Abstract
Purpose
Pain is one of the indications to treat varicocele at any age. The purpose of this study is to find a possible correlation between pain and objective testicular damage through the analysis of hormonal values.
Methods
Between 1990 and 2001, varicocelectomy was performed on 44 adolescents with painful varicocele using two different techniques. Thirty-eight patients were eligible for the study. Pre- and post-operative hormonal values were analyzed retrospectively to find a possible correlation between pain and testicular damage or discomfort. The patients had to fill out a simple questionnaire about their type of pain following a two-grade rating scale. After treatment, relief of pain or persistence of symptoms were recorded.
Results
Six months after surgery 26 patients showed complete relief of pain. There was not a statistically significant correlation between grade of varicocele, type of surgery and relief of symptoms. Clinically there was not a statistically significant correlation between pain and hormonal values.
Conclusions
Management of painful varicocele in pediatric patients should be studied through randomized trials comparing conservative and surgical treatments. While waiting for objective data supporting surgery, clinical evidence justifies varicocelectomy which, on the other hand, is not supported by objective clinical data (i.e., hormonal values).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic varicocele is the most commonly diagnosed peripubertal andrologic disease and the most commonly treatable cause of male-related impaired fertility potential [1].
It is now accepted that the treatment of varicocele in children should be concomitant with the onset of ipsilateral testicular hypotrophy (or testicular growth arrest) and when varicocele is accompanied by pain. Obviously, changes in semen quality are not considered as a parameter for surgery in pediatric patients, while they remain the first indication for surgery in adult patients or as soon as patients are old enough to perform semen analysis [2].
However, the need to treat varicocele in pediatric patients without testicular hypotrophy but with painful varicocele is still doubtful; while testicular hypotrophy and changes in semen quality are objective elements obtained measuring the diameters and the volume of the testis (for testicular hypotrophy) and through a comparison with WHO criteria for normal semen analysis (for changes in semen quality), pain is still considered a subjective evidence, even though formalized in validated questionnaires. Clinicians or surgeons know that it is not possible to assess pain with absolute certainty, especially in pediatric age. Also, this problem often affects patient randomization, reproducibility of the data obtained as well as treatment options; to treat or not to treat painful varicocele?
Patients often perceive or interpret pain differently depending on the situation; many patients report acute pain after sport practice (bike, football, etc.), professional activities or after school.
Recently it has been noticed that literature reports different studies, although limited in number, showing relief of pain after varicocelectomy; none of these studies, however, could explain how varicocele may cause pain or why varicocelectomy should relieve patients from pain [3–6].
Through a retrospective study on patients treated for painful varicocele, this study tries to find out whether pain may be somehow related to objective data and then whether a possible relief of pain may be based on objective parameters.
Materials and methods
The Authors established the inclusion criteria for this study after considering the inclusion criteria used in the most important studies on this topic reported in literature. Varicocele was classified as follows: grade I, palpable varicocele only with Valsalva; grade II, palpable varicocele without Valsalva; grade III, visible varicocele.
The inclusion criteria for this study were the following: age between 14 and 16 years, grade II or III left varicocele, no testicular hypotrophy at US and orchidometer measurements, no previous infections of the urinary system, no previous testicular traumas or previous inguinal and scrotal surgeries, no neurological or metabolic diseases, pain already treated conservatively for at least 2 months.
Between 1990 and 2001 all patients that visited our Department for varicocele underwent objective examination, Doppler velocimetry as well as blood tests before and after treatment to assess the testosterone hormone profile at baseline, FSH and LH. In this study, the Authors considered only patients surgically treated for scrotal or testicular pain associated with varicocele in the period previously indicated. From 2001 to present, hormonal tests have been performed only when clinically indicated (i.e., micropenis, small testes for age, endocrine pathology).
Patients could define their pain as: (1) a continuous pain sometimes treated with analgesics; (2) a sense of obstruction/discomfort.
Evaluation criteria
After recruiting patients retrospectively, the Authors considered only the patients who had completed the post-operative follow-up (3, 6 and 12 months after surgery), undergone blood tests and filled out the questionnaire both before surgery and 6 months after surgery.
All patients with complete regression of pain were considered as responders; otherwise they were referred to as non-responders.
Hormonal assessment (FSH, range 1–14 U/L; LH, range 2–10 U/L; TT μmol/L) was used as an objective counterproof of a possible correlation between varicocele—testicular damage—pain. All patients without testicular hypotrophy and pain who underwent surgery in that same period were considered as the control group for hormonal values.
Statistical analysis was performed using the student t test, Chi-square and Fischer exact tests. Significance value was set at P < 0.05. The analysis was conducted with the Statistical Package for Social Sciences (SPSS) software version 15 for Windows SPSS Inc, Chicago, USA.
Results
Between 1990 and 2001, varicocelectomy was performed on 398 patients. Of these patients, 102 underwent hormonal tests and 44 (11%) surgery for scrotal or testicular pain associated with varicocele. Only 38 patients aged between 14 and 16 years were eligible for the study.
Twenty-nine patients had grade III varicocele while nine had grade II varicocele; 24 (20 grade III and 4 grade II) underwent microsurgical varicocelectomy with vein by-pass and artery sparing while 14 (9 grade III and 5 grade II) underwent videolaparoscopic varicocelectomy without artery sparing.
Surgical complications were two hydroceles in the microsurgery group; no complications were reported in the laparoscopy group. After 1 year no patient developed hypotrophy.
Twenty-six (68%) patients stated to have a type 1 pain; 12 patients (32%) stated a type 2 pain. Six months after treatment, pain had resolved in 22 patients from the former group and in four patients from the latter group. Four patients from the type-1 group felt less pain but a constant scrotal discomfort, while eight patients from the type-2 group felt no changes. There was a statistically significant correlation between pre- and post-treatment pain reduction (P < 0.05).
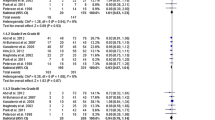
Hormonal evaluation (Table 1)
Data analysis did not show statistically significant differences between pre- and post-operative condition (P > 0.05) for both FSH and LH. This was confirmed by comparing the data regarding these patients with the values from subjects without pain (control group) and treated surgically (data not included in the study). This suggested that there was not an organic (hormonal) basis that could justify a potential testicular damage.
As for testosterone, there was a statistically significant difference between pre- and post-treatment values, with an increased post-operative TT value in all patients. This could represent a possible bias due either to the physiological growth of subjects or surgery. However, also for testosterone there were not statistically significant pre- and post-operative differences between these patients and the patients without pain (P > 0.05).
It was not possible to notice any correlation between varicocele grade and type of pain, or between relief of pain and varicocele grade. This means that the surgical approach (microsurgery vs. laparoscopic varicocelectomy or artery sparing vs. complete ligation) could not accurately predict outcomes of relief of symptoms.
Discussion
Although over the years many authors have studied varicocele to identify common elements in patients affected by this condition, it is not yet clear whether varicocele is to be treated in pediatric patients, which patients need surgery, which correlation may exist between varicocele, pain, grade and testicular hypotrophy and which subjects are more likely to develop testicular hypotrophy [7–9].
Studies explaining the correlation between varicocele and pain with an objective perspective are not currently available in literature. Only few studies reported in literature consider the efficacy of varicocele ligation in the treatment of scrotal pain, but none of these focuses on the nature of this pain or its pathogenesis [6], [10–12].
Many Authors have suggested a conservative treatment of pain, including scrotal support, nonsteroidal anti-inflammatory medications, decreased physical activity, etc.…, apparently with poor results [9, 10].
The Authors of this study believe that pain origin and cause are difficult to establish, although clinical evidence supports the surgical treatment of varicocele. Different studies showed that surgery proved successful in 68–88% of patients in terms of post-operative relief of pain. Yet, the patient population of these studies was very varied, with different median ages, age ranges, varicocele grades and, above all, different categorizations of pain rating: many have defined the pain of patients affected by varicocele as a dull, throbbing, sharp or pulling sensation, either requiring analgesics or not.
Varicocele damages the affected testis as it is proved by the onset of testicular hypotrophy which, on the other hand, does not affect all patients. It surely affects and damages spermatogenesis, as shown by semen analysis but, again, this is not true for all patients; varicocele causes pain, but only 2–10% of the affected patients report this symptom. Also, studies reporting or proving a possible correlation between pain and testicular hypotrophy, a sign of testicular damage, are not currently available. So how is it possible to explain a post-operative relief of pain? Is it related to the successful treatment of varicocele or to the surgical denervation of the area? On this topic, a recent study by Strom et al. [13] reported their experience with chronic orchialgia unrelated to varicocele successfully treated with microsurgical denervation. Should this approach be applied also to varicocele-related pain?
When surgeons decide to treat varicocele, they give scientifically sound reasons to the parents, but they also have to explain that surgical treatment may not bring the expected benefit, i.e., fertility. Surgeons should behave likewise when dealing with pain. In literature, different studies have shown either the efficacy or uselessness of the treatment with respect to the outcomes, i.e., fertility and pregnancy rate, following scientifically justified randomized studies. The same scientific approach should be used for the treatment of pain [14–16].
This study does not show the origin or the cause of pain, which is ultimately a subjective symptom; its aim is to show that pain is not clinically correlated to a gonadal deficit. There is clinical evidence that relief of pain is strictly correlated to the treatment of varicocele in the majority of cases. For this reason, varicocele should be surgically treated until more certain information on the origin of this pain is available or further randomized studies involving pharmacologic treatment are carried out to support a conservative treatment of varicocele instead of surgery.
References
Karademir K, Senkul T, Baykal K, Ates F, Iseri C, Erden D (2005) Evaluation of the role of varicocelectomy including external spermatic vein ligation in patients with scrotal pain. Int J Urol 12:484–488. doi:10.1111/j.1442-2042.2005.01063.x
Zampieri N, Zuin V, Corroppolo M, Chironi C, Cervellione RM, Camoglio FS (2007) Varicocele and adolescents: semen quality after 2 different laparoscopic procedure. J Androl 28:727–733. doi:10.2164/jandrol.107.002600
Peterson AC, Lance RS, Ruiz HE (1998) Outcomes of varicocele ligation done for pain. J Urol 159:1565–1567. doi:10.1097/00005392-199805000-00043
Yeniyol CO, Tuna A, Yener H, Zeyrek N, Tilki A (2003) High ligation to treat pain in varicocele. Int Urol Nephrol 35:65–68. doi:10.1023/A:1025972601213
Maghraby HA (2002) Laparoscopic varicocelectomy for painful varicoceles: merits and outcomes. J Endourol 16:107–110. doi:10.1089/089277902753619627
Yaman O, Ozdiler E, Anafarta K, Gogus O (2000) Effect of microsurgical subinguinal varicocele ligation to treat pain. Urology 55:107–108. doi:10.1016/S0090-4295(99)00374-X
Nielsen ME, Zderic S, Freedland SJ, Jarow JP (2006) Insight on pathogenesis of varicoceles: relationship of varicocele and body mass index. Urology 68(2):392–396. doi:10.1016/j.urology.2006.02.005
Prabakaran S, Kumanov P, Tomova A, Hubaveshki S, Agarwal A (2006) Adolescent varicocele: association with somatometric parameters. Urol Int 77(2):114–117. doi:10.1159/000093902
Zampieri N, Zuin V, Corroppolo M, Ottolenghi A, Camoglio FS (2008) Relationship between varicocele grade, vein reflux and testicular growth arrest. Pediatr Surg Int 24:727–730. doi:10.1007/s00383-008-2143-7
Al-Buheissi SZ, Patel HR, Wazait HD, Miller RA, Nathan S (2007) Predictors of success in surgical ligation of painful varicocele. Urol Int 79:33–36. doi:10.1159/000102910
Chawla A, Kulkarni G, Kamal K, Zini A (2005) Microsurgical varicocelectomy for recurrent or persistent varicoceles associated with orchialgia. Urology 66:1072–1074. doi:10.1016/j.urology.2005.05.052
Levine LA, Matkov TG, Lubenow TR (1996) Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchalgia. J Urol 155:1005–1007. doi:10.1016/S0022-5347(01)66369-9
Strom KH, Levine LA (2008) Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol 180(3):949–953. doi:10.1016/j.juro.2008.05.018
Sigman M, Jarow JP (1997) Ipsilateral testicular hypotrophy is associated with decreased sperm counts in infertile men with varicoceles. J Urol 158:605–607. doi:10.1016/S0022-5347(01)64567-1
Evers JL, Collins JA (2003) Assessment of efficacy of varicocele repair for male subfertility: a systemic review. Lancet 361:1849–1852. doi:10.1016/S0140-6736(03)13503-9
Diamond DA, Zurakowski D, Bauer SB, Borer JG, Peters CA, Cilento BG Jr et al (2007) Relationship of varicocele grade and testicular hypotrophy to semen parameters in adolescents. J Urol 178:1584–1588. doi:10.1016/j.juro.2007.03.169
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zampieri, N., Ottolenghi, A. & Camoglio, F.S. Painful varicocele in pediatric age: is there a correlation between pain, testicular damage and hormonal values to justify surgery?. Pediatr Surg Int 24, 1235–1238 (2008). https://doi.org/10.1007/s00383-008-2252-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2252-3