Abstract
A 5-year-old boy had a thoracolumbar-level MMC that had been repaired at the day after birth and kyphotic deformity got worse as he grew. He complained of discomfort about not being able to take a supine posture and decided to perform surgery for kyphosis. In our case, surgical correction is offered to stop the deformity progression, manage the associated pain, and finally to gain sitting and supine posture. We report the surgical procedure with 4 levels of en bloc kyphectomy and using the lag screws. Especially when lag screws are used, several complications including posterior instrumentation failure, hardware prominence and wound break down can be solved by removing the implants after bone fusion has been achieved.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelomeningocele (MMC) is a congenital disorder leading to functional, cosmetic, and mechanical problems related to the spine and the spinal cord. Patients may suffer from severe kyphosis [17]. The incidence of kyphosis in patients with MMC is around 12–20% [2, 18, 19], and most cases are rigid, reaching high degrees in adolescence [14,15,16]. The deformity may cause recurrent skin ulcerations, impaired sitting balance, and respiratory compromise. Since the first kyphectomy was reported by Sharrard in 1968 [22], several different surgical approaches have been devised. Nevertheless, surgical correction for kyphosis is prone to complications including pseudarthrosis, wound problems, recurrence of deformity, and infections [8, 9, 11,12,13, 20]. Thus, many types of incisions and surgical approaches have been described to overcome some of these problems, but none is ideal. We present a case of severe congenital kyphosis treated with kyphectomy and transcorporal insertion of lag screws.
Clinical presentation
A 5-year-old boy had a thoracolumbar-level MMC that had been repaired on the day after birth. He was also diagnosed with Chiari malformation type II, hydrocephalus, kyphosis, and bilateral club foot, and underwent ventriculoperitoneal shunt surgery and Achilles tenotomy. The kyphotic deformity became worse as he grew. He was paraplegic, with complete loss of bowel and bladder sensation. While continuing conservative treatment for the lumbar kyphotic deformity, the back area protruded more and more, and tenderness occurred (Fig. 1). He complained of discomfort due to the inability to assume a supine posture, and it was decided to perform surgery for kyphosis.
Following prone positioning, the spine was exposed through a posterior midline incision. At the L1–2 level, there is no posterior arch of the vertebrae, and the dural membrane is exposed under the skin. The thin dural sac was carefully dissected, along with the surrounding tissue. After tagging the dura at the top of the L1 level and the bottom of the L4 level, we checked that there was no CSF leakage. Rootlets were checked by dissecting the dual lateral sides of the L1–4 level and cut after cauterization. Next, we performed sufficient dissection of the muscles around the vertebral body, and then performed kyphectomy from T12 to L4 using a threadwire saw (Fig. 2a, b). Even after kyphectomy, lumbar kyphosis was not fully reduced. Following rod installation at the T12 and L5 pedicle screws and the iliac screw using the cantilever maneuver, we were able to reduce the kyphosis to some extent. However, bone-to-bone contact was not achieved because of the kyphectomy defect. We decided that additional internal fixation would be necessary to close the gap between T12 and L5. Lag screws were inserted in the opposite direction between T12 and L5 to close the gap (Fig. 2c). Subsequently, posterior and posterolateral onlay fusion was performed using kyphectomized local bone and allograft bone chips. After surgery, the kyphotic deformity improved from 179° to 35° (Fig. 3a). The child was able to lay down in the supine position.
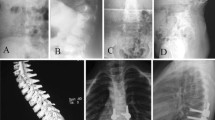
a Immediate postoperative lateral radiograph showing correction of the kyphotic deformity. b 4 months postoperative, removal of the prominent problematic screw and the laminar hook was installed. c 6 months postoperative, proximal laminar hook was being pulled out. All other implants were removed except for the lag screws d 12 months postoperative
However, wound breakdown was observed at 4 months postoperatively, and a computed tomography (CT) scan confirmed that the heads of both screws at the T12 level and the left screw at the L5 level were quite prominent. We removed the problematic screws and installed a laminar hook at the T9, T10, and T11 levels to connect with the iliac screw. After this procedure, the patient’s kyphosis improved even more, and the implant prominence resolved (Fig. 3b). After 3 months, implant prominence occurred again, and an imaging scan confirmed that the proximal laminar hook was being pulled out (Fig. 3c). Seven months after the initial operation, a CT scan confirmed that bone fusion had been successfully achieved, and all other implants were removed except for the lag screws in the vertebral body at the kyphectomy site (Fig. 3d). Subsequently, the patient did not suffer from any other problems and improved, with no difficulties sleeping supine.
Discussion
A kyphotic deformity develops in up to 12–20% of patients with MMC, and adverse outcomes often occur if it is not treated [1]. The kyphotic deformity typically occurs in the upper lumbar and lower thoracic region [7]. With severe kyphosis, patients present with difficulty in lying supine because of the prominent gibbus deformity in the back, making it an uncomfortable and often painful position to maintain. Surgical correction of the kyphotic deformity in patients with MMC has been associated with significant morbidity, with several articles reporting various complications in 83–90% of patients [11, 17, 19]. Most of the complications are related to wound breakdown, but reported complications include hardware prominence, instrumentation failure, junctional kyphosis, infection, cerebrospinal fluid leakage, and death [1, 4,5,6, 11, 21].
In our case, surgical correction was offered to stop the deformity from progressing, to manage the associated pain, and finally to help the patient gain the ability to assume sitting and supine postures. We report a surgical procedure with 4 levels of en bloc kyphectomy in which lag screws were used. Several articles have reported that sufficient vertebral resection can play a significant role in reducing the tension of the skin and improving the skin wound restoration process [10, 20]. A kyphotic deformity can be corrected using kyphectomy, transcorporal lag screw installation, and pedicle screw insertion. We suggest that pedicular screw fixation and fusion with rods can be effective for achieving sagittal balance and for maintaining stability over time. However, repeated instrumentation failures occurred, and two revision operations had to be performed. Eventually, the lag screws were well positioned at the kyphectomy site, allowing solid bone fusion (Fig. 4). Lag screws were invented to close the gap between fractured bone fragments [3]. In this case, we utilized lag screws to close a bony gap following wide kyphectomy.
Given the rarity of this deformity, the optimal treatment remains unclear, although complete kyphectomy and fusion have yielded good outcomes in the literature. Especially when lag screws are used, several complications (including posterior instrumentation failure, hardware prominence and wound breakdown) can be solved by removing the implants after bone fusion has been achieved. We suggest that this surgical strategy could be another procedural option for kyphotic deformity in children.
References
Banta JV, Hamada JS (1976) Natural history of the kyphotic deformity in myelomeningocele. J Bone Joint Surg Am 58:279
Carstens C, Koch H, Brocai DR, Niethard FU (1996) Development of pathological lumbar kyphosis in myelomeningocele. J Bone Joint Surg Br 78:945–950
Cobey MC (1946) Lag-screw fixation in fractures of the tibial tuberosity. J Bone Joint Surg Am 28:273–276
Eckstein HB, Vora RM (1972) Spinal osteotomy for severe kyphosis in children with myelomeningocele. J Bone Joint Surg Br 54:328–333
Furderer S, Hopf C, Schwarz M, Voth D (1999) Orthopedic and neurosurgical treatment of severe kyphosis in myelomeningocele. Neurosurg Rev 22:45–49
Heydemann JS, Gillespie R (1987) Management of myelomeningocele kyphosis in the older child by kyphectomy and segmental spinal instrumentation. Spine (Phila Pa 1976) 12:37–41
Hoppenfeld S (1967) Congenital kyphosis in myelomeningocoele. J Bone Joint Surg Am 49:276–280
Hyun SJ, Jung JM (2018) Spinal deformity surgery : it becomes an essential part of neurosurgery. J Korean Neurosurg Soc 61:661–668. https://doi.org/10.3340/jkns.2018.0150
Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ (2017) Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine 14:126–132. https://doi.org/10.14245/kjs.2017.14.4.126
Kang J, Hosogane N, Ames C, Schwab F, Hart R, Burton D, Shaffrey C, Smith JS, Bess S, Lafage V, Cho K-J, Ha Y (2018) Diversity in surgical decision strategies for adult spine deformity treatment: the effects of neurosurgery or orthopedic training background and surgical experience. Neurospine 15:353–361. https://doi.org/10.14245/ns.1836086.043
Ko AL, Song K, Ellenbogen RG, Avellino AM (2007) Retrospective review of multilevel spinal fusion combined with spinal cord transection for treatment of kyphoscoliosis in pediatric myelomeningocele patients. Spine (Phila Pa 1976) 32:2493–2501. https://doi.org/10.1097/BRS.0b013e3181573b11
Kocaoglu B, Erol B, Akgulle H, Gasimov E, Yalcin S (2008) Combination of Luque instrumentation with polyaxial screws in the treatment of myelomeningocele kyphosis. J Spinal Disord Tech 21:199–204. https://doi.org/10.1097/BSD.0b013e318074e4c6
Lee BH, Hyun SJ, Han S, Jeon SI, Kim KJ, Jahng TA, Kim HJ (2018) Total deformity angular ratio as a risk factor for complications after posterior vertebral column resection surgery. J Korean Neurosurg Soc 61:723–730. https://doi.org/10.3340/jkns.2018.0125
Lindseth RE, Stelzer L Jr (1979) Vertebral excision for kyphosis in children with myelomeningocele. J Bone Joint Surg Am 61:699–704
Lintner SA, Lindseth RE (1994) Kyphotic deformity in patients who have a myelomeningocele. Operative treatment and long-term follow-up. J Bone Joint Surg Am 76:1301–1307
Martin J Jr, Kumar SJ, Guille JT, Ger D, Gibbs M (1994) Congenital kyphosis in myelomeningocele: results following operative and nonoperative treatment. J Pediatr Orthop 14:323–328
McMaster MJ (1988) The long-term results of kyphectomy and spinal stabilization in children with myelomeningocele. Spine (Phila Pa 1976) 13:417–424
Mintz LJ, Sarwark JF, Dias LS, Schafer MF (1991) The natural history of congenital kyphosis in myelomeningocele. A review of 51 children. Spine (Phila Pa 1976) 16:S348–S350
Niall DM, Dowling FE, Fogarty EE, Moore DP, Goldberg C (2004) Kyphectomy in children with myelomeningocele: a long-term outcome study. J Pediatr Orthop 24:37–44
Odent T, Arlet V, Ouellet J, Bitan F (2004) Kyphectomy in myelomeningocele with a modified Dunn-McCarthy technique followed by an anterior inlayed strut graft. Eur Spine J 13:206–212. https://doi.org/10.1007/s00586-003-0662-4
Ryabykh SO, Pavlova OM, Savin DM, Burtsev AV, Gubin AV (2018) Surgical Management of Myelomeningocele-Related Spinal Deformities. World Neurosurg 112:e431–e441. https://doi.org/10.1016/j.wneu.2018.01.058
Sharrard WJ (1968) Spinal osteotomy for congenital kyphosis in myelomeningocele. J Bone Joint Surg Br 50:466–471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wui, SH., Hyun, SJ., Kim, KJ. et al. Kyphectomy and interbody fixation using lag screws in a child with myelomeningocele kyphosis: a technical case report. Childs Nerv Syst 35, 1407–1410 (2019). https://doi.org/10.1007/s00381-019-04217-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04217-w