Abstract
Purpose
Previous small studies have demonstrated that seizure outcomes following surgery for extratemporal lobe epilepsy (ETLE) in children are worse than those for temporal lobe epilepsy. We have conducted a meta-analysis of the available literature to better understand ETLE surgical outcomes in children.
Methods
We searched PubMed (1990–2009) for appropriate studies using the following terms: ETLE, ETLE surgery, ETLE surgery outcome, frontal lobe epilepsy, occipital lobe epilepsy, and parietal lobe epilepsy. Our collected data included patient age at seizure onset and surgery, the cerebral lobe involved with epileptogenesis, MRI findings, predominant seizure semiology, intracranial monitoring use (electrode implantation), epileptic region histopathology, and postoperative seizure outcome. Statistical analysis was performed to determine associations among these variables and postoperative outcome.
Results
Ninety-five patients from 17 studies satisfied the inclusion criteria. Pathological findings (p = 0.039) and seizure type (p = 0.025) were significantly associated with outcome: A larger proportion of patients with cortical dysplasia and complex partial seizures experienced better outcomes. Age at surgery (p = 0.073) and the cerebral resection site (p = 0.059) were marginally associated with seizure outcome.
Conclusions
This study confirms previous reports: Surgical outcomes for ETLE epilepsy are significantly worse than those for temporal lobe epilepsy. The reasons for this difference may include the diffuse nature of the pathology involved in ETLE, difficulty in localizing the seizure focus in young children, and involvement of “eloquent” nonresectable cortex in epileptogenesis. Because of the reporting variability among different epilepsy centers, more uniform protocols are necessary for fair evaluation and comparison of outcomes among the different centers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epilepsy in children is commonly the result of a congenital malformation of the cerebral cortex. Epilepsy in adults, in contrast, is usually due to neoplasm, injury, or other type of acquired cortical abnormality. Extratemporal lobe epilepsy (ETLE) is more commonly seen in children [1–3], consistent with the congenital nature of the extratemporal epileptic foci. Siegel et al. [4] have suggested that this is due to the progression of cortical maturation, which begins in the central part of the brain, so any congenital deformities become apparent in the extratemporal areas first. Epileptic foci in adults, on the other hand, are typically acquired and located in the temporal lobe [5]. In general, patients with ETLE, both children and adults, have worse postoperative outcomes than the patients with temporal lobe epilepsy (TLE) because the frontal, parietal, and occipital lobes contain areas for speech, sensorimotor processing, visual processing, and other “higher functions” that can become involved in epileptogenesis. Since these important cortical regions must be spared, completely removing a focus in ETLE is often impossible [6]. In contrast, surgical resection in the temporal lobe may be completed with more favorable outcomes [7]. This analysis considers the postoperative seizure outcomes of children with ETLE without lesions.
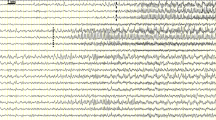
ETLE can be difficult to treat, in part, because localizing the epileptogenic focus to a specific resectable cerebral region is difficult. Certain seizure foci may be difficult (if not impossible) to localize by surface electroencephalograph (EEG) recording. In 1998, Westmoreland [8] demonstrated that certain frontal lobe foci show no evidence of EEG change. Furthermore, the seizures that begin outside the temporal lobe can quickly propagate to other parts of the brain, further complicating seizure focus localization [6]. It may be possible to estimate the location of seizure focus by careful observation of the semiology and progression of the seizure [9, 10]; however, the exact localization of seizure focus may be difficult in young children due to their inability to tolerate intracranial monitoring studies through implanting intracranial electrodes.
Each previously reported study related to ETLE surgery in children describes a small number of patients and their surgical outcomes. The authors, therefore, have conducted a meta-analysis of the available literature regarding ETLE surgery in children to gain a better understanding of these outcomes. The primary concern in this study is to determine which of the preoperative variables under consideration is strongly associated with postoperative seizure outcome in children.
Patients and methods
We collected data from previously reported studies in English literature conducted on the surgical outcome of ETLE in children (aged 17 years or younger). PubMed searches were used to identify relevant papers with the following search terms: ETLE, ETLE surgery, ETLE surgery outcome, frontal lobe epilepsy, occipital lobe epilepsy, and parietal lobe epilepsy. The bibliographies of these papers were then searched individually to find additional relevant studies. Some of the discovered studies included clinical outcome on both adults and children; the data related to children were extracted individually in these studies.
All accessible studies published after 1990 were reviewed. The year 1990 was chosen because most studies published after that year included magnetic resonance imaging (MRI) findings, essential for this analysis. To be included in this study, all patients had at least 1 year follow-up. Some of the studies did not define seizure outcome in terms of the Engel system; in each of these cases, the given definition of each outcome class was translated into the Engel system for use in this analysis. Studies that included only a summary of demographic information without mentioning the outcome related to the individual patient were excluded, so that individual variables could be considered for each patient.
Children with nonlesional epilepsy, including cortical dysplasia with an extratemporal focus, were included. Multilobar foci that included the temporal lobe were included, but purely temporal lobe foci were excluded. “Lesion” was defined not by MRI findings but on the basis of histopathological results. Patients with tumors, vascular lesions, multiple sclerosis, and heterotopias were excluded. We included the patients with the following histopathological diagnosis: cortical dysplasia, gliosis, inflammation, polymicrogyria/ulegyria, neuronal loss, and “normal.” A large subset of pediatric patients in these studies underwent hemispherectomy; this population was not considered to be a part of the nonlesional ETLE population and was excluded from our analysis. This procedure circumvents the classical dilemma related to exact seizure focus localization and ETLE surgery: to remove the epileptogenic focus while sparing as much of the surrounding eloquent cortex as possible. All the other types of surgical procedures, such as lobectomy, topectomy, focal resection, and multiple subpial transection, were considered.
Data for these patients were extracted from 15 [11–25] case series and two [26, 27] case reports. All studies were retrospective. They often included both pediatric and adult patients. In those studies that included all age groups, the information regarding pediatric patients was extracted and included in our analysis. Specific types of data collected were the following: age of seizure/surgery, duration of epilepsy, outcome class (as defined by the Engel classification system) [28], histopathological findings, predominant seizure semiology (classified as simple partial, complex partial, generalized, or infantile spasms), location of focus (lobe of brain), surgery type/location, lateralization, MRI findings, and whether or not the patient underwent intracranial monitoring through electrode implantation.
The relationships between the preoperative variables and seizure outcomes were analyzed using R (version 2.4.1, Vienna, Austria). Each variable was compared to outcome individually to determine if there was a significant association between the variable and outcome (specifically, seizure freedom). Continuous variables (age of onset/surgery and duration of epilepsy) were summarized using mean and standard deviation and were compared across groups using ANOVA. Categorical variables were summarized using frequency and percentage and were compared using Fisher’s exact test (Table 1).
Results
Overall seizure outcome
There were 95 patients who satisfied the above inclusion criteria and were included in this study. Of these patients, 32 (33.7%) had Engel class I outcome or complete seizure freedom; 14 patients (14.7%) had Engel class II outcome (<90% seizure reduction or freedom with medication), 24 (25.3%) had Engel III (>75% seizure reduction), and 25 (26.3%) had Engel IV or no worthwhile improvement. Combining the patients in classes I, II, and III, 70 (73.7%) of the patients had a worthwhile reduction in seizure frequency, while 25 (26.3%) did not benefit from surgery.
Preoperative factors related to surgical outcome
The mean age of seizure onset for the study group was 4.5 ± 3.6 years. This variable was not associated with seizure outcome (p = 0.505). The mean duration of epilepsy was 6.4 ± 4.2 years and similarly was not associated with postoperative outcome (p = 0.292). The mean age at the time of surgery for the study group was 9.6 ± 5.6 years. The association between age at surgery and outcome was found to be marginally significant (p = 0.073). Some patients did not have data points for every variable. In these cases, only those patients with the available data for a given variable were included in the final analysis.
Seizure semiology was classified as complex partial (CPS), generalized (GS), infantile spasms (IS), and “other,” which included simple partial seizures and mixed-type seizures. Sixty-five of the 95 patients had information available regarding their seizure type. A significant association was found between seizure semiology and outcome class (p = 0.025). Of those patients in this group who had an Engle class I outcome (n = 28), 14 (50%) experienced CPS, nine (32.1%) experienced GS, four (14.3%) had IS, and one (3.6%) had “other” types of seizures.
Histopathology data were available for every patient but one. Pathological results were divided into three categories for analysis: cortical dysplasia (CD), gliosis, and “other.” The “other” category included neuronal loss, encephalitis, polymicrogyria, ulegyria, chronic inflammation, and “normal.” A significant association was found between histopathology and outcome class (p = 0.039). Notably, in the class I group (n = 27), 18 (66.7%) of the patients had CD, nine (33.3%) had gliosis, and no patient fits into the “other” category.
To increase the number of patients in the categories analyzed, the types of surgery performed to remove the epileptic focus were divided into frontal resections (including frontal total/partial lobectomy), posterior cortical resections (parietal and occipital partial/total lobectomy), and “other” (includes central/multilobar resections and multiple subpial transection). The association between surgery type and outcome class was found to be marginally significant (p = 0.059) with the patients undergoing surgery in the posterior cortical regions enjoying better outcomes. Seventy-six of the 95 patients in the study had available data regarding the type of surgery. Among these patients, 21 (27.6%) had Engel class I outcome, 12 (15.8%) had class II outcome, 20 (26.3%) had class III, and 23 (30.3%) had class IV outcome. Among those patients who had class I outcome, nine (42.9%) underwent frontal lobe surgery, nine (42.9%) underwent posterior cortical surgery, and three (14.3%) underwent “other” surgeries.
Lateralization of the seizures had no association with seizure outcome (p = 0.976). One patient had a bilateral focus, and this patient was in Engel class III with respect to seizure frequency postoperatively. The rest of the patients were evenly distributed among the four classes and hemispheres (see Table 1). Abnormal MRI findings also had no significant association with seizure outcome (p = 0.902). Finally, the use of intracranial monitoring had no association with seizure outcome (p = 0.124), with a largely even distribution of patients among the four classes.
Discussion
The diagnosis of ETLE and its surgical treatment requires a multidisciplinary comprehensive preoperative evaluation. The history should include careful documentation of ictal behavior, which may, in some cases, help to localize the epileptogenic focus to a particular lobe or region of the brain (this may prove difficult in infants). In addition to providing valuable localizing information, seizure semiology may be a significant predictor of postoperative outcome. As shown by our data, there is a significant association between seizure type and outcome class: More patients with complex partial seizures experienced an Engel class I outcome. The young child with a developing and quite plastic cortex is very vulnerable to generalized seizures. Over the course of many years, repeated generalized seizures can be a significant detriment to normal cognitive development and involve more cortical regions in seizure generation, resulting in worse outcomes.
The next step in the diagnosis of ETLE is to perform neuroimaging, including functional imaging studies [MRI, positron emission tomography (PET), and single photon emission computed tomography (SPECT), the latter two typically performed ictally and interictally]. PET and SPECT scans may show hypermetabolism or hypoperfusion at the region of the seizure focus [16, 29]. Our analysis found that the presence of a structural abnormality on MRI did not have an association with postoperative seizure outcome. This finding may be due to the nature of malformation of cortical development such as cortical dysplasia; the affected brain tissue often extends beyond the visible MRI abnormality [23].
Some patients may require intracranial EEG monitoring, which is typically used when the imaging, history, and scalp EEG do not point to a specific focus [30]. Centeno and colleagues [31] report little value in intracranial monitoring in infants and very young children since the cortex is not well-developed to allow for the precise localization of seizure focus. Since the seizure foci of the patients who undergo intracranial EEG monitoring cannot be localized by noninvasive means, these patients may or may not be destined for a worse outcome regardless of the type of monitoring used [31, 32]. The data reviewed does not ascribe any significance to the use of intracranial monitoring as a predictor of outcome.
The treatment of both temporal and extratemporal epilepsy begins with a trial of antiepileptic drug therapy. Usually multiple drugs are tried for a period of up to 2 years before the surgical option is entertained [33, 34]. Although earlier surgery may be beneficial, our data support no significant association between the duration of epilepsy and postoperative seizure outcome. One of the interesting findings in childhood epilepsy that is not observed in adult epilepsy is spontaneous remission of seizures with cortical maturation [30, 33]. As such, caution should be exercised in pursuing an aggressive course of surgical treatment for every patient with a difficult-to-localize focus. Indeed, Huttenlocher [35] warned that immediate surgical recourse may not be warranted. This particular study, however, compared the outcomes of children with regard to intelligence scores and found that children with near-normal or normal intelligence had the highest rates of spontaneous remission. It did not characterize the type of epilepsy by syndromes in each group. Such benign epilepsies include Rolandic epilepsy, Panayiotopoulos syndrome, and idiopathic childhood occipital epilepsy of Gastaut, among others. These seizure disorders are often self-limiting and require no surgical intervention [36].
When the surgical option is pursued, the location of the surgery (and by extension, the location of the epileptic focus) may have some predictive value with regard to the seizure outcome after the operation. Although statistical significance was not attained, the trend in the data show that children who undergo surgery of the frontal lobe tend to have worse outcomes, whereas children who undergo surgery of the posterior cerebral cortex may fair better. This finding echoes that of Elsharkawy and colleagues [37]. In children, this association is likely observed because the frontal lobe is relatively immature compared to the posterior cortices and may be more vulnerable to repeated seizure activity and the development of multifocal seizures.
Several groups have established that ETLE surgery has a significantly worse outcome than that of TLE surgery [6, 37–41]. Whereas children with TLE have favorable outcomes (Engel I or II) at a rate of 75%, ETLE patients may experience such outcomes at a rate of 50% [30]. Our analysis shows an even lower seizure freedom rate (33.7%). ETLE outcomes may be poor primarily because of the pathology involved in the disease. The pathology is generally widespread, congenital, and often involves eloquent cortex, whereas TLE is usually associated with mainly temporal lobe involvement and is more amenable to aggressive resection [3, 5]. Our data demonstrate that a positive histopathological finding has a favorable association with postoperative outcome. Specifically, a majority of patients in the Engel outcome class I group harbored cortical dysplasia. Dysplastic cortex is more likely to be identified against normal cortex intraoperatively as compared to neuronal loss, polymicrogyria, and inflammation. However, the diffuse nature of the focus, a result of maturation of the cortex beginning in the central area of the brain (the area most commonly involved with dysplastic cortex) [4], often leads to subtotal resection. Other investigators have also found more favorable outcomes among patients with structural abnormalities [4, 13, 31, 42]. Elsharkawy and colleagues [40] demonstrated that, among ETLE patients, those with malformations of cortical development (MCD or no focal lesion) have a 33.3% chance of seizure-free outcome, whereas the patients with neoplasms have a 56% rate.
Improving the outcomes in ETLE surgery has proven a difficult task. Although several suggestions have been advocated, no strong evidence supports a particular approach. Some groups have claimed the duration of epilepsy as a significant predictor of seizure outcome [3, 4, 43]. The reasoning behind this argument is that, in children, the cortex can recover more readily from more aggressive resection otherwise not well-tolerated later in life. However, Fogarasi and coworkers [44] have contradicted this claim. Fogarasi’s finding is supported by our data: The patients with class I outcomes had the highest mean age at surgery, this association was marginally significant (p = 0.073). It is possible that with progressive development of the cerebral cortex, the seizures focus “matures” and is more “focal” and, therefore, amenable to focal resection.
In order to improve surgical outcomes from ETLE surgery, multiple methods and techniques have been proposed. Bauman and others have suggested resection of seizure focus in multiple stages, particularly among the patients whose seizure focus prove difficult to localize or resides close to the eloquent cortex. These authors claimed seizure freedom in 60% of patients, with 50% of the patients improving over baseline after the second procedure [13]. Shukla and colleagues [41] suggested that careful selection of the patients for surgery is the best way to improve outcomes. Others have proposed that seizure freedom should not be considered as the only endpoint for ETLE surgery [34, 45, 46]. These studies base such reasoning on the fact that ETLE surgical outcomes are already poor, so the focus of treatment should be on improving patients’ quality of life by reducing seizure frequency rather than eliminating seizures. However, even these studies disclosed that patients who are seizure free have a better quality of life than the patients whose seizures persist in any form after surgery [37, 47]. Therefore, we believe that seizure freedom should remain the goal of epilepsy surgery, while diagnostic and surgical techniques should be developed and improved to increase the proportion of patients who become (and remain) seizure free.
Most importantly, there is a marked lack of uniformity among epilepsy centers regarding how patients are evaluated preoperatively and treated operatively. The methods of reporting are diverse. These deficiencies prevent fair comparison of the various treatment paradigms across different centers. Many studies do not report the data that are required to understand their treatment paradigm in an effort to work toward more desirable outcomes. Basic data such as the use of intracranial monitoring, location of the seizure focus, and age of the patient at surgery and at seizure onset were missing in some of the studies included in the present meta-analysis. The development of more uniform protocols for preoperative evaluation and reporting will allow for the collection of the data that can be used to compare outcomes from different treatment paradigms and ultimately improve outcomes in this population.
This meta-analysis is limited by its constituent studies, namely, by their small sample size. Each individual study was usually the experience of one center and often contained no more than 20 patients without a non-surgical control group. One study that did have a control group found that 21% of the patients on a medical course of treatment achieved seizure freedom [48]. This study, however, did not randomize patients to each treatment option. The patients in the study were taken from the population that was deemed unfit for surgery, and this likely resulted in the introduction of a selection bias. The inclusion of studies with adequate data in our analysis is also another source of selection bias. Several studies with relatively large number of patients had to be excluded since the clinical details related to the individual patients were not available.
Conclusions
This meta-analysis confirms the findings of previous studies that outcomes of ETLE surgery in the patients without lesions are poor. Factors significantly associated with postoperative seizure outcome in children are the seizure type (the patients experiencing CPS appear to have better outcomes) and pathological findings (patients with cortical dysplasia appear to have better outcomes than patients with other pathologies). Factors that are marginally associated with outcome include the location of surgery and age at surgery. Although not formally tested, the location of surgery appears to suggest that frontal lobe foci are associated with worse outcomes. Older children may experience better outcomes, probably due to the greater difficulty in localizing the epileptic region in very young children. In order to improve surgical outcomes, it may be necessary to resect epileptic tissue in multiple stages, as well as to carefully select patients to undergo surgery. Although there is no solid evidence in support of a particular method to improve outcomes, further studies should be performed to develop new techniques to increase the rate of seizure freedom in this population. The goal of surgery should remain to provide the patient with seizure freedom.
References
Cahan L, Sutherling W, McCollough AM, Rausch R, Engel J, Candall PH (1984) Review of 20 years' UCLA experience with surgery for epilepsy. Cleve Clin Q 51:313–318
Prats A, Morrison G, Wolf AL (1995) Focal cortical resections for the treatment of extratemporal epilepsyin children. Neurosurg Clin N Am 6:533–540
Pomata HB, González R, Bartuluchi M, Petre CA, Ciraolo C, Caraballo R, Cersósimo R, Tenembaum S, Soprano AM, Medina CS, Rabinowicz A, Waisburg H, Taratuto AL, Taratuto A, Monges J (2000) Extratemporal epilepsy in children: candidate selection and surgical treatment. Childs Nerv Syst 16:842–850
Siegel A, Cascino GD, Meyer FB, Marsh WR, Scheithauer BW, Sharbrough FW (2006) Surgical outcome and predictive factors in adult patients with intractable epilepsy and focal cortical dysplasia. Acta Neurol Scand 113:65–71
Frater J, Prayson RA, Morris HH III, Bingaman WE (2000) Surgical pathologic findings of extratemporal-based intractable epilepsy. Arch Pathol Lab Med 124:545–549
Haglund M, Ojemann GA (1993) Extratemporal resective surgery for epilepsy. Neurosurg Clin N Am 4:283–292
Schramm J (2008) Temporal lobe epilepsy surgery and the quest for optimal extent of resection: a review. Epilepsia 49:1296–1307
Westmoreland BF (1998) The EEG findings in extratemporal seizures. Epilepsia 39:S1–S8
Lee JJ, Lee SK, S-y L, Park K-I, Kim DW, Lee DS, Chung CK, Nam HW (2008) Frontal lobe epilepsy: clinical characteristics, surgical outcomes and diagnostic modalities. Seizure 17:514–523
Swartz BE, Halgren E, Delgado-Escueta AV, Feldstein P, Maldonado H, Walsh GO (1990) Multidisciplinary analysis of patients with extratemporal complex partial seizures. II. Predictive value of semiology. Epilepsy Res 5:146–154
Duchowny M, Jayakar P, Resnick T, Harvey AS, Alvarez L, Dean P, Gilman J, Yaylali I, Morrison G, Prats A, Altman N, Birchansky S, Bruce J (1998) Epilepsy surgery in the first three years of life. Epilepsia 39:737–743
Sinclair DB, Aronyk K, Snyder T, McKean JDS, Wheatley M, Gross D, Bastos A, Ahmed SN, Hao C, Colmers W (2004) Extratemporal resection for childhood epilepsy. Pediatr Neurol 30:177–185
Bauman JA, Feoli E, Romanelli P, Doyle WK, Devinsky O, Weiner HL (2005) Multistage epilepsy surgery: safety, efficacy, and utility of a novel approach in pediatric extratemporal epilepsy. Neurosurgery 56:318–334
Hirabayashi S, Binnie CD, Janota I, Polkey CE (1993) Surgical treatment of epilepsy due to cortical dysplasia: clinical and EEG findings. J Neurol Neurosurg Psychiatry 56:765–770
Blume WT, Whiting SE, Girvin JP (1991) Epilepsy surgery in the posterior cortex. Ann Neurol 29:638–645
Chugani HT, Shewmon DA, Shields WD, Raman S, Youssef C, Harry VV, Warwick JP (1993) Surgery for intractable infantile spasms: neuroimaging perspectives. Epilepsia 34:764–771
Olivier A, Boling W (2000) Surgery of parietal and occipital lobe epilepsy. Adv Neurol 84:533–575
Korkman M, Granström M-L, Kantola-Sorsa E, Gaily E, Paetau R, Liukkonen E, Boman P-A, Blomstedt G (2005) Two-year follow-up of intelligence after pediatric epilepsy surgery. Pediatr Neurol 33:173–178
Cukiert A, Buratini JA, Machado E, Sousa A, Vieira JO, Argentoni M, Forster C, Baldauf C (2001) Results of surgery in patients with refractory extratemporal epilepsy with normal or nonlocalizing magnetic resonance findings investigated with subdural grids. Epilepsia 42:889–894
Lehman R, Andermann F, Olivier A, Tandon PN, Quesney LF, Rasmussen TB (1994) Seizures with onset in the sensorimotor face area: clinical patterns and results of surgical treatment in 20 patients. Epilepsia 35:1117–1124
Wennberg R, Quesney F, Olivier A, Rasmussen T (1998) Electrocorticography and outcome in frontal lobe epilepsy. Electroencephalogr Clin Neurophysiol 106:357–368
Cohen-Gadol AA, Britton JW, Collignon FP, Bates LM, Cascino GD, Meyer FB (2003) Nonlesional central lobule seizures: use of awake cortical mapping and subdural grid monitoring for resection of seizure focus. J Neurosurg 98:1255–1262
Cohen-Gadol AA, Ã-zduman K, Bronen RA, Kim JH, Spencer DD (2004) Long-term outcome after epilepsy surgery for focal cortical dysplasia. J Neurosurg 101:55–65
Tandon N, Alexopoulos AV, Warbel A, Najm IM, Bingaman WE (2009) Occipital epilepsy: spatial categorization and surgical management. J Neurosurg 110:306–318
Hufnagel A, Zentner J, Fernandez G, Wolf HK, Schramm J, Elger CE (1997) Multiple subpial transection for control of epileptic seizures: effectiveness and safety. Epilepsia 38:678–688
McGonigal A, Gavaret M, Da Fonseca AT, Guye M, Scavarda D, Villeneuve N, Regis J, Bartolomei F, Chauvel P (2008) MRI-negative prefrontal epilepsy due to cortical dysplasia explored by stereoelectroencephalography (SEEG). Epileptic Disord 10:330–338
Malone S, Miller I, Jakayar P (2008) MRI-negative frontal lobe epilepsy with ipsilateral akinesia and reflex activation. Epileptic Disord 10:349–355
Engel J Jr, Van Ness P, Rasmussen TB, Ojemann L (1993) Outcome with respect to epileptic seizures. In: Engel J Jr (ed) Surgical treatment of the epilepsies. New York, Raven, pp 609–621
Binder DK, Podlogar M, Clusmann H, Bien C, Urbach H, Schramm J, Kral T (2009) Surgical treatment of parietal lobe epilepsy. J Neurosurg 110:1170–1178
Snead OC (2001) Surgical treatment of medically refractory epilepsy in childhood. Brain Dev 23:199–207
Centeno R, Yacubian EM, Sakamoto AC, Ferraz AFP, Carrete H Jr, Cacalheiro S (2006) Pre-surgical evaluation and surgical treatment in children with extratemporal epilepsy. Childs Nerv Syst 22:945–959
Wyllie E, Youssef GC, Prakash K, Juan B, William B, Paul R (1998) Seizure outcome after epilepsy surgery in children and adolescents. Ann Neurol 44:740–748
Dlugos DJ (2001) The early identification of candidates for epilepsy surgery. Arch Neurol 58:1543–1546
Goyal M, Robinson S (2008) Expanding the role of surgery in intractable extratemporal pediatric epilepsy. Neurosurg Focus 25:E15
Huttenlocher P (1994) When does childhood epilepsy become intractable? Indications and contraindications for epilepsy surgery in children. Semin Pediatr Neurol 1:118–126
Panayiotopoulos CP, Michael M, Sanders S, Valeta T, Koutroumanidis M (2008) Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Brain 131:2264–2286
Elsharkawy AE, Behne F, Oppel F, Pannek H, Schulz R, Hoppe M, Pahs G, Gyimesi C, Nayel M, Issa A, Ebner A (2008) Long-term outcome of extratemporal epilepsy surgery among 154 adult patients. J Neurosurg 108:676–686
Elsharkawy AE, May T, Thorbecke R, Ebner A (2009) Predictors of quality of life after resective extratemporal epilepsy surgery in adults in long-term follow-up. Seizure 18:498–503
Tellez-Zenteno JF, Dhar R, Wiebe S (2005) Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain 128:1188–1198
Elsharkawy AE, Pannek H, Schulz R, Hoppe M, Pahs G, Gyimesi C, Nayel M, Issa A, Ebner A (2008) Outcome of extratemporal epilepsy: experience of a single center. Neurosurgery 63:516–526
Shukla G, Bhatia M, Singh VP, Jaiswal A, Tripathi M, Gaikwad S, Bal CS, Sarkar C, Jain S (2003) Successful selection of patients with intractable extratemporal epilepsy using non-invasive investigations. Seizure 12:573–576
Terra-Bustamante VC, Fernandes RMF, Inuzuka LM, Velasco TR, Alexandre V, Wichert-Ana L, Funayama S, Garzon E, Santos AC, Araujo D, Walz R, Assirati JA, Machado HR, Sakamoto AC (2005) Surgically amenable epilepsies in children and adolescents: clinical, imaging, electrophysiological, and post-surgical outcome data. Childs Nerv Syst 21:546–551
Adler J, Erba G, Winston KR, Welch K, Lombroso CT (1991) Results of surgery for extratemporal partial epilepsy that began in childhood. Arch Neurol 48:133–140
Fogarasi A, Tuxhorn I, Hegyi M, Janszky J (2005) Predictive clinical factors for the differential diagnosis of childhood extratemporal seizures. Epilepsia 46:1280–1285
Tanriverdi T, Poulin N, Olivier A (2008) Psychosocial outcome after extratemporal epilepsy surgery: a prospective clinical study. Turk Neurosurg 18:114–124
Tracy JI, Dechant V, Sperling MR, Cho R, Glosser D (2007) The association of mood with quality of life ratings in epilepsy. Neurology 68:1101–1107
Tanriverdi T, Olivier NP, Olivier A (2008) Quality of life after extratemporal epilepsy surgery: a prospective clinical study. Clin Neurol Neurosurg 110:30–37
Selwa LM, Schmidt SL, Malow BA, Beydoun A (2003) Long-term outcome of nonsurgical candidates with medically refractory localization-related epilepsy. Epilepsia 44:1568–1572
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansari, S.F., Maher, C.O., Tubbs, R.S. et al. Surgery for extratemporal nonlesional epilepsy in children: a meta-analysis. Childs Nerv Syst 26, 945–951 (2010). https://doi.org/10.1007/s00381-009-1056-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-009-1056-7