Abstract
Congenital intracranial meningiomas are rare lesions. We present a case of congenital intraventricular cystic meningioma, initially characterized with fetal MRI and confirmed postnatally with histopathology. To our knowledge, this is the first in vivo description of a congenital meningioma with fetal MRI. The fetal MRI was able to characterize the lesion as an atypical intraventricular mass which was separate from the choroid plexus, differentiating the mass from a choroid plexus neoplasm. An intraventricular location of the meningioma is more commonly described in pediatric than in adult patients. Meningioma should be considered in the differential for an intraventricular congenital lesion, and fetal MRI is advocated for lesion characterization.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital central nervous system (CNS) tumors are uncommon. They account for 0.5% to 1.5% of all congenital tumors, although the true incidence is underestimated as some result in fetal demise [1]. These tumors are most often identified on routine antenatal ultrasound or postnatally. For those identified with antenatal screening, fetal MRI has been advocated to clarify the anatomical extent of the tumor and diagnose intracranial complications and to assess fetal development [2]. Congenital meningiomas are rare, and an intraventricular location of the meningioma is more commonly described in pediatric than adult patients [3]. We present a case of a congenital intraventricular meningioma, detected antenatally and imaged with fetal MRI, which subsequently underwent postnatal surgical resection. While the eventual diagnosis of an intraventricular cystic meningioma was made histologically, the fetal MRI was able to characterize the lesion, and more importantly exclude other pathologies of the CNS which may be missed on conventional antenatal ultrasound. The examination also served as a baseline for the early postnatal MRI imaging that was performed.
Case report
A G2P1 30-year-old with no significant family history, a normal first trimester screen, and a normal non-invasive prenatal test result underwent a routine fetal anatomy ultrasound at 20-week gestation, showing a unilateral slightly complex intraventricular cystic lesion. A specialist tertiary ultrasound at 25 weeks and 6 days confirmed the presence of a heterogenous echogenicity avascular cystic lesion within the left lateral ventricular trigone causing mild unilateral ventriculomegaly, and resulting in displacement of the adjacent choroid plexus (Fig. 1). The remainder of the fetal anatomical survey was unremarkable. The patient proceeded to fetal MRI at 27-week 2-day gestational age (Fig. 2) which confirmed the presence of a left intraventricular multi-septated cystic lesion, which was T2 hypointense relative to CSF, slightly hyperintense to CSF on T1 weighted imaging, and did not demonstrate abnormal susceptibility or restricted diffusion. The left lateral ventricle was dilated and the cavum septum pellucidum was deviated to the right. No other intracranial abnormalities were detected on MRI.
Fetal MRI brain performed at 27-week and 2-day gestation showing a cystic lesion expanding the left lateral ventricle. Top row (a–c) showing axial, sagittal, and coronal T2 weighted imaging of the left sided intraventricular lesion, which is T2 hyperintense with subtle low signal internal septations, with the lesion slightly lower signal than CSF, d Axial T1WI showing the lesion as hypointense to brain but mildly hyperintense to intraventricular CSF, e–f Axial DWI trace and ADC respectively showing facilitated diffusion in the lesion, g Axial gradient echo showing no intralesional susceptibility
Serial ultrasound examinations at 30-, 33-, and 36-week gestation demonstrated absolute growth of the lesion; however, this was relatively proportional to overall fetal brain growth. The patient underwent a semi-elective cesarean section at 38 weeks and 6 days without maternal or fetal complications. The newborn fetal Apgar scores were 8 and 9. A cranial ultrasound on day 0 of life showed similar size of the cystic lesion compared with the late antenatal ultrasounds, without development of hydrocephalus (Fig. 3). The first postnatal MRI brain examination on day 3 showed similar size of the lesion, although it was associated with some new focal restricted diffusion corresponding to more solid components of the mass. A subsequent MRI performed 2 months later showed the lesion to have remained stable in size, but shows further evolution of signal characteristics, with larger solid components which showed enhancement and mild restricted diffusion (Fig. 4). At 4 months of age, a gross total excision was performed via a trans-sulcal craniotomy. Histopathological diagnosis was of an atypical meningioma, WHO grade II (mitotic index 7/10 hpf) (Fig. 5). By immunohistochemistry the tumor was negative for EMA, but positive for vimentin, progesterone receptor, E-Cadherin, and D2-40, consistent with the immunophenotype of a meningioma (Fig. 5). There were no peri-operative complications. As of 2 years post-surgical excision, the patient is in good physical health with normal development.
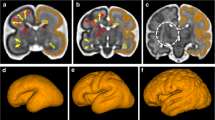
Neonatal brain MRI at 2 months of age. a, b Axial T2 weighted imaging showing the multiseptated cystic lesion expanding the left lateral ventricle, slightly hypointense to CSF, c Coronal FLAIR showing partial suppression of the internal cystic components of the lesion with hyperintense septations and nodular components inferiorly, d Axial T1 weighted imaging showing the lesion to be heterogeneously hypointense, but mildly hyperintense to CSF with hyperintense septations, e, f Trace DWI and ADC maps respectively showing restriction in the more solid component of the lesion, g Axial SWI showing no intralesional susceptibility, h Axial T1 weighted imaging after gadolinium administration showing nodular enhancement of the diffusion restricting components of the lesion. Arrow showing the choroid plexus separate to and displaced anteriorly by the lesion
MRI brain acquired post-surgical resection. a Axial T2 showing the surgical resection of the left lateral intraventricular lesion via a left parietal approach, b Axial post gadolinium sequence confirming the absence of any residual parenchymal, ependymal or leptomeningeal enhancement, c Coronal FLAIR sequence through the ventricular trigones demonstrating the ventriculomegaly secondary to the known tumor
a Low magnification image of the tumor, showing variable cellularity, central vascularity, and tumor circumscription (H&E, ×20), b High magnification to show the relatively uniform and bland tumor cell nuclei, delicate cytoplasm and prominent tumor-associated blood vessels (H&E, ×400), c High magnification to show an area with increased mitotic activity (arrows) (H&E, ×400), d E-cadherin immunohistochemical staining of tumor cells (E-cadherin, ×40)
Discussion
To our knowledge, this is the first in vivo description of a congenital meningioma with fetal MRI. This presented as an intraventricular complex cystic lesion causing unilateral ventriculomegaly and displacing the adjacent choroid plexus. The lesion showed absolute growth over time when followed with ultrasound and MRI antenatally; however, this was not greatly out of proportion to overall antenatal brain growth. Post-natal MRI further characterized the lesion as being a solid-cystic mass with nodular enhancing components showing restricted diffusion. Albeit rare, a complex intraventricular cystic mass, separate to the choroid plexus, when detected on antenatal imaging should raise the possibility of an intraventricular congenital meningioma. Choroid plexus tumors can also rarely present as intraventricular cystic masses, the so-called cystic variant of choroid plexus papilloma; however, these lesions are described as arising from the choroid plexus, unlike our case, which was clearly separate to the choroid, displacing it [4, 5]. Fetal MRI characterized the relationship of the lesion to the choroid, and this examination finding may aid clinicians in the workup of fetal intraventricular lesions in the future.
Data availability
Not applicable.
Materials availability
Not applicable.
Code availability
Not applicable.
References
Stiller CA, Bunch KJ (1992) Brain and spinal tumours in children aged under two years: incidence and survival in Britain, 1971-85. Br J Cancer Suppl 18:S50–S53
Milani HJ, Araujo Junior E, Cavalheiro S, Oliveira PS, Hisaba WJ, Barreto EQ, Barbosa MM, Nardozza LM, Moron AF (2015) Fetal brain tumors: Prenatal diagnosis by ultrasound and magnetic resonance imaging. World J Radiol 7:17–21
Hong S, Usami K, Hirokawa D, Ogiwara H (2019) Pediatric meningiomas - a report of 5 cases and review of the literature. Childs Nerv Syst 35:2219–2225
Miyagi Y, Yoshihiro N (2006) Satoshi OS et. al. Purely cystic form of choroid plexus papilloma with acute hydrocephalus in an infant. J Neurosurg 105:480–484
Murata M, Morokuma S, Tsukimori K et al (2009) Rapidly growing cystic variant of choroid plexus papilloma in a fetal cerebral hemisphere. Ultrasound Obstet Gynaecol 33(1):116–118
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to this case report, either via diagnosis or resection of the lesion.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval was not required for this case report.
Consent to participate
We explained the content and purpose of the case report to the patient’s mother after the lesion was successfully resected and the histopathology results were finalized. The patient’s mother gave verbal consent and asked for a copy of the manuscript, should it ever be published.
Consent to publication
See consent to participate.
Conflicts of interest / competing interest
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, J., Lakshmanan, R., Dyke, J.M. et al. Case report: congenital intraventricular meningioma demonstrated with fetal MRI. Childs Nerv Syst 38, 191–194 (2022). https://doi.org/10.1007/s00381-021-05067-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05067-1