Abstract
Purpose
Carnitine deficiency has been found in cancer patients and has been associated with fatigue. This study aimed to explore the prevalence of carnitine deficiency in pediatric cancer patients and its relationship with fatigue and other potential contributing factors.
Methods
Children with cancer or Langerhans cell histiocytosis who were receiving treatment or had completed therapy were eligible. Patients completed the Pediatric Functional Assessment of Chronic Illness-Fatigue, the Pediatric Quality of Life Inventory Multidimensional Fatigue Scale, a numeric fatigue rating, and had carnitine levels obtained. Carnitine deficiency was defined as a total and/or free carnitine level less than normal for age or an acylcarnitine value higher than normal for age.
Results
Data from 142 children aged 8–17 were analyzed. Twenty-eight of 142 (19.7 %) had decreased total and 42.8 % (12/28) had decreased free carnitine levels. No patients had elevated acylcarnitine levels or elevated ratios. Patients with versus without carnitine deficiency differed by age (p = 0.043), treatment (p = 0.037), duration since last chemotherapy (p = 0.020), and body mass index (p = 0.010), but not fatigue, when all data were analyzed together. Yet, a negative relationship between fatigue and carnitine levels was found on a subgroup (off-therapy; fatigue worse than the norm).
Conclusion
No significant association between fatigue and carnitine level was demonstrated when data from all patients were analyzed together; however, a significant yet unexpected relationship was found for patients who completed therapy and reported elevated fatigue. Given the small sample size, these results should be interpreted with caution. Future studies to explore impact upon excessive carnitine levels are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatigue is a prevalent and concerning symptom for both adult and pediatric cancer patients and can negatively impact patients’ quality of life [1–8]. The etiology of fatigue in cancer patients is not yet well understood. Generating a better understanding of potential contributing factors is important to develop potential interventions for patients with fatigue. Carnitine is a micronutrient required for fatty acid metabolism and energy production and is available over the counter as a dietary supplement. Carnitine has been evaluated in a variety of adult conditions including cancer, chronic liver disease, multiple sclerosis, chronic fatigue syndrome, fibromyalgia, end-stage renal disease, and neuropathy [9–12]. Patients with carnitine deficiency are susceptible to the development of chronic fatigue secondary to impaired utilization of long-chain fatty acids in energy metabolism [13]. Patients with cancer are thought to be particularly at risk for carnitine deficiency due to decreased intake, increased metabolic needs, and treatment with medications that interfere with carnitine metabolism [13–16].
Several studies have evaluated levocarnitine supplementation and its impact on fatigue and other patient variables in adult cancer patients [13–16]. In 50 adult cancer patients with low plasma carnitine levels and fatigue who received levocarnitine supplementation for 1 week, restored carnitine levels and a statistically significant improvement in fatigue scores in 90 % of patients was seen [15]. Gramignano et al. reported statistically significant improvements in fatigue, quality of life, lean body mass, appetite, and perceived global health status in 12 adults with advanced cancer who received levocarnitine for 4 weeks in an open-label, nonrandomized study [16]. Cruciani et al. [13], in a phase I/II open-label trial, demonstrated that cancer patients who received levocarnitine supplementation experienced improved fatigue, mood, and sleep with a dose-dependent improvement in fatigue within the subgroup that received 7 days of supplementation and experienced a rise in carnitine-associated laboratory values (“responders”). A randomized, double-blind, placebo-controlled, parallel group study of levocarnitine supplementation in 29 adult cancer patients with moderate-severe fatigue and carnitine deficiency by the same investigators found significant improvements in fatigue, functional well-being, and performance status among patients who had been started on upfront levocarnitine treatment/supplementation [17], though analysis of the data overall failed to demonstrate significant change in fatigue for the entire group.
The few studies that have evaluated carnitine status and the potential association with fatigue and other patient-related variables in pediatric cancer patients have demonstrated varied results. Hockenberry et al. [18] studied plasma carnitine levels and fatigue in 67 pediatric patients with a diagnosis of leukemia/lymphoma or solid tumor who were chemo naive or had received prior chemotherapy, before and 1 week after receiving chemotherapy with cisplatin, ifosfamide, and/or doxorubicin. Of the 67 subjects, a significant negative correlation between fatigue and total and free carnitine levels (higher fatigue and lower carnitine levels) 1 week after chemotherapy was found in 22 adolescents who had received prior chemotherapy. Rogalidou et al. [19] evaluated serum total and free carnitine levels in 40 children with acute leukemia at various time points and concluded that the reduction in carnitine levels seen was not correlated with age, sex, nutritional status, and leukemia risk group or hemoglobin level. Yaris et al. [20] examined the relationship between serum total carnitine levels and nutritional status in 51 children (ages 3–16.5 years at diagnosis) with lymphoma or solid tumor at diagnosis and 3 months after initiation of treatment. They found that the decrease in serum total carnitine levels noted from diagnosis to 3 months after diagnosis was independent of the patient’s nutritional status.
Generalization of results from the studies mentioned above has been limited due to small samples, variation in patient diagnosis, treatment received, and carnitine sampling time points. To further understand the potential impact of carnitine deficiency in pediatric cancer patients, this study aimed to estimate the prevalence of carnitine deficiency in children with cancer via recruiting children with a variety of cancer diagnoses and treatment regimens. We also explored the relationship between carnitine deficiency and fatigue as well as other potential contributing factors. Results from this study could expand the knowledge of the relationship between carnitine status and fatigue and its potential impact on clinical practice.
Methods
The study was approved by the hospital’s Institutional Review Board and the Scientific Review Committee of Robert H. Lurie Comprehensive Cancer Center at Northwestern University. Informed consent, and assent where applicable, was obtained prior to participation.
Sample and procedures
A total of 150 patients, 8 to 18 years of age with cancer or Langerhans cell histiocytosis were recruited from Ann and Robert H. Lurie Children’s Hospital of Chicago (formerly Children’s Memorial Hospital, Chicago). Inclusion criteria were as follows: (1) treatment duration of at least 1 month or completion of therapy within the previous 5 years; (2) a Lansky or Karnofsky performance score of ≥50; (3) ability to read and understand English; (4) no evidence of cognitive dysfunction that would limit the ability to report fatigue in the investigator’s opinion; and (5) patients treated with stem cell transplantation were eligible if they were pre-transplant (prior to conditioning) or greater than 100 days post-transplant. Exclusion criteria included the following: (1) use of oral levocarnitine, a nutritional supplement containing carnitine or treatment with total parenteral nutrition containing levocarnitine within the previous 2 weeks; (2) antineoplastic treatment with surgery only; (3) pregnant or lactating females; and (4) recent participation on a therapeutic fatigue study. Patients who were receiving treatment and those who had completed therapy at the time of study participation were grouped into “on-therapy” and “off-therapy,” respectively, in the analysis.
Patients completed two validated fatigue scales, pediatric Functional Assessment of Chronic Illness Therapy-Fatigue (pedsFACIT-F) [21] and The Pediatric Quality of Life Inventory Multidimensional Fatigue Scale (MFS) [22], during their clinic visit. The pedsFACIT-F consists of 11 items and measures fatigue in the past 7 days utilizing a five-point Likert rating scale. Using raw scores, the maximum score for this survey instrument is 44 with higher scores representing more severe fatigue. The minimally important difference was 4.7, estimated using clinical anchors of anemic status and functional performance ratings. The previously established general population norm for the pedsFACIT-F score was 7.8 with a standard deviation (SD) of 9.6. The MFS consists of three subscales of six items each including general fatigue, sleep/rest fatigue, and cognitive fatigue using a five-point rating scale. The items were reverse-scored and transformed to a 0–100 scale with lower scores indicating more fatigue. The mean scores (SD) of a sample of 52 healthy children, ages 5 to 18, have been previously reported and are as follows: 80.49 (13.33) for total score, 85.34 (14.95) for general subscale, 75.00 (18.76) for sleep/rest subscale, and 81.14 (17.43) for cognitive subscale. Additionally, patients were asked to rate their fatigue using age-appropriate National Comprehensive Cancer Network (NCCN) fatigue screening: 1–5 rating (1 = absence of fatigue, 5 = severe fatigue; for patients aged ≤12 years) and a 0–10 rating (0 = no fatigue, 1–3 = mild fatigue, 4–6 = moderate fatigue, 7–10 = severe fatigue; for patients aged >12 years) [23]. Blood samples were obtained on the same day, or within 48 h, of completion of fatigue measures for evaluation of carnitine status, in which carnitine deficiency was defined as a total and/or free carnitine level less than normal for age or an acylcarnitine value higher than normal for age. Plasma concentrations of free and total carnitine levels were measured by high-performance liquid chromatography tandem mass spectrometry. Acylcarnitine levels were calculated as the difference between total carnitine and free carnitine. The acylcarnitine to free carnitine ratio was also calculated. Normal levels for total carnitine/free carnitine/acylcarnitine are 28–83/22–66/3–32, 34–77/22–65/4–29, and 34–78/25–54/5–30 μmol/L for patients with ages 7–10, 11–17, and ≥18 years, respectively.
Statistical analysis
Descriptive statistics were used to calculate NCCN fatigue rating, pedsFACIT-F, MFS subscale and total scores, and carnitine and acylcarnitine levels. Patients who were receiving treatment (on-therapy) and those who had completed therapy (off-therapy) at the time of study participation were compared across covariates using t tests and chi-squared tests. Covariates analyzed included age, sex, race, diagnosis group, treatment received, recent treatment, BMI, performance status, hemoglobin level, albumin level, comorbid conditions, hospitalizations, and home medications (see Table 1). t Tests were performed to compare mean fatigue scores by therapy status.
To determine the prevalence of carnitine deficiency, proportions and 95 % confidence intervals using exact binomial methods were used to analyze the entire sample and patients by treatment status (on- vs off-therapy). t Tests and chi-squared tests were used to analyze the relationship between carnitine status (normal vs deficiency) and fatigue and other selected covariates. For both pedsFACIT-F and MFS, missing responses were replaced by the mean of the completed items if more than 50 % of the items were answered. If more than 50 % of the items were missing, the fatigue score was not computed and the patient was excluded from data analysis. Data analyses were conducted using SAS software (version 9.3; SAS Institute Inc., Cary, NC).
Results
Sample
A total of 148 pediatric cancer patients were enrolled during the study period from January 2011 to January 2012. Of these 148, 6 were excluded from analysis due to lack of carnitine testing (n = 4) or fatigue measures (n = 2). Of the 142 patients being analyzed, 80 (56 %) were on-therapy and 62 (44 %) were off-therapy. On- and off-therapy patients differed significantly by age (p = 0.026), diagnosis (p = 0.014), treatment (p = 0.003), treatment duration (p = 0.024), hospitalizations (p < 0.001), infections (p = 0.005), home medication usage (p < 0.001), chemotherapy agents (vinca alkaloids, p = 0.029), days since last chemotherapy (p < 0.001), and hemoglobin (p < 0.001) and albumin (p = 0.039) levels (see Table 1).
The means (SD) for total carnitine, free carnitine, acylcarnitine, and acyl/free carnitine ratio were 40.98 μmol/L (10.86), 34.09 μmol/L (9.97), 6.90 μmol/L (3.05), and 0.21 (0.11), respectively. On- and off-therapy patients had significantly different total carnitine levels (p = 0.046) (see Table 2). Twenty percent of sample (n = 28; 20 %) met the criterion of carnitine deficiency defined by the current study; specifically, 22.5 % (18 of 80) of on-therapy and 16.1 % (10 of 62) off-therapy patients had carnitine deficiency. All 28 patients had a decreased total carnitine level; 43 % had a decreased free carnitine level, yet none had an elevated acylcarnitine level or an elevated acyl/free carnitine ratio. Given no patients had an elevated acylcarnitine level or acyl/free carnitine ratio, these variables were not further analyzed. When compared by therapy status, 23 % on-therapy patients and 16 % off-therapy patients had decreased total carnitine levels (p = 0.34). In addition, 13 % on-therapy patients and 3 % off-therapy patients had decreased free carnitine levels (p = 0.05). The median duration of therapy was 431 days (range 28–1474 days) for on-therapy patients with decreased carnitine levels.
Carnitine status (normal vs deficiency) was significantly (p < 0.05) associated with age, type of treatment received, time since last chemotherapy, and BMI (see Table 3). Patients with decreased carnitine levels were older (p = 0.04), received combination therapy with chemotherapy/radiation/surgery, and chemotherapy/radiation/stem cell transplantation (p = 0.04), shorter time since last chemotherapy (p = 0.02), and lower BMI index (p = 0.01). When patients were classified into anemic status (anemic = 48; nonanemic = 93) using hemoglobin values adjusted by age and gender, no significant relationship between anemic status and carnitine deficiency was found (p = 0.27).
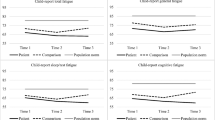
More than 50 % of patients reported worse fatigue than the average fatigue scores reported by the US pediatric general population with 56.3 and 71.8 % as measured by pedsFACIT-F and MFS, respectively. As shown in Table 4, on-therapy patients reported more severe fatigue than off-therapy patients when fatigue was measured by using the NCCN score (8–12 years old; p = 0.01), pedsFACIT-F (p = 0.03), and two MFS subdomains (general fatigue, p = 0.03, and sleep, p = 0.01). There was no statistically significant difference in fatigue scores between patients with normal versus abnormal carnitine levels across all fatigue scales (Table 5). Scatter plots between free and total carnitine levels versus pedsFACIT-Fatigue and MFS are shown in Fig. 1, in which negligible Spearman’s rho was found with rho close to zero on all comparisons. We further evaluated the relationship between fatigue and carnitine levels in those who reported worse fatigue scores than the general population mean. Since only 19 on-therapy patients had a MFS score worse than the general population norm, we did not report the correlation in this subset. For pedsFACIT-F, a significant Spearman’s rho was found for patients who were off-therapy (n = 29), rho = 0.44 (p = 0.016), and 0.42 (p = 0.023) for total carnitine and free carnitine levels, respectively. Yet, no significant relationship (p < 0.5) was found for other comparisons. When patients were grouped into no/mild fatigue (n = 60; 38.6 %) and moderate/severe fatigue (n = 44; 38.6 %) using the NCCN single fatigue rating, it was found that patients with carnitine deficiency tended to report moderate/severe fatigue (n = 18; 66.8 %) rather than no/mild fatigue (n = 9; 33.3 %), p = 0.05.
Discussion
This cross-sectional study evaluated the prevalence of carnitine deficiency in children with cancer and explored the relationship between carnitine status and fatigue and other potentially influential factors. Results of this study showed 20 % of patients met the carnitine deficiency criteria defined by the current study, including patients who were off-therapy. For on-therapy patients, the duration of treatment ranged from approximately 1 month to 4 years with a mean of 395 total days of therapy. For off-therapy with carnitine deficiency, the duration since completion of therapy ranged from about 5 months to 2.5 years with a median of 340 days. These findings suggest that patients can develop carnitine deficiency at any stage of the treatment continuum.
Rogalidou et al. [19] found a statistically significant decline in total and free serum carnitine levels from at diagnosis to 1 year after treatment and a significant increase in levels between the end of treatment and months to years after completion of therapy for children with ALL. Specifically, abnormally low levels of free carnitine were found with 22.5, 48.7, 34.2, and 6.3 % of patients at diagnosis, 1 year of therapy, end of therapy, and months to years after completion of treatment, respectively. Total carnitine levels less than normal for age were seen in 32.5, 56.4, 42.1, and 25 % at the respective time points [19]. In contrast, in our patient sample, fewer patients had abnormal free (total) carnitine values, 12.5 % (22.5 %) and 3.2 % (16.1 %) for on- and off-therapy patients, respectively. We hypothesize that differences in study design, sample size (n = 40 vs 144) and types of cancer (acute leukemia vs all cancer types) might contribute to the difference in results. A larger scale epidemiology study should be conducted to understand the prevalence of carnitine deficiency across the treatment continuum, from diagnosis to long-term survivorship. This could aid in understanding some of the short and long-term treatment effects experienced by childhood cancer patients. Regardless of the relationship between carnitine deficiency and fatigue, investigators pointed out that patients could have carnitine deficiency months to years after completion of treatment, and metabolic profiling of asymptomatic childhood cancer survivors revealed significantly lower plasma carnitine levels in individuals with cardiac dysfunction than those with normal function [24].
In the current study, significant relationships were found between carnitine deficiency versus age, types of treatment, time since last chemotheraphy, and BMI. We did not find significant relationship between carnitine deficiency and fatigue when data from all patients were analyzed together. When analyzing patient subgroups based on therapy status (on- vs off-therapy) and fatigue severity (worse vs better than norms), we found a moderate rho (rho = 0.4) between fatigue and carnitine for off-therapy patients who reported more severe fatigue, however, in a different direction to that reported by Hockenberry et al. [18]. It was noted that our sample had lower averaged free carnitine and total carnitine values than patients included in Hockenberry’s study. We suspected that excessive carnitine levels might also contribute to self-reported fatigue. Given the small sample size (n = 29) in this subgroup of the current study (off-therapy; worse fatigue than the norm), future studies should be conducted to evaluate whether this finding could be replicated. Additionally, investigators might want to pay attention to the impact of excessive carnitine levels and further define normal ranges of carnitine levels and not just focus on a single cutoff value. In contrast to prior studies, in order to maximize generalizability of the results, we did not limit patient inclusion criteria to those who received certain chemotherapy agents and instead, we recruited patients who were at various stages along the treatment continuum and had received various treatments, which also resulted in small percentage of patients meeting the carnitine deficiency criteria and further decreased the statistical power.
There are several limitations to this study. There was no control group for comparison. Although this is one of the largest evaluations of carnitine status in pediatric cancer patients to date, the sample size is still relatively small. While efforts were made to control for other factors, such as psychiatric diagnoses and comorbid conditions, which could contribute to fatigue, this information was assessed through review of the medical record and therefore may not be entirely representative as some patients may have undiagnosed or unreported conditions. Furthermore, fatigue is often associated with other symptoms including pain, nausea/vomiting, and sleep disturbances which were not assessed in this study, which we plan to include in future studies. In this study, we did not find significantly different carnitine deficiency levels between on- and off-therapy patients who received emetogenic chemotherapy. We speculated that nutritional status might play a critical role. Nutritional status was assessed using albumin, weight, height, and BMI which may not be the most accurate representation of patient nutritional status. Different eating habits among individuals (e.g., children vs adolescents, females vs males) can influence their particular food types that increase the availability of carnitine in the diet. Our future trial would closely monitor patients’ eating habits and nutritional intake allowing for further exploration of correlations with carnitine and fatigue. Furthermore, obtaining urine carnitine levels may provide additional information regarding carnitine metabolism and status in pediatric cancer patients. Additional information could also be gained by prospectively following larger numbers of patients at multiple time points during their care including diagnosis, through treatment and during long-term follow-up.
In summary, in this cross-sectional study, we aimed to explore the prevalence of carnitine deficiency in children with cancer. About 20 % of patients had carnitine deficiency regardless of treatment status. Age, type of treatment received, time since last chemotherapy treatment, and BMI were found to be related to carnitine deficiency. No significant association between fatigue and carnitine level was demonstrated when data from all patients were analyzed together; however, a significant yet unexpected relationship was found for patients who completed therapy and reported more severe fatigue than the general population norm. Given the small sample size, these results should be interpreted with caution. Future studies to explore impact upon excessive carnitine levels are warranted.
References
Henry D, Viswanathan HN, Elkin E, Traina S, Wade S, Cella D (2008) Symptoms and treatment burden associated with cancer treatment: results from a cross-sectional national survey in the U.S. Support Care Cancer 16:791–801
Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR (2007) Cancer-related fatigue: the scale of the problem. Oncologist 12:4–10
Minton O, Richardson A, Sharpe M, Hotopf M, Stone P (2008) A systematic review and meta-analysis of the pharmacological treatment of cancer-related fatigue. J Natl Cancer Inst 100:1155–1166
Morrow GR (2007) Cancer-related fatigue: causes, consequences, and management. Oncologist 12:1–3
Ryan JL, Carroll JK, Ryan EP, Mustian KM, Fiscella K, Morrow GR (2007) Mechanisms of cancer-related fatigue. Oncologist 12:22–34
Perdikaris P, Merkouris A, Patiraki E, Tsoumakas K, Vasilatou-Kosmidis E, Matziou V (2009) Evaluating cancer related fatigue during treatment according to children’s, adolescents’ and parents’ perspectives in a sample of Greek young patients. Eur J Oncol Nurs 13:399–408
Dupuis LL, Milne-Wren C, Cassidy M, Barrera M, Portwine C, Johnston DL, Silva MP, Sibbald C, Leaker M, Routh S (2010) Symptom assessment in children receiving cancer therapy: the parents’ perspective. Support Care Cancer 18:281–299
Collins JJ, Byrnes ME, Dunkel IJ, Lapin J, Nadel T, Thaler HT, Polyak T, Rapkin B, Portenoy RK (2000) The measurement of symptoms in children with cancer. J Pain Symptom Manag 19:363–377
Hedayati SS (2006) Dialysis-related carnitine disorder. Semin Dial 19:323–328
Malaguarnera M (2012) Carnitine derivatives: clinical usefulness. Curr Opin Gastroenterol 28:166–176
Reuter S, Evans A (2011) Long-chain acylcarnitine deficiency in patients with chronic fatigue syndrome. Potential involvement of altered carnitine palmitoyltransferase-I activity. J Intern Med 270:76–84
Tejani A, Wasdell M, Spiwak R, Rowell G, Nathwani S (2011) Carnitine for fatigue in multiple sclerosis. Cochrane Database Syst Rev 5:CD007280–CD007280
Cruciani RA, Dvorkin E, Homel P, Malamud S, Culliney B, Lapin J, Portenoy RK, Esteban-Cruciani N (2006) Safety, tolerability and symptom outcomes associated with L-carnitine supplementation in patients with cancer, fatigue, and carnitine deficiency: a phase I/II study. J Pain Symptom Manag 32:551–559
Cruciani R, Dvorkin E, Homel P, Culliney B, Malamud S, Shaiova L, Fleishman S, Lapin J, Klein E, Lesage P (2004) l-carnitine supplementation for the treatment of fatigue and depressed mood in cancer patients with carnitine deficiency: a preliminary analysis. Ann N Y Acad Sci 1033:168–176
Graziano F, Bisonni R, Catalano V, Silva R, Rovidati S, Mencarini E, Ferraro B, Canestrari F, Baldelli AM, De Gaetano A, Giordani P, Testa E, Lai V (2002) Potential role of levocarnitine supplementation for the treatment of chemotherapy-induced fatigue in non-anaemic cancer patients. Br J Cancer 86:1854–1857
Gramignano G, Lusso MR, Madeddu C, Massa E, Serpe R, Deiana L, Lamonica G, Dessì M, Spiga C, Astara G (2006) Efficacy of l-carnitine administration on fatigue, nutritional status, oxidative stress, and related quality of life in 12 advanced cancer patients undergoing anticancer therapy. Nutrition 22:136–145
Cruciani RA, Dvorkin E, Homel P, Culliney B, Malamud S, Lapin J, Portenoy RK, Esteban-Cruciani N (2009) L-carnitine supplementation in patients with advanced cancer and carnitine deficiency: a double-blind, placebo-controlled study. J Pain Symptom Manag 37:622–631
Hockenberry MJ, Hooke MC, Gregurich M, McCarthy K (2009) Carnitine plasma levels and fatigue in children/adolescents receiving cisplatin, ifosfamide, or doxorubicin. J Pediatr Hematol Oncol 31:664–669
Rogalidou M, Evangeliou A, Stiakaki E, Giahnakis E, Kalmanti M (2010) Serum carnitine levels in childhood leukemia. J Pediatr Hematol Oncol 32:e61–e69
Yaris N, Akyüz C, Coskun T, Büyükpamukçu M (2002) Serum carnitine levels of pediatric cancer patients. Pediatr Hematol Oncol 19:1–8
Lai JS, Cella D, Kupst MJ, Holm S, Kelly ME, Bode RK, Goldman S (2007) Measuring fatigue for children with cancer: development and validation of the pediatric functional assessment of chronic illness therapy-fatigue (pedsFACIT-F). J Pediatr Hematol Oncol 29:471–479
Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P (2002) The PedsQL in pediatric cancer: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module. Cancer 94:2090–2106
National Comprehensive Cancer Network (2010) NCCN Practice Guildlines in Oncology: Cancer-Related Fatigue v.1. www.nccn.org Accessed Date Accessed 2010 Accessed
Armenian SH, Gelehrter SK, Vase T, Venkatramani R, Landier W, Wilson KD, Herrera C, Reichman L, Menteer J-D, Mascarenhas L (2014) Carnitine and cardiac dysfunction in childhood cancer survivors treated with anthracyclines. Cancer Epidemiol Biomark Prev 23:1109–1114
Acknowledgments
Dr. Haertling’s efforts were supported by a grant from the SurvivorVision when she was on fellowship at Ann & Robert H. Lurie Children’s Hospital of Chicago. We also thank Kara Halligan, RN, for her assistance in patient recruitment and enrollment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare that no conflict of interest exists.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding source
Dr. Haertling’s efforts were supported by a grant from the SurvivorVision when she was on fellowship at Ann & Robert H. Lurie Children’s Hospital of Chicago.
Electronic Supplementary Material
ESM 1
(DOC 303 kb)
Rights and permissions
About this article
Cite this article
Lai, JS., Haertling, T., Weinstein, J. et al. A cross-sectional study of carnitine deficiency and fatigue in pediatric cancer patients. Childs Nerv Syst 32, 475–483 (2016). https://doi.org/10.1007/s00381-015-2983-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2983-0