Abstract
In a retrospective study, intraoperative photos and video documentations of 884 children demonstrate that inguinal hernias and their recurrences are aspects of a full spectrum, which ranges from fully closed internal inguinal rings (IIR) and small openings to all-the way-down-into-the-scrotum open processus; 92% of the children had indirect and 2% direct hernias, 4% had no open IIR, 1% was femoral, 2% were hernias en pantalon and 1% combinations of indirect, direct and femoral hernias; 3% were recurrences. Among the 28 children with recurrences, the IIR was fully open in only 36%, partially open in 25%, had only a small opening in 21% and even a closed IIR in 18%. The present paper demonstrates that the yes/no concept of inguinal hernia needs to be redefined. Hernias and their recurrences constitute a spectrum. There are hernias and recurrences without a laparoscopically visible open IIR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Hernia” in Greek means swelling or budding. In patients with a groin swelling from prolapsed bowel, a “herniotomy” is suggested and performed.
In laparoscopy one would expect an open internal inguinal ring (IIR) in all cases of an indirect inguinal hernia, or in a recurrence, respectively. Irritatingly however, this is not always the case [1]. Open IIRs may be found in patients who never had an inguinal hernia. More so, in children with an inguinal hernia, an even bigger IIR might be found during laparoscopy on the contralateral side, although a hernia was never seen there. Evidently, an open IIR is not equivalent to a hernia, and an IIR’s physical shape is not directly correlated with a hernia.
Conversely, despite a hernia being diagnosed clinically, no open IIR is found laparoscopically in approximately 4% of patients. This “hernia” will persist after surgery, lead to parents’/patients’ disappointments and may even lead to lawsuits. Obviously, there are hernias without open IIRs.
If a swelling recurs or persists postoperatively, it is called a recurrence.
Recurrences raise similar questions. There are clinical recurrences in which no opening is found during re-laparoscopy. And, there are recurrences with an only small 1- or 2-mm-diameter opening, too small for a prolapse of intra-abdominal contents.
Both, hernias and recurrences thus seem not to be limited to the presence of an open IIR, and their laparoscopic picture appears to encompass a full spectrum. The dilemma is known from adult hernia surgery [2–7]. With increasing numbers of inguinal hernias being treated laparoscopically in children, and with ongoing controversy about different recurrence rates in “open” versus laparoscopic techniques, the clinical role of the laparoscopic spectrum of inguinal hernias and their recurrences is discussed.
Materials and methods
A series of 884 patients, operated on laparoscopically for the diagnosis of either inguinal hernia or recurrence of inguinal hernia (667 boys, 214 girls; median age 1.6 years, range 1 week–14 years), the videorecordings and photorecordings of all IIRs were evaluated retrospectively. All procedures had been videorecorded or photodocumented. The videos were reviewed by the author. Clinical followup studies were performed by senior physicians of the author’s department. Parents would return for a clinical evaluation 4–6 weeks postoperatively and one year later. The last 100 patients in the series were contacted at home by telephone by a senior physician. The study includes only IIRs which were diagnosed preoperatively with displaying a hernia. IIRs which were found unexpectedly open intraoperatively (at the contralateral side), without any previous history of a hernia, were excluded. They were suture-closed but not part of this study.
Preoperatively, nearly all patients were diagnosed with having indirect hernias, only three children were preoperatively suspected of possibly having a direct hernia (0.3%). In none a femoral hernia or a combination of several hernia types was suspected preoperatively. Intraoperatively, the configuration of the IIR ranged from fully open (Fig. 1) to completely closed (Fig. 2). In case of a doubtful configuration, the internal ring was fully exposed using a forceps in order to evaluate the depth of the processus.
Only those IIRs were included where previously an evident clinical hernia had been diagnosed. Open IIRs found unexpectedly during an unrelated procedure were excluded, also unexpected open contralateral IIRs.
Among the 884 children were 27 who had previously been operated upon laparoscopically because of an inguinal hernia (3%). Among the recurrences were two children with a second recurrence (0.2%). Thus, a total of 29 of the children underwent laparoscopy for a recurrent hernia. In no case did a “recurrence” occur in an IIR, which was found open unexpectedly (contralaterally, without a previous hernia) and had been closed routinely with a suture.
In 31 children the hernia was metachronous. The majority of them, 30, had occurred after an open hernia repair, only one after a previous laparoscopic repair. The metachronous hernias were noticed between 14 days and 7 years after surgery for the first hernia (median 2.2 years). Again, recurrences refer only to those previously closed IIRs, which had presented before with a clinical hernia. IIRs closed when found incidentally (without previous hernia) were excluded.
Up to case number 558, any open IIR wider than 2 mm was suture-closed. In all subsequent children any open IIR was closed, irrespective of the diameter. The technique of suture closure of the IIR was described earlier [8]. Essentially, the opening was suture-closed with an N-shaped nonabsorbable suture.
Children with isolated femoral hernias were excluded.
Results
On the side of a clinically diagnosed inguinal hernia, the following spectrum of IIRs was found: no opening (Fig. 2), an open processus of only few mm depth (Fig. 3), an open processus of several mm depth (Fig. 4), an open processus of more than 1 cm length (= inguinal hernia, Fig. 1) and a processus reaching all the way down into the scrotum (= scrotal hernia, Fig. 5).
Statistically the findings were:

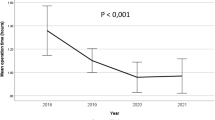
In only 92% of children with the diagnosis “inguinal hernia” an open IIR was found (n = 804, Fig. 7). In 4% of patients (n = 35) the IIR was closed unexpectedly (Fig. 2). In the initial 27 of these patients (77%) the swelling (“hernia”) continued to persist postoperatively. Therefore, in the subsequent patients with a closed IIR, the peritoneum was incised, an “inguinal lipoma” resected (Fig. 6), the IIR narrowed by vicryl sutures and the peritoneum closed.
In 31 of the no-open IIR-children, the IIR was completely flat, without any depression. In four children, minor depressions were seen of various depths. The remainder of patients had either direct hernias or combinations hereof as described earlier [1].
Among the 28 children with recurrences, in five (18%) only the former suture, but no open IIR was found (Fig. 7). In four of these patients an open hernia repair had been performed, in one child the previous procedure was laparoscopy. In six children (21%) a small opening was identified, too small to permit organ prolapse or a veritable hernia. In seven children (25%) the former suture had partially opened (Fig. 8) and in 10 (36%) the opening was as big as before.
In a further 2-year-old boy with a left-sided hernia a 2 mm-diameter open processus vaginalis was found on the right side and was sutured. Two years later on that side a direct inguinal hernia was noted.
Discussion
The concept of either having a hernia or not, or having a recurrence or not, is based on the surgeons’ visual impressions obtained during the open approach. Laparoscopy has modified the picture.
In an inguinal hernia, as seen during laparoscopy, a full spectrum from a shallow depression to a clinical scrotal hernia is found.
In Greek, “hernia” means “swelling”. Herniotomy means “to cut into the swelling”.
Laparoscopy, in contrast, demonstrates open IIRs, not exactly hernias. Laparoscopy exposes a discrepancy between open IIR and hernia. As a consequence, the surgeon has become uncertain as to whether to close any open IIR encountered. If the concept of “herniotomy” is to be preserved it would be adequate to only close any open IIR, which clinically has presented as a “hernia”, and to leave an IIR open which never presented as a hernia. However, nobody knows how many open IIRs subsequently develop into a hernia. The fact that metachronous hernias are far less frequently seen after laparoscopic repair, if all open IIRs are closed routinely, point to the possibility that open IIRs become hernias in a percentage similar to the incidence of metachronous hernias.
On the other side, there evidently are hernias and recurrences without open IIRs. The dilemma is known from open surgery [7]. The surgeon’s immediate reflex is to declare an “incorrect diagnosis”. However, the swelling is there. Hernia in Greek simply is swelling. The question is what to do in these instances. At present, and as long as no better concept is provided, it seems acceptable to open the peritoneum at the site of the IIR, search for an (almost always present) inguinal lipoma, remove it and close the IIR with sutures. Based on the limited number of patients we saw, it appears that this measure overcomes the swelling. Analogous swellings caused by lipomata are found in open surgery. Also, in adult patients a similar percentage of lipomata were found in patients with postoperatively persistent groin swellings [6]. It has been suggested to remove any lipoma in the presence of an open IIR [2]. The concept is that a sliding lipoma represents “a sliding herniation of preperitoneal fat into the inguinal canal, forming a reducible indirect inguinal hernia in the absence of a peritoneal sac” [5]. Even if the removal of the lipoma as such does not cure the hernia, the procedure in itself may cause sufficient trauma and subsequent scarring to do away with the swelling.
A parallel situation is found in “recurrences”. In more than a third of patients, diagnosed with having a “recurrence”, the IIR was found to be either completely closed or to feature only a 2-mm-diameter opening. It is conceivable that the small opening permits passage of intra-abdominal fluid, producing groin swelling and mimicking a hernia. The phenomenon is known from patients with VP shunts. But there are “recurrences” without an open IIR. In analogy with primary inguinal hernias we would suggest considering incision of the peritoneum, check for a lipoma and remove it. In adult patients, missed lipomata are a known cause of recurrences [3] and their removal in the absence of an open IIR has been suggested repeatedly [4].
There is a group of children without open IRRs and without lipomata. The highest risk of diagnosing a hernia without an open IIR and without lipomata was observed in boys with preoperatively diagnosed “bilateral inguinal hernias”. In some of these children several flat depressions were found, not only at the site of indirect hernias, but also at the site of direct and femoral hernias: at the absence of any noticeable deep open IIR. At present we do not know how to treat these children adequately. Placement of a mesh, completely covering all the affected area, as practised in adult patients, may in theory be an option. In practice, however, nobody would expect a growing child to deal for life with the unwanted side effects of a foreign body placed into the lower abdominal wall.
Also, with a recurrence, a partial opening may allow prolapse and create a swelling. If, however, the opening is barely small enough to allow passage of intra-abdominal fluid but not prolapse, the term “recurrence” appears questionable. Nevertheless we have sutured these openings if encountered.
The clinical implications of these observations are obvious. Strictly correlating “hernia” to an open IIR will not fully describe the clinical picture of a hernia. In open inguinal hernia repair in children lipomata are no problem. This is owed to the local dissection in order to gain access to the IIR from outside, thereby creating postoperative scarring which stabilises the surgical result no matter whether the diagnosis was absolutely correct to begin with. Even if a lipoma is left behind, it will be caught within scars and prevent a new swelling. Laparoscopy in contrast is unable to profit from this collateral damage.
However, the laparoscopic picture of a hernia or a recurrence seems not fully adequate either. Abdominal distension due to CO2 insufflation may flatten out minor depressions. Only minimum insufflation allows a correct picture.
In summary, there are three conclusions. First, the correlation between an open IIR and a hernia is unknown. Since metachronous hernias are observed less frequently after routine closure of any open IIR, it appears permitted to laparoscopically close any open IIR encountered. Second, almost half of the recurrences are not failures of surgical IIR closure. They are more complex phenomena. Inguinal lipomata may be responsible in a part of these patients. Third, there remains a fraction of children in whom several depressions are seen laparoscopically and also swellings being seen from outside, but no obvious open IIR is identified laparoscopically. The abdominal wall seems more pliable in these patients than in others. No surgical procedure is indicated in these children because they carry no risk of incarceration.
References
Schier F (2006) Laparoscopic inguinal hernia repair––a prospective personal series of 542 children. J Pediatr Surg 41:1081–1084
Carilli S, Alper A, Emre A (2004) Inguinal cord lipomas. Hernia 8:252–254
Felix E, Scott S, Crafton B, Geis P, Duncan T, Sewell R, McKernan B (1998) Causes of recurrence after laparoscopic hernioplasty. A multicenter study. Surg Endosc 12:226–331
Gersin KS, Heniford BT, Garcia-Ruiz A, Ponsky JL (1999) Missed lipoma of the spermatic cord. A pitfall of transabdominal preperitoneal laparoscopic hernia repair. Surg Endosc 13:585–587
Lau H (2004) Sliding lipoma: an indirect inguinal hernia without a peritoneal sac. J Laparoendosc Adv Surg Tech A 14:57–59
Shpitz B, Kuriansky J, Werener M, Osadchi A, Tiomkin V, Bugayev N, Klein E (2004) Early postoperative evaluation of groins after laparoscopic total extraperitoneal repair of inguinal hernias. J Laparoendosc Adv Surg Tech A 14:353–357
Waters KJ (1999) Clinical dilemma. A hernia sac cannot be found at operation. Br J Surg 86:1107
Schier F, Montupet PH, Esposito C (2002) Laparoscopic inguinal herniorrhaphy in children: a three-centre experience with 933 repairs. J Pediatr Surg 37:395–397
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schier, F. The laparoscopic spectrum of inguinal hernias and their recurrences. Pediatr Surg Int 23, 1209–1213 (2007). https://doi.org/10.1007/s00383-007-2018-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-007-2018-3