Abstract
Purpose
Pure arterial malformations of the brain are rare vascular lesions.
Methods
We present a 10-year-old healthy boy who presented with an incidental finding of pure arterial malformation.
Results
Our case seems to represent the second description of pure arterial malformation discovered incidentally in a child.
Conclusion
We review the clinical presentation, angiographic findings, and management of our case in the context of other reported pediatric cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, greater attention has been garnered on rare vascular malformations of the brain —“pure arterial malformations”—in both the adult and pediatric age groups [1,2,3,4,5,6,7,8,9]. Moreover, pure arterial malformations are thought to be associated with a benign natural history and should be treated conservatively. At times, these malformations may be mistaken for arteriovenous malformations (AVMs), arteriovenous fistulas (AVFs), or cerebral saccular aneurysms [2,3,4,5].
Incidental presentation of pure arterial malformation in otherwise healthy children has been less frequently described [9]. In this study, we describe the clinical course of one child over 12 months of follow-up.
Case report
History
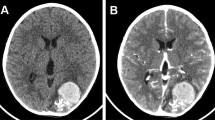
Our patient is a 10-year-old boy who presented after a concussion suffered during a hockey game. He had no relevant past medical history. A noncontrast CT of the head (Fig. 1) suggests abnormal cerebral vasculature. The patient was otherwise asymptomatic.
Examination
Patient displayed a normal neurological examination without focal deficits. There was no pronator drift.
Diagnostic studies
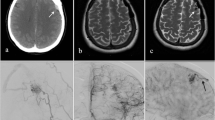
Advanced imaging with CT angiogram (CTA) of the head (Fig. 2) revealed a tortuosity of vessels in the left internal carotid artery segments. Patient then underwent a diagnostic cerebral angiogram (Fig. 3). There was no aneurysm, AV fistula, or early venous phase drainage associated with this malformation.
Clinical course
The patient did well throughout the year of follow-up and at 1 year after the procedure. He remained asymptomatic. There was no growth or change in the morphological appearance of the lesion based on follow-up CTA. Because our patient was asymptomatic with no changed based on noninvasive imaging, the risks of invasive conventional angiography did not seem warranted. He has also returned to playing hockey.
Discussion
Our case was consistent with the previously published incidental case of pure arterial malformation in a child (Table 1) [9].
In one review [9], the authors found that the most common locations for pure arterial malformations were the ACAs and PCoA-PCA complex, as in our patient.
Catheter angiography is an important component to distinguish these entities. Differentiating between AVMs and AVFs, and pure arterial malformations is straightforward as there is no arteriovenous shunting in pure arterial malformations [4, 5].
The etiology of pure arterial malformations is unknown. Some hypotheses include an embryologic defect or insult during development of the intracranial arterial circulation resulting in dysplasia, segmental arterial vulnerability from an acquired insult such as viral infection or genetic mutation later in life, or a chronic healed traumatic dissection of a major intracranial artery [9].
Conservative management as a mainstay of treatment for pure arterial malformations is consistent with case reports and small case series published in the literature [2,3,4,5,6,7,8,9].
Conclusions
Pure arterial malformations are a rare type of brain vascular malformation in the pediatric patient population. Most reported cases have been associated with diseases such as viral infection, PHACE syndrome, and moyamoya disease. Incidental presentation in children is even less common. Diagnosis of these lesions may be challenging; however, catheter angiography may help ascertain the diagnosis of pure arterial malformation. Invasive treatment is generally not indicated. Management consists of surveillance with serial imaging such as MRA.
References
Brinjikji W, Cloft HJ, Flemming KD, Comelli S, Lanzino G (2018) Pure arterial malformations. J Neurosurg 129:91–99
Lanterna LA, Brembilla C, Gritti P (2014) Pure arterial malformation of the posterior cerebral artery (letter). J Neurosurg 121:1007–1008
Lanzino G, Burrows AM, Flemming KD, Cloft HJ (2014) Pure arterial malformations of the posterior cerebral artery (letter). J Neurosurg 120:575
McLaughlin N, McLaughlin RR, Duckwiler G, Martin NA (2013) Pure arterial malformations of the posterior cerebral artery: importance of its recognition. J Neurosurg 119:655–660
McLaughlin N, Duckwiler G, Martin NA (2014) Pure arterial malformations of the posterior cerebral artery. Response (letter). J Neurosurg 120:575–577
Sako T, Uchino A, Saito N (2016) Pure arterial malformation of the posterior inferior cerebellar artery diagnosed by MR angiography. Neuroradiol J 29:283–285
Sorenson TJ, Brinjikji W, Flemming KD, Lanzino G (2018) Pure arterial malformation of the posterior inferior cerebellar artery with interspersed adipose tissue: case report. J Neurosurg Peds 22:261–264
Uchino A, Abe M, Sawada A, Takase Y, Kudo S (2003) Extremely tortuous superior cerebellar artery. Eur Radiol 13(Suppl 6):L237–L238
Yamada K, Hayakawa T, Ushio Y, Mitomo M (1985) Cerebral arterial dolichoectasia associated with moyamoya vessels. Surg Neurol 23:19–24
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thatikunta, M., Raman, N.V., Zieles, K.N. et al. An incidental pure arterial malformation in a child: case report and review of the literature. Childs Nerv Syst 36, 2877–2881 (2020). https://doi.org/10.1007/s00381-020-04539-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04539-0