Abstract
Post-traumatic clival hematomas are a rare entity and almost exclusive to the pediatric population. Those of retroclival location are exceptionally rare. This entity was first described in 1941 by Coleman and Thomson, and since then, less than 30 cases have been reported in the literature. Clinically, these hematomas are usually silent and slow, but clinical state worsening may be sudden and rapidly fatal by the onset of obstructive hydrocephalus in the absence of prompt treatment. Here, the authors report a new case of pediatric post traumatic retroclival epidural hematoma following a minor blunt head trauma in a 03-year-old male patient with good outcomes. The authors will proceed with a review of the literature regarding the pathophysiology and mechanisms of occurrence of such post-traumatic injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-traumatic clival hematomas are a rare entity and almost exclusive to the pediatric population [1,2,3]. Hematomas can be epidural or subdural and can be difficult to differentiate on imaging, the anatomy of the tectorial membrane being a reference [4]. Those of retroclival location are exceptionally rare [3, 5, 6]. This entity was first described in 1941 by Coleman and Thomson [6], and since then, less than 30 cases of posttraumatic retroclival epidural hematoma have been reported in the literature [7]. Clinically, these hematomas are usually silent and slow, but clinical state worsening may be sudden and rapidly fatal by the onset of obstructive hydrocephalus in the absence of prompt treatment [6].
Here, the authors report a new case of pediatric post traumatic retroclival epidural hematoma following a minor blunt head trauma in a 3-year-old male patient with good outcomes. The authors will proceed with a review of the literature regarding the pathophysiology and mechanisms of occurrence of such post-traumatic injury.
Case report
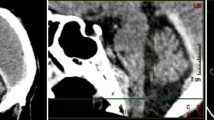
A 3-year-old male patient with no particular medical or surgical history and good cognitive, emotional, communicative, and motor capacities was brought by his mum to the emergency room then to our neurosurgery department for management of head trauma. The child’s mum reported that her son fell out from his bed from a height of about 0.5 m with occipital landing 4 h before admission. She also reported that her boy vomited several times without any episodes of generalized or focal seizures. A standard general physical check-up was performed and revealed no abnormalities apart from a discreet shallow subcutaneous bump next to the traumatic occipital impact point without oozing blood, bruise, or loss of cutaneous continuity. The boy did not seem to be dazed or shocked. Temperature, pulse rate, respiratory rate, blood pressure (with cuff covering 2/3 of the upper arm), weight, height, and head circumference were in normal range. On neurological examination, the boy was reactive and vitally stable. His Glasgow Coma Scale was assessed to be 15/15. His pupils were bilaterally equal, round, and reactive to light. The rest of the examination was within normal confines. The chest X-ray was normal. A complete blood count as well as serum electrolytes blood test was all in normal range. An urgent brain computed tomography (CT) scan (Fig. 1) was performed showing a retroclival lens-shaped hyperdensity, lateralized on the right side, of regular contours, coming into contact with the dorsum sella, measuring 17 × 9 mm in diameter suggestive of an epidural retroclival hematoma. There were no signs of either associated upper cervical spine dislocation or clival fracture over the hematoma.
Non-enhanced brain CT scan in axial (a, d parenchymal and bone window respectively), sagittal (b, e parenchymal and bone window respectively), and coronal plane (c, f parenchymal and bone window respectively) showing a retroclival lens-shaped hyperdensity (red arrows), measuring 17 × 9 mm in diameter, lateralized on the right side, of regular contours, coming into contact with the dorsum sella. Note the absence of neither associated upper cervical spine dislocation nor clival fracture over the hematoma on bone window images (d, e, f) and the persistence of the spheno-occipital synchondrosis (e yellow arrow)
Regarding the reassuring clinical condition of the patient at the time of admission, it was decided to maintain a conservative treatment under strict neurological surveillance and close monitoring of his hemodynamic condition. The control brain CT scan (Fig. 2) performed 5 days later showed the stability in size of the hematoma. CT angiography revealed no other apparent abnormalities such as aneurysm, occult arteriovenous malformation, or traumatic arterial dissection.
During all the surveillance period, the patient had no further episodes of vomiting or cranial nerve palsy. He continued to progress until his discharge ten days after the traumatic event with close appointment at the out-patient clinic. He returned after a week of discharge and he was fully asymptomatic over subsequent visits.
Discussion
Trauma is the most common cause of extradural hematomas [6]. Most cases are associated with skull fractures and unlike supratentorial epidural hematomas, which are mainly due to arterial damage, most extradural hematomas in the posterior cerebral fossa are due to involvement of the venous sinuses [6, 8]. The higher incidence of such hematoma in pediatric population may be due to cervical muscle and ligamentous immaturity of the craniocervical junction, as well as the increased head-body ratio characteristic of this age group [1, 9]. However, the pathophysiology of these retroclival epidural hematomas is not yet well elucidated [5, 6]. It has been suggested that the particular characteristics of the craniovertebral junction predispose to these hematomas since there is a precarious stability of this junction essentially during childhood [5] as the occipital condyles are relatively smaller and the atlantooccipital joint is oriented more horizontally. In addition, damage and dislocation of the ligament tissues connecting the odontoid process to the skull base could be involved in this pathophysiology. Elongation as well as dislocation of the tectorial membrane, posterior longitudinal ligament, and cruciate ligament could disrupt local vascular structures at the cervico-occipital hinge (basilar venous plexus, dorsal meningeal branch of the meningohypophyseal trunk) leading to the onset of retroclival bleeding [6, 10].
Clinically, retroclival epidural hematoma is usually silent and slow or may be associated with raised intracranial pressure [6]. Few cases of post-traumatic subdural and not epidural retroclival hematomas have been reported in adult patients, with symptoms of raised intracranial pressure and paralysis of the VI nerve in the first hours after the trauma [11, 12]. Our patient did not show obvious signs of damage to the 6th cranial nerve, and his intracranial hypertension was limited to a few episodes of vomiting.
According to the literature, the hematoma’s size has no correlation with the severity of symptoms and clinical signs [1, 5]. Just as the initial state of consciousness, judged by the Glasgow score, does not make it possible to predict the prognosis of patients [1, 5, 10].
Brain CT scan is the first-line imaging method. However, beam hardening may mask this type of hematoma [13]. Multiplanar reconstructions, particularly sagittal ones, and CT angiography can increase the sensitivity of CT for the detection of retroclival hematomas and add other information such as possible clival fracture or associated vascular lesion. MRI is the most sensitive diagnostic tool for diagnosing these lesions [6]; it makes it possible to overcome the beam hardening encountered on the CT scan, with great sensitivity thanks to the gradient echo sequences sequence allowing the detection of hemoglobin degradation products, such as deoxyhemoglobin which is responsible for a hyposignal by effect of magnetic susceptibility.
Regarding management, a review of the literature [5,6,7] showed that conservative treatment is generally adopted as first-line treatment as it was decided for our patient. However, the management of these hematomas will depend on associated injuries, degree of brainstem compression, progression of hydrocephalus, and/or cranial nerve palsies, in which case surgical treatment should be sought. Approaches most frequently used for the drainage of this type of hematoma are the sub-occipital, sub-temporal, and the extreme lateral, although previous approaches supported by endoscopy have been reported [14].
Conclusion
Post-traumatic retroclival epidural hematoma remains pathology almost exclusive to pediatric population, and although there are few cases reported in the literature, it is possible that this entity is often underdiagnosed and must involve CT scan investigation of cervico-occipital hinge to rule out predisposing underlying ligament instability.
Availability of data and materials
Mehdi Borni was responsible for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
References
Kwon T-H, Joy H, Park Y-K, Chung H-S (2008) Traumatic retroclival epidural hematoma in a child: case report. Neurol Med Chir 48:347–350
Guillaume D, Menezes AH (2006) Retroclival hematoma in the pediatric population: report of two cases and review of the literature. J Neurosurg 105:321–325 PEDIAT
Tahir M, Quadri S, Hanif S, Javed G (2011) Traumatic retroclival epidural hematoma in pediatric patient–case report and review of literature. Surg Neurol Int 2:78
Suliman HM, Merx HL, Wesseling P, van der Sluijs B, Vos PE, Thijssen HOM (2001) Retroclival extradural hematoma is a magnetic resonance imaging diagnosis. J Neurotrauma 18:1289–1293
Shane Tubbs R, Christoph PhD, Griessenauer JTHM (2010) Retroclival epidural hematomas: a clinical series. Neurosurgery 67:404–407
Bernardo Ratilal MD, Pedro Castanho MD, Carlos Vara Luiz MD, Joa˜o Oliveira Antunes M (2006) Traumatic clivus epidural hematoma: case report and review of the literature. Surg Neurol 66:200–202
Nguyen HS, Shabani SLS (2016) Isolated traumatic retroclival hematoma: case report and review of literature. Childs Nerv Syst 32:1749–1755
Mizushima H, Kobayashi NSY (1998) Epidural hematoma of the clivus. Case report J Neurosurg 88:590–593
Silvera VM, Danehy AR, Newton AW, Stamoulis C, Carducci C, Grant PE, Wilson CR, Kleinman PK (2014) Retroclival collections associated with abusive head trauma in children. Pediatr Radiol 44(Suppl 4):S621-631
BP Y (2003) Traumatic retroclival epidural hematoma in a child. Pediatr Neurosurg 39(6):339–340
Tubbs RS, Griessenauer CJ, Hankinson T, Rozzelle C, Wellons JC, Blount JP, Oakes WJ, Cohen-Gadol AA (2010) Retroclival epidural hematomas: a clinical series. Neurosurgery 67(2):404–406
Catalá-Antúnez I, de Quintana-Schmidt C, Clavel-Laria P, Montes-Graciano G (2011) [Abducens nerve palsy due to postraumatic retroclival and spinal subdural hematoma: case report and literature review]. Molet-Teixidó J Neurocir 22:337–341
Paterakis KN, Karantanas AH, Hadjigeorgiou GM, Anagnostopoulos VKAC (2005) Retroclival epidural hematoma secondary to a longitudinal clivus fracture. Neurol Neurosurg 108:67–72
Marks SM, Paramaraswaren RN, Johnston RA (1997) Transoral evacuation of a clivus extradural haematoma with good recovery: a case report. Br J Neurosurg 11:245–247
Author information
Authors and Affiliations
Contributions
All the authors contribute to write this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interest
The authors declared no potential conflicts of interests with respect to research, authorship and/or publication of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borni, M., Abdelmouleh, S., Bounemra, M. et al. Isolated pediatric retroclival epidural hematoma following a minor blunt head trauma: a case report with review of the literature. Childs Nerv Syst 39, 807–810 (2023). https://doi.org/10.1007/s00381-022-05686-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05686-2