiver satisfaction survey results, but were included in intraoperative analyses. Sixteen families were reached via telephone for long-term follow-up, resulting in a mean follow-up time of 2 (SD = 2.7) years.
Discussion
This study represents the first blinded, randomized controlled trial comparing OH and LH of unilateral and bilateral inguinal hernias in children ≤3 years of age. In this study, we found a significantly shorter operative time among patients undergoing unilateral LH, with similar postoperative acetaminophen doses required, postoperative LOS, incidence of postoperative complications, and parent and/or caregiver satisfaction scores regarding recovery and wound appearance.
We found no significant difference in the number of postoperative acetaminophen doses received among children undergoing open and laparoscopic repair of both unilateral and bilateral inguinal hernias utilizing the FLACC pain assessment tool. These findings persisted in both univariate and multivariate analysis when adjusting for the number of fentanyl doses received. These results are similar to those seen in prior prospective, retrospective, and RCT studies [8, 11, 18, 21, 28]. Although Koivusalo et al. found that patients undergoing unilateral IH repair required more rescue analgesia (p < 0.05), the authors noted similar intra-operative fentanyl doses, discharge pain scores and outpatient ibuprofen doses among groups [17]. These results suggest that LH confers no increased pain or discomfort.
Wound appearance and time to return to full activity represent additional parent and/or caregiver concerns. Comparative studies and RCTs note higher wound appearance scores and a lower incidence of “ugly scar(s)” after LH [8, 11, 18, 19, 21]. Time for return to normal activity varies within the literature [17, 18]. We report a similar number of days to full activity after unilateral open and laparoscopic repair at 3.3 and 2.5 days, respectively, and bilateral open and laparoscopic repair at 4.3 and 3.7 days. These results and those of the literature support equivalent or greater wound cosmesis and similar days until return to full activity after laparoscopic repair.
In this study, unilateral LH resulted in shorter operative times than unilateral OH, a consistent finding for overall laparoscopic repair in univariate (p = 0.003) and multivariate (p = 0.010) analysis. These results are similar to those reported by other investigators, in which mean operative times range from 8.7 to 58.66 min for unilateral LH and 12–57.08 min for bilateral LH [8, 13, 17–19, 21, 29–31]. Randomized controlled trials differ, with early reports noting similar [18] or even increased operative time with laparoscopic repair, [17] while more recent studies report equivalent or shorter operative times [19, 21, 31]. These results suggest that laparoscopy itself is not the sole determinant of shorter operative time, but more likely the specific technique of repair and surgeon experience with the particular approach.
During the early experience with pediatric LH, recurrence was a significant concern. Recurrence rates after OH repair typically range from 0 to 5% [8, 13, 19, 32]. LH must offer a similarly low recurrence rate as OH prior to consideration as an equivalent treatment modality. Studies focusing on LH report recurrence rates of 0–4.4%, [17, 18, 21, 29, 33, 34] while those directly comparing recurrence among patients undergoing OH and LH report similar rates between groups [17, 18, 21]. In this study, we report a 0% recurrence rate in the OH group and a 3.8% recurrence rate in the LH group with a mean follow-up of 2 years. It is important that published recurrence rates be considered in the context of length of time for follow-up, as historically only 50% recur within 6 months, with 76% recurring in 2 years and 96% within 5 years [35, 36].
Complications after LH are relatively infrequent, with descriptive studies reporting rates from 0 to 6.4% [7, 14, 16, 24, 28–31, 33, 37, 38]. The most common complications are related to hydrocele development, [16, 30, 31, 34, 39, 40] high testes, [24] wound infection, [16, 40] stitch sinus or granuloma, [16, 40] and, rarely, testicular atrophy [39] or retroperitoneal hematoma [40]. Prospective and retrospective studies report complication rates of 0.6–8.8% after OH and 0–3.9% after LH, with no differences reported among groups [8, 10, 11, 13]. RCTs support these results, reporting low overall complication rates, and the majority reporting no difference among groups [17–19, 21]. In this study, we note a complication rate of 6.67% after OH and 7.7% after LH, with a major complication rate of 0 and 3.8%, respectively. Importantly, all complications occurred during the first year of the study, with no complications, neither major nor minor, seen during subsequent years.
This studay has several limitations, foremost being the small sample size, which may not have allowed adequate power to demonstrate all potential differences or capture rare complications. Patient enrollment was halted due to a combination of low enrollment rates, likely due to inclusion criteria and institutional case mix. Interim analysis at that time suggested non-inferiority of laparoscopic repair to open repair. Importantly, in this study, the operative time associated with open repair was longer than reported in prior studies, most likely due to the use of transinguinal laparoscopy and because this study was conducted at teaching institutions, which may have contributed to our finding that operative time was shorter for laparoscopic repair. Additionally, the small sample size in this study may not provide enough power to detect differences in the rate of post-operative complications, which are infrequent events after pediatric inguinal hernia repair. Nonetheless, our overall findings support similar results after laparoscopic and open inguinal hernia repair, a finding not previously reported in this age group. Additionally, although the randomization process is designed to control for potential confounders, the operative surgeon was not randomized, thus creating potential bias as surgeon experience likely has an impact on many aspects of LH including operative time and recurrence rates. Additionally, the decision to administer acetaminophen is affected by prior fentanyl dosing. Although the number of fentanyl doses was controlled for in univariate and multivariate analysis, we cannot know the full impact of fentanyl dosing on subsequent FLACC scoring and acetaminophen dosing decisions on a per patient basis, as each individual’s response to opiate administration may vary.
Conclusion
This randomized controlled trial compared OH and LH of unilateral and bilateral inguinal hernias in children <3 years of age. Our study found that LH demonstrated potentially shorter operative times than OH, with similar pain mediation requirements, length of stay, and incidence of postoperative complications between groups. Parents/caregivers report similar days until return to full activity, satisfaction with recovery time, and satisfaction with wound appearance. OH and LH thus both appear to be equally safe and effective.
References
Gross RE (1953) Surgery of Infancy and Childhood. Saunders
Grosfeld JL (2006) Pediatric surgery, 6th edn. Mosby/Elsevier, Philadelphia
DuBois JJJ (1997) Transinguinal laparoscopic examination of the contralateral groin in pediatric herniorrhaphy. Surg Laparosc Endosc 7:384–387
Grossmann PAW (1995) The efficacy of laparoscopic examination of the internal inguinal ring in children. J Pediatr Surg 30:214–218. doi:10.1016/0022-3468(95)90562-6
Pellegrin K, Bensard DD, Karrer FM, Meagher DP (1996) Laparoscopic evaluation of contralateral patent processus vaginalis in children. Am J Surg 172:602–606. doi:10.1016/S0002-9610(96)00242-5
Miltenburg D, Nuchtern J, Jaksic T et al (1998) Laparoscopic evaluation of the pediatric inguinal hernia—a meta-analysis. J Pediatr Surg 33:874–879. doi:10.1016/S0022-3468(98)90664-9
Gorsler CM, Schier F (2003) Laparoscopic herniorrhaphy in children. Surg Endosc Other Interv Tech 17:571–573. doi:10.1007/s00464-002-8947-y
Saranga Bharathi R, Arora M, Baskaran V (2008) Pediatric inguinal hernia: laparoscopic versus open surgery. JSLS 12:277–281
Tsai YC, Wu CC, Yang SSD (2007) Minilaparoscopic herniorrhaphy with hernia sac transection in children and young adults: a preliminary report. Surg Endosc Other Interv Tech 21:1623–1625. doi:10.1007/s00464-007-9207-y
Endo M, Watanabe T, Nakano M et al (2009) Laparoscopic completely extraperitoneal repair of inguinal hernia in children: a single-institute experience with 1257 repairs compared with cut-down herniorrhaphy. Surg Endosc Other Interv Tech 23:1706–1712. doi:10.1007/s00464-008-0300-7
Tsai YC, Wu CC, Yang SSD (2010) Open versus minilaparoscopic herniorrhaphy for children: a prospective comparative trial with midterm follow-up evaluation. Surg Endosc Other Interv Tech 24:21–24. doi:10.1007/s00464-009-0645-6
Ho CH, Yang SS, Tsai YC (2010) Minilaparoscopic high-ligation with the processus vaginalis undissected and left in situ is a safe, effective, and durable treatment for pediatric hydrocele. Urology 76:134–137
Niyogi A, Tahim AS, Sherwood WJ et al (2010) A comparative study examining open inguinal herniotomy with and without hernioscopy to laparoscopic inguinal hernia repair in a pediatric population. Pediatr Surg Int 26:387–392
Turial S, Enders J, Krause K, Schier F (2010) Laparoscopic inguinal herniorrhaphy in premature infants. Eur J Pediatr Surg 20:371–374. doi:10.1055/s-0030-1261932
Esposito C, Turial S, Alicchio F et al (2013) Laparoscopic repair of incarcerated inguinal hernia. A safe and effective procedure to adopt in children. Hernia 17:235–239. doi:10.1007/s10029-012-0948-8
McClain L, Streck C, Lesher A et al (2015) Laparoscopic needle-assisted inguinal hernia repair in 495 children. Surg Endosc Other Interv Tech 29:781–786. doi:10.1007/s00464-014-3739-8
Koivusalo AI, Korpela R, Wirtavuori K et al (2009) A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 123:332–337. doi:10.1542/peds.2007-3752
Chan KL, Hui WC, Tam PKH (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19:927–932. doi:10.1007/s00464-004-8224-3
Shalaby R, Ibrahem R, Shahin M et al (2012) Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg 2012:484135. doi:10.1155/2012/484135
Feng S, Zhao L, Liao Z, Chen X (2015) Open versus laparoscopic inguinal herniotomy in children: a systematic review and meta-analysis focusing on postoperative complications. Surg Laparosc Endosc Percutaneous Tech 25:275–280. doi:10.1097/SLE.0000000000000161
Celebi S, Uysal A, Inal F, Yildiz A (2014) A single-blinded, randomized comparison of laparoscopic versus open bilateral hernia repair in boys. J Laparoendosc Adv Surg Tech 24(2):117–121
Rogers DA, Hatley RM, Howell CGJ (1998) A prospective, randomized comparison of traditional and laparoscopic inguinal exploration in children. Am Surg 64:119–121
Pastore V, Bartoli F (2014) Neonatal laparoscopic inguinal hernia repair: a 3-year experience. Hernia 19:611–615. doi:10.1007/s10029-014-1269-x
Turial S, Enders J, Krause K, Schier F (2011) Laparoscopic inguinal herniorrhaphy in babies weighing 5 kg or less. Surg Endosc Other Interv Tech 25:72–78. doi:10.1007/s00464-010-1132-9
Esposito C, Turial S, Escolino M et al (2012) Laparoscopic inguinal hernia repair in premature babies weighing 3 kg or less. Pediatr Surg Int 28:989–992. doi:10.1007/s00383-012-3156-9
(1992) Numerical recipes in C
Harrison MR, Lee H, Albanese CT, Farmer DL (2005) Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: a novel technique. J Pediatr Surg 40:1177–1180
Kozlov Y, Novozhilov V (2015) Technology of single-incision laparoscopic surgery in treatment of inguinal hernia in small babies. J Laparoendosc Adv Surg Tech A 25:526–530. doi:10.1089/lap.2014.0206
Shalaby R, Ismail M, Samaha A et al (2014) Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg 49:460–464. doi:10.1016/j.jpedsurg.2013.10.019
Montupet P, Esposito C (2011) Fifteen years experience in laparoscopic inguinal hernia repair in pediatric patients. Results and considerations on a debated procedure. Surg Endosc Other Interv Tech 25:450–453. doi:10.1007/s00464-010-1188-6
Shalaby R, Ismail M, Dorgham A et al (2010) Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg 45:2210–2216. doi:10.1016/j.jpedsurg.2010.07.004
Esposito C, Giurin I, Alicchio F et al (2012) Unilateral inguinal hernia: laparoscopic or inguinal approach. Decision making strategy: a prospective study. Eur J Pediatr 171:989–991. doi:10.1007/s00431-012-1698-4
Montupet P, Esposito C (1999) Laparoscopic treatment of congenital inguinal hernia in children. J Pediatr Surg 34:420–423. doi:10.1016/j.arcped.2007.03.035
Lee DY, Baik YH, Kwak BS et al (2015) A purse-string suture at the level of internal inguinal ring, taking only the peritoneum leaving the distal sac: is it enough for inguinal hernia in pediatric patients? Hernia 19(4):607–610
Abraham MK, Nasir AA, Puzhankara R et al (2012) Laparoscopic inguinal hernia repair in children: a single-centre experience over 7 years. Afr J Paediatr Surg AJPS 9:137–139. doi:10.4103/0189-6725.99400
Grosfeld JL, Minnick K, Shedd F et al (1991) Inguinal hernia in children: factors affecting recurrence in 62 cases. J Pediatr Surg 26:283–287. doi:10.1016/0022-3468(91)90503-L
Tsai YC, Wu CC, Ho CH et al (2011) Minilaparoscopic herniorrhaphy in pediatric inguinal hernia: a durable alternative treatment to standard herniotomy. J Pediatr Surg 46:708–712. doi:10.1016/j.jpedsurg.2010.09.004
Schier F, Montupet P, Esposito C (2002) Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 37(3):395–397
Schier F (2006) Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg 41:1081–1084. doi:10.1016/j.jpedsurg.2006.02.028
Ozgediz D, Roayaie K, Lee H et al (2007) Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: report of a new technique and early results. Surg Endosc Other Interv Tech 21:1327–1331. doi:10.1007/s00464-007-9202-3
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix


Rights and permissions
About this article
Cite this article
Gause, C.D., Casamassima, M.G.S., Yang, J. et al. Laparoscopic versus open inguinal hernia repair in children ≤3: a randomized controlled trial. Pediatr Surg Int 33, 367–376 (2017). https://doi.org/10.1007/s00383-016-4029-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-4029-4