Abstract
Treatment of “forme fruste” choledochal cyst (FFCC) where pancreaticobiliary malunion (PBMU) is associated with minimal dilatation of the common bile duct (CBD) remains controversial. PBMU allows pancreaticobiliary reflux to occur, which causes complications such as recurrent pancreatitis and gallbladder cancer. Therefore, some surgeons opt to treat FFCC by cholecystectomy alone in order to prevent gallbladder cancer, with the result that pancreaticobiliary reflux could still occur. Our treatment of choice—excision of both the CBD and the gallbladder, followed by Roux-en-Y hepatico-jejunostomy—can eliminate pancreaticobiliary reflux and prevent complications. Our case, a 2-year-old boy, initially presented to a hospital abroad with recurrent abdominal pain. Endoscopic retrograde cholangiopancreatography showed massive protein plugs impacted in the papilla of Vater and mild CBD dilatation, but PBMU was not identified. Intraoperative cholangiography performed during laparotomy 5 days later suggested PBMU with minimal CBD dilatation. Despite these findings, cholecystectomy with T-tube drainage was performed rather than CBD excision with biliary reconstruction. Postoperative T-tube cholangiography clearly showed PBMU. The T-tube was removed after 2 weeks, and 3 months later the boy was referred to us because of recurrent pancreatitis. We performed CBD excision and Roux-en-Y hepatico-jejunostomy. His postoperative course was uneventful, and he is well after 10 years of follow-up. This case provides strong evidence that CBD excision with biliary reconstruction is mandatory for treating FFCC and, conversely, that cholecystectomy alone is inadequate for treating children with FFCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreaticobiliary malunion (PBMU) was first reported by Arnolds in 1906 in an autopsy case with dilatation of the common bile duct (CBD)—that is, choledochal cyst [1]. PBMU is almost always associated with choledochal cyst [2] and is generally regarded to be a congenital anomaly that is frequently associated with malignancy of the biliary tract. The first such case, a case of bile duct carcinoma arising in the wall of a choledochal cyst, was reported by Irwin and Morison in 1944 [3]. Thus, PBMU has come to be regarded as a precancerous condition, and surgical intervention, such as resection of the gallbladder or extrahepatic bile duct or both, is usually performed irrespective of evidence for malignancy.
Recent advances in diagnostic techniques have shown that some PBMU patients have minimal or no dilatation of the extrahepatic bile duct, the so-called “forme fruste” choledochal cyst (FFCC), and for these cases, the optimal treatment is controversial. We experienced a case of FFCC in whom resection of the CBD was necessary after cholecystectomy due to recurrent episodes of pancreatitis.
Our case report illustrates that, in children, dissolution of the anomalous junction between the CBD and pancreatic duct with a diversion procedure (CBD excision and biliary reconstruction) is mandatory for preventing complications in the long term.
Case report
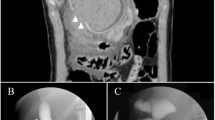
A 2-year-old Japanese boy was admitted to a hospital abroad for investigation of recurrent abdominal pain and jaundice. Endoscopic retrograde cholangiopancreatography (ERCP) showed massive protein plugs impacted in the papilla of Vater, with mild secondary dilatation of the CBD. ERCP failed to demonstrate the pancreatic duct, so PBMU, characterized by a long common channel, could not be identified. Five days later, laparotomy was performed. Intraoperative cholangiography suggested PBMU with minimal dilatation of the CBD, but no protein plugs were seen, and it was assumed they had been dislodged spontaneously after ERCP. Despite evidence that PBMU was present, cholecystectomy with T-tube drainage was performed instead of a diversion procedure (CBD excision with biliary reconstruction). Postoperative T-tube cholangiography clearly showed PBMU (Fig. 1). The T-tube was removed 2 weeks after surgery; however, 3 months later, the boy was referred to our hospital because of recurrent abdominal pain.
On admission, physical examination revealed normal vital signs with no evidence of jaundice or anemia, but laboratory data showed high levels of serum amylase. One week after hospitalization, CBD excision and Roux-en-Y hepatico-jejunostomy were performed. The level of amylase measured in aspirate from the CBD at the time of surgery was 10 IU/l. Intraoperative cyst endoscopy with a pediatric cystoscope showed the presence of debris in both the intrahepatic and intrapancreatic bile ducts, and these were flushed clean with normal saline by irrigation through the cystoscope. Macroscopically, the excised CBD had a thickened wall. The outer diameter of the CBD was only 8 mm, and its lumen was 5 mm. Microscopically, the excised biliary duct showed chronic inflammation with fibrous change. No malignant cells were seen. The postoperative course was uneventful, and the patient is currently well with no episodes of pancreatitis or cholangitis after 10 years of follow-up.
Discussion
PBMU is defined as an anomalous junction between the pancreatic duct and the CBD that lies outside the duodenal wall and beyond the influence of the sphincter of Oddi [4]. It is more common in Japan than in the United States or Europe [5]. PBMU allows pancreatic secretions to constantly regurgitate into the biliary duct, where bile activates enzymes secreted by the pancreas, damaging the biliary mucosa [6].
ERCP studies have shown that the bile duct is not always dilated in cases of PBMU. In 1981, Okada et al. [7] were the first to report a case of choledochal cyst with minimal dilatation of the cyst and called it “common channel syndrome.” It was later renamed FFCC by Lilly et al. in 1985 [8].
Most FFCC in adults is diagnosed incidentally because of an anomaly of the gallbladder; i.e., tumor, polyp, or thickening of the wall [9]. Simple cholecystectomy in adults presenting with FFCC has been justified because of the high incidence of associated gallbladder carcinoma [10]. In other words, excision of the CBD was regarded as unnecessary because in adults, CBD carcinomas develop rarely in PBMU without choledochal cyst [11].
In 1995, to investigate risks for carcinogenesis, the Japanese Study Group on Pancreaticobiliary Maljunction (JSPBM) conducted a national survey of 569 patients with PBMU who underwent surgery [12]. This study showed that the incidence of bile duct carcinoma in cases of noncystic type PBMU was lower than that for cases with cystic type regardless of patient age. In fact, the incidence was almost equal to the incidence for 12,399 control patients without PBMU who underwent biliary surgery. The JSPBM also conducted a national case registration from 1990 to 1998 and found that biliary tract carcinomas occurred in 138 (39.3%) of 351 patients with undilated type PBMU, of which the majority was found in the gallbladder or the intrahepatic bile duct, with only two cases occurring in the extrahepatic bile duct [13].
Although carcinogenesis in PBMU is not yet clearly understood, regurgitation of pancreatic secretions may play an important role in provoking malignant changes. Even after simple cholecystectomy, pancreatic secretions continue to come in contact with the bile duct because of PBMU. This contact allows the biliary epithelium to be damaged, leading to fibrosis, inflammatory cell infiltration, chronic pancreatitis, and malignant changes [8]. Todani et al. collected and analyzed 1,062 cases of PBMU from the Japanese literature and found the incidence of carcinoma of the biliary duct in FFCC to be as high as 12.2% [14]. Although our case was not associated with biliary carcinoma, there was chronic inflammation of the resected CBD mucosa, which could have progressed to carcinoma later in the patient’s life.
Although the hydrostatic pressure within the pancreatic duct is usually greater than that in the bile duct [15], bile may reflux into the pancreatic duct under certain circumstances if there is an anomalous junction, such as during postprandial gallbladder emptying. Such reflux could contribute to acute pancreatitis. Because our case had high levels of serum amylase and recurrent episodes of abdominal pain, we considered that he had recurrent pancreatitis as a complication of simple cholecystectomy. In hindsight, his clinical symptoms and laboratory data were most likely caused by stasis or obstruction at the level of the long common channel directly associated with the pathogenesis of PBMU. It is difficult to resolve these pathological symptoms without a diversion procedure, such as resection of the CBD followed by Roux-en-Y hepatico-jejunostomy. If PBMU is found accidentally in an asymptomatic child, close observation is required, and if any symptoms at all are noted, CBD excision with biliary reconstruction is recommended. However, close postoperative follow-up is required because postoperative stricture formation and recurrent cholangitis are problems associated with reconstruction of the nondilated biliary tree [8].
In conclusion, given the long lifespan of pediatric patients, PBMU must be treated in children, unlike in adults, and dissolution of the anomalous junction between the CBD and the pancreatic duct by excising the CBD and reconstruction are critical to prevent serious long-term complications. We recommend CBD excision and Roux-en-Y hepatico-jejunostomy as the treatment of choice in children with FFCC.
References
Arnolds (1906) Eine manneskopfroben Retentionszyste des choledochus. Dtsch Med Wochenschr 32:1804
Miyano T, Yamataka A, Li L (2000) Congenital biliary dilatation. Semin Pediatr Surg 9:187–195
Irwin ST, Morison JE (1944) Congenital cyst of common bile duct containing stones and undergoing cancerous change. Br J Surg 32:319–321
Komi N, Funabiki T (1997) Diagnostic criteria of pancreaticobiliary maljunction. Pancreaticobiliary Maljunction:3–4
Alonso-Lej F, Rever WB Jr, Pessagno DJ (1959) Congenital choledochal cyst, with a report and analysis of 94 cases. Int Abst Surg 108:1–30
Mizuno M, Kato T, Koyama K (1996) An analysis of mutagens in the contents of the biliary tract in pancreaticobiliary maljunction. Surg Today 26:597–602
Okada A, Nagaoka M, Kamata S, et al. (1981) Common channel syndrome—anomalous junction of the pancreatico-biliary ductal system. Z Kinderchir 32:144–151
Lily JR, Stellin GP, Karrer FM (1985) Forme fruste choledochal cyst. J Pediatr Surg 20:449–451
Tanaka K, Nishimura A, Yamada K, et al. (1993) Cancer of the gallbladder associated with anomalous junction of the pancreatobiliary duct system without bile duct dilatation. Br J Surg 80:622–624
Sugiyama M, Atomi Y (1998) Anomalous pancreaticobiliary junction without congenital choledochal cyst. Br J Surg 85:911–916
Azuma T, Hanyu F, Nakamura, et al. (1996) A clinical study on surgical treatment for anomalous arrangement of the pancreaticobiliary ductal system without dilatation of the common bile duct (in Japanese). Jpn J Gastroenterol Surg 29:806–812
Hasumi A, Sugaya H, Aoki H (1995) Pancreaticobiliary maljunction and biliary tract cancer [in Japanese]. J Bil Panc 16:753–757
Tashiro S, Yokita S, Matsumura T (2001) Pancreaticobiliary maljunction without dilatation of the bile duct is a high risk factor of biliary cancer: a study of the registered cases in Japan [in Japanese]. J Bil Panc 22:469–474
Todani T, Watanabe Y, Fujii T (1985) Carcinoma arising from the bile duct in choledochal cyst and anomalous arrangement of the pancreaticobiliary ductal union [in Japanese]. Tan to Sui (The Biliary Tract and Pancreas) 6:525–535
Menguy RB, Hallenbeck GA, Bolman JL, et al. (1958) Intraductal pressures and sphincteric resistance in canine pancreatic and biliary ducts after various stimuli. Surg Gynecol Obstet 106:306–320
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyano, G., Yamataka, A., Shimotakahara, A. et al. Cholecystectomy alone is inadequate for treating forme fruste choledochal cyst: evidence from a rare but important case report. Ped Surgery Int 21, 61–63 (2005). https://doi.org/10.1007/s00383-004-1266-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-004-1266-8