Abstract
Objective
The objective of this study is to investigate the characteristics of rare meningiomas occurring during childhood and adolescence specially demography, locations, radiological findings, pathological features, and outcome; 34 patients can be followed up and analyzed.
Methods
Fifty-nine patients with meningiomas were treated during the period of 2000–2007 at the Department of Neurosurgery, Beijing Tiantan Hospital. Thirty-four cases which can be followed up were analyzed by retrospective method. Clinical presentation, anatomical distribution, radiological findings, clinical behavior, outcome, and follow-up are summarized.
Results
All cases had been performed microsurgical treatment including 20 cases totally resection. Eleven cases have been achieved subtotal resection. Two patients have been performed biopsy because of giant tumor volume. One patient has been partially resected for internal carotid artery involved. The operative mortality is zero. The average follow-up period is 4 years long. There was recurrence in seven and metastasis in two. Adjuvant radiotherapy has been performed on residual, malignant, and recurrent tumors. Six patients are dead.
Conclusions
The sex predominance is not similar to that in adults. Increased ICP, decreased visual acuity, and seizure are the common presentation. There is a higher incidence of intraventricle and skull base region. Larger size and frequent abnormal tumor calcification and cyst appear not relative to pathological subtypes. The higher incidence of atypical histopathological features than adult is affirmative. The prognosis is good if the tumor can be totally removed and adjuvant radiotherapy not to be significant beneficial after incomplete excision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Meningiomas belong to the most common intracranial neoplasms, this entity accounts for 10–20% of all intracranial tumors in adults. The incidence of meningiomas rises with advancing age and is more common in women [1]. However, the low incidence of children and adolescent meningiomas (CAMs) has resulted in a lack of information that might allow conclusions based on clinical characteristics, biological behavior, treatment, and outcome. They, representing only 0.4–4.1% of the pediatric-age tumors and 1.5–2% of all intracranial meningiomas [2–4], constitute a challenging issue for pediatric neurosurgeons because of their different behavior as compared with adult meningiomas. Several teams have reviewed the large pool of data obtained from the pertinent literature and have seemed to some conclusions. But, the data may not be adequately reliable because of the different ages even about 50 years ago and different centers in so many countries where the knowledge and technology is distinct.
Patients and methods
Among all the CNS tumors operated during the period of 2000–2007 at Department of Neurosurgery, Beijing Tiantan Hospital, Capital Medical University referred to, only 59 tumors were histologically verified meningiomas occurring in patients below the age of 17. But 34 cases out of them can be followed up. So, we analyze these 34 patients to investigate the characteristics of CAMs. Clinical information was obtained by review of patient records and operative reports, computed tomography (CT) or magnetic resonance (MR) images, and follow-up data which was obtained via telephone interviews. Age, sex, presenting symptoms, neurological examination results, histopathologic findings, operation, radiological therapy, and prognosis were evaluated. All patients were scanned with CT and/or magnetic resonance imaging (MRI). Radiological findings such as location, size, cystic changes, calcification, edema, and contrast enhancement were analyzed.
Results
Incidence, age, and sex distribution
Out of 2,891 intracranial meningiomas operated on at Beijing Tian Tan Hospital during this period, only 59 cases (2.04%) were under 17 years old. Among these cases, there are 29 boys and 30 girls, ranging in age from 2 to 17 years (median 10 years). Twenty-eight of these cases occur in childhood (<11 years) and 31 cases in adolescence (12–18 years). There is no newborn or infant patient (see Table 1). The sex ratio between male and female is 0.97:1. Table 1 shows the distribution of age and sex.
Among these 59 children and adolescent with meningiomas, only 34 patients can be followed up. So, we analyzed 34 patients to investigate on the characteristics.
Clinical presentation
The most common symptoms are headache, nausea, and vomiting related to increased intracranial pressure (n = 22). Other common symptoms included generalized seizures and decreased visual acuity and weakness. Seizures are present in six of 34 patients. Generalized seizures are present in patients with supratentorial convexity, sphenoid ridge lateral 1/3, and cavernous sinus (n = 5). A deep sylvian fissure (case 9) meningioma was associated with focal motor seizures with intermittent secondary generalization. Various focal neurological deficits related to tumor location were present in seven of the 34 patients, including diplopia, aphasia, facioplegia, decreased hearing, ptosis, ataxia, and dysphagia. Two patients were presented with palpable mass (cases 24 and 31). The ages at onset of symptoms or signs are between 2 and 17 years (median 10 years). The median preoperative duration of symptoms is 2 months (range 1 week to 7 years). Most of the patients exhibited their symptoms for less than 12 months. The clinical presentations are summarized in Table 2.
Anatomical distribution
In our series, the patients were all with single lesion before first operation.
Supratentorial lesions were accounted in 27 cases. The tumor is located at the cerebral convexity in six cases; at parasagittal and parafalcine in two cases; at occipital diploe in one case; at anterior or middle cranial fossa in one case each; at tubercullum sellae or cavernous sinus in one case each; at sphenoid ridge in one case; and at tentorium in two cases.
Intraparenchymally, the tumor was located at the lateral ventricle trigone in five cases; at third ventricle in two cases; occupying bilateral and third ventricle together in one case; and at deep Sylvian fissure in three cases.
Infratentorial lesions summed up to eight cases. The tumor was located at cerebellopontine angle in two cases; at petrous apex in three cases; and at foramen magnum or posterior cranial fossa one case each.
The locations of tumors in 34 patients list as Table 3.
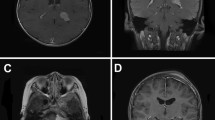
Radiological findings
Tumor sizes range from 2 to 11 cm in the longest diameter (average 5.3 cm). Lobe form tumor is showed in 15 cases. Other tumors are showed globular form.
Sixteen cases were diagnosed using CT; MRI was performed in 28 patients. Nine patients performed both. CT scan showed hypodense, hyperdense, or mixed-density lesions and homogeneous and heterogeneous enhancement on postcontrast studies. Bone erosion was seen in two cases. Bone hyperostosis like sunray effect was seen in case 24. Tumor calcification was present in nine cases, ranging in appearance from fine and cloud-like or punctate to dense and nodular.
MRI showed hypo- to isointense patterns on T1- and T2-weighted images, besides homogeneous or heterogeneous enhancement on post-gadolinium studies. MRI of eight cases showed a cystic component. Among them, pathological investigation revealed five cases WHO grade III or II. Compare with 11 cases high-grade out of 34 cases. It seems that a relationship between cystic component and high-grade pathology, but the outcome of Fish exact probability test is not obviously difference. Moderate peritumoral edema was detected in 14 cases, severe edema in five cases, and no obvious edema in 15 cases. Most tumors showed homogeneous dense enhancement. We can see marked dural tail sign in 10 cases, compare to 15 cases with no dural enhancement except nine cases with intraventricular tumor.
Pathological findings
The histological subtypes were meningothelial in nine cases. The pathological finding in case 34 was meningothelial with active growth, and it has a WHO grade of II. Two of the 12 cases with fibrous (fibroblastic) subtype were meningioma with karyokinesis, and they have a pathological grade of II. One of the five cases with transitional (mixed) subtype was transitional meningioma with brain tissue invasion, so it has a WHO grade of II. Anaplastic (malignant) subtype was in three cases, atypical in two cases, and angiomatous, secretory, and papillary (with partial hemangipericytoma texture) in one case each. Above all, brain invasion by the meningioma, active growth, or meningioma with karyokinesis were noted in five cases. In our study, the number of non-benign tumor (grade > I) was six (17.6%). It is significantly more than that of all meningiomas (about 10% [5, 6]) (Table 4).
Clinical behavior, outcome, and follow-up
In our series, all cases had been performed with microsurgical treatment including total resection on 20 cases. Adjuvant radiotherapy was performed in four cases (cases 13, 15, 20, 21) and total resection without radiotherapy in two cases (cases 23, 27). Eleven cases have been achieved subtotal resection, and five of them have performed adjuvant radiotherapy (three of five were grades II or III). Two cases (cases 26, 31) were performed biopsy because of giant tumor volume. Case 28 was partially resected for internal carotid artery involved.
All cases had average follow-up period of 4 years (0.4–8.1 years). There were six death cases (17.6%, cases 10, 14, 19, 26, 31, 34) due to the tumor recurrence and brain compression after operation. Two patients (cases 26, 31) had giant supratentorial tumor and processed biopsy only to identify the pathology. One patient (case 34) had a thoracic and lumber cord metastasis 1 year after operation and dead from recurrence 2 years after operation. One patient (case 14) died 1 year after operation due to generalized seizure onset. The other two patients (cases 10, 19) died because of recurrence and the family gave up on them. Among the death cases, three (10, 19, 34) had been subtotal or partial resection and radiological therapy; their pathological report are anaplastic (malignant) subtype or actively growth nature.
In our series, there were seven patients who had been radiologically treated because of non-total resection or high-grade pathology. Among them, two patients were totally resected but with high grade; two patients were not totally resected with low grade; three patients were with both problems. Then, three of them had been already dead due to recurrence or metastasis; four patients were followed up without recurrence; case 8 had been recurrent but without tumor augmentation.
Twenty patients show no evidence of the disease clinically and radiologically. The other four cases show no recurrence but focal seizure, hand numbness, or hemiparesis partially.
There are 11 cases recurrent or metastatic which can be classified into three kinds. Firstly, six cases with pathological WHO grades II or III, including two cases with radiological therapy, have been performed total resection and had not any recurrence and metastasis. Secondly, 11 cases have not been performed total resection; seven cases of them were WHO grade I, including 1case with RT. Among them, two cases (8 and 28) were recurrent or metastatic, and case 8 r-knifed 3 years after operation because of recurrence, and now the tumors have not grown. Thirdly, most poor cases (10, 19, 32, 34) were the patients who have not been totally resected and were with high pathological grade. All of them were radiologically treated, but everyone had recurrence or/and metastasis. The therapeutic, prognostic, and follow-up data are summarized in Table 5.
Discussion
Demography
Meningiomas are relatively rare intracranial neoplasms in childhood and adolescent, since they have different features as compared with adult meningiomas [2–4, 7]. In the pre-CT era, reports of CHMs were rarely found in the relevant neurosurgical literature. Among the 750 intracranial tumors reported by Matson [8], only three (0.4%) were meningiomas. Cushing and Eisenhardt [9] found only six patients under the age of 21 among 313 with meningiomas (1.9%). Recent studies reported that children and adolescent meningiomas represent 1.5–2% of all meningiomas and 0.4–4.1% of all intracranial pediatric tumors [2–4]. In our group, they represented 2.04% of all meningiomas operated during the same period. The availability of better diagnostic tools, surgical techniques, and sophisticated immunohistochemical staining methods influenced higher rates of referral of such cases and help resolve the problem of some atypical cases. The sex ratio between male and female is 0.97:1. The sex predominance is not similar to that in adults which is about 2:1 [5, 6].
Clinical presentation
The clinical presentation is variable and often depended on the site of the tumor. In our study, it seems that the most common clinical manifestations of PDMs are the signs of increased ICP (41.5%), which present headache with or without nausea, vomiting, and papilledema. The reason is that the tumors grow slowly and massive, usually starting from intraventricular site (26.5%) and posterior cranial fossa (20.6%) leading to CSF circulation obstruction. The following common presentation is visual disorder, including decreased visual acuity (9.4%) and diplopia (5.7%). Visual sensation pathway compression from tumor and secondary optic atrophy from increased ICP are the main reason. Then, the other clinical presentation is seizure (9.4%), limbs weakness (7.5%), and brainstem or cranial nerve compression symptoms such as facioplegia, decreased hearing, dysphagia, and ataxia. This finding is the same to some authors [3, 10, 11] and contrary to the conclusions of other authors [2–4, 7, 9, 12, 13] who report focal neurological deficit as the most frequent presentation (33%), followed by seizure (25%), and symptoms of increased ICP (25%). We have not encountered patients with the insidious onset of symptoms [14–16].
Imaging characteristics
Computed tomography and MR images have been widely used diagnostic tool in our hands but not every patient scan both. Computed tomography showed these tumors with sharp and lobulated margins and homogeneous and heterogeneous postcontrast enhancement, some of them with remarkable peritumoral edema. MRI has become the definitive method of diagnosis. It has an important role in the early detection of recurrent tumors during follow-up assessments, which may provide a better chance of complete tumor removal and a longer satisfactory survival. Childhood meningiomas show variable imaging features on CT/MRI, and there are no typical imaging features that might suggest meningioma in children.
In our series, tumor calcification were observed in 10 cases (29.4%), ranging in appearance from fine and cloud-like or punctate to dense and nodular. Focal erosion or hyperostosis like “sunray effect” was shown in three cases. Cystic meningioma is more frequent in children and may involve various types of tumor cysts. Caroli reports 15% frequency of intra- or peritumoral cysts, whereas in the adult population, cystic forms are present in 2–4% of all meningiomas [11, 17–19] and that the average duration of clinical history was 1.2 years to be shorter than meningiomas at other ages (2.8–3.5 years) [20], In our series, 12 cases (35%) showed a cystic component, and the average duration is 1 year. The tendency of cystic tumor may be attributed to the manifestation earlier than solid ones.
Tumor localization and size
The convexity and parasagittal locations are the most frequent sites of meningiomas in adults (>50%) [7] and in several series of CHMs (55%) [21]. This series differs from others in that the parasagittal, parafalcine, and convexity localization were encountered in only eight cases (23.5%), while tumors occurring in peculiar localizations such as intraventricular(23.5%) and sylvian fissure(8.8%). Then, other tumors origin around the skull base region, i.e., petroclival (8.8%), CPA (5.9%), foramen magnum tubercullum sellae, cavernous sinus, sphenoid ridge, subfrontal, and subtemporal tumors comprise 32.3% of the cases. Some authors believe that the large size of some CHMs which has been mentioned in several series [22, 23], especially in those including NF pedigrees, implicates NF as a stigma suggestive of rapid tumor growth [24]. But, we found 19 large tumors (>5 cm in diameter) in 56% of the cases in this series without any sign of NF and 11 (57.8%) out of them is finally with relatively good clinical outcome. So, the concept of a large CHM as an aggressive tumor with a rather poor prognosis and outcome is not accepted.
Histopathological variants
Meningothelial meningiomas constitute the major subtype in many series [7, 16]. In our series, fibrous (fibroblastic) meningiomas is the major subtype, the following are meningothelial and the transitional meningiomas. Cystic changes and calcification seem not relative to the pathological subtypes. The histopathological examination revealed a grade III meningioma in two cases, a grade II neoplasm in nine patients, and a grade I meningioma in 23 cases, according to the 2007 WHO grade classification [25]. Among them, two cases were put into grade II class because of tumor with actively growth or with karyokinesis. There were totally 11 non-benign tumors among the 34 tumors, supporting the higher incidence of atypical histopathological features in childhood and adolescence meningiomas.
Meningiomas with brain invasion, karyokinesis, or active growth were given importance in our series. Only case 34 was radiologically treated for subtotal resection; thoracical and lumber cord metastasis occurred 1 year after operation. She waited and was recurrent and dead 2 years after operation. Other patients were all resected totally without radiology treatment, now they are all alive without recurrence. Therefore, if meningiomas have no evidence of malignancy, brain invasion, karyokinesis, and active growth, it is of the most impotence that total resection and postoperative adjuvant therapy are not imperative.
Clinical behavior and outcome
The marked operative mortality has been decreasing in the last decades. Surgical treatment is reported in 412 children [20], with an operative mortality of 7%. Precisely, 63 patients were operated on before 1970, with an operative mortality of 26.7%; 119 patients were operated on between 1970 and 1989, with an operative mortality of 10%; and 260 children were operated on between 1990 and 2004, with an operative mortality of 0.3%. Except for the relatively older age factor, in which the youngest case was 2 years old and the average age was 14 years in our series, it is the earlier relative diagnosis and progress in microsurgical anesthesiologic techniques and better preoperative care, the experience currently available in the pediatric neurosurgery departments; total elimination of the atypical and nominated malignant subtypes and large tumors have been the factors for us to lower the operative mortality to zero in all our 34 patients.
It is suggested that the typical meningiomas occurring in the first two decades of life have a low recurrence rate if total resection in microsurgical can be achieved and have excellent outcome with a good long-term survival rate [10, 20]. In our series, 20 cases have been achieved total resection in microsurgical, and anyone of them has not been recurrent with the average of 4-year period of follow-up, even if the patients with the relative tumor invasion, who have been performed total resection and adjuvant radiotherapy (cases 13, 15, 20, 21) and total resection without radiotherapy (cases 23 and 27).
Eleven cases have been achieved subtotal or partial resection. Five cases have performed adjuvant radiotherapy (three of five were grades II or III), and four cases have been recurrence or metastasis (three of four were grades II or III). Among the other six cases, two (8 and 28) were recurrent or metastatic. Case 8 r-knifed 3 years after operation because of recurrence; now, the tumors have not grown. So, above all, from our observation, adjuvant radiotherapy has not appeared to be significant beneficial after incomplete excision of meningiomas in children for lower recurrence rate, but it is rather risky to use radiotherapy for benign and partially excised cerebral lesions during childhood.
Conclusion
In summary, comparison of our observations with those reported in the available literature suggests the conclusions that (a) the sex predominance is not similar to that in adults; (b) increased ICP (41.5%), decreased visual acuity (9.4%), and seizure (9.4%) are the common presentation; (c) there is a higher incidence of intraventricular, skull base region; (d) huge size and frequent abnormal tumor calcification and cyst appear not relative to pathological subtypes; (e) the higher incidence of atypical histopathological features is affirmative; (f) the prognosis is good if the tumor can be totally removed; and (g) adjuvant radiotherapy not to be beneficial after incomplete excision.
References
Abdulrauf SI, Al-Mefty O (2003) Intracranial meningioma. In: Batjer HH, Loftus CM (eds) Textbook of neurological surgery, vol 2. Lippincott/Williams & Wilkins, Philadelphia, pp 1303–1311
Di Rocco C, Di Rienzo A (1999) Meningiomas in childhood. Crit Rev Neurosurg 9:180–188
Amirjamshidi A, Mehrazin M, Abbassioun K (2000) Meningiomas of the central nervous system occurring below the age of 17: report of 24 cases not associated with neurofibromatosis and review of literature. Child’s Nerv Syst 16:406–416
Zwerdling T, Dothage J (2002) Meningiomas in children and adolescents. J Pediatr Hematol Oncol 24:199–204
Jason R, Maciej M, Marc CC (2007) Intracranial meningiomas: an overview of diagnosis and treatment. Neurosurg Focus 23(4):1–7
Whittle IR, Smith C, Navoo P, Collie D (2004) meningiomas. Lancet 363:1535–43
Erdincler P, Lena G, Sarioglu AC, Kuday C, Choux M (1998) Intracranial meningiomas in children: review of 29 cases. Surg Neurol 49:136–140
Matson DD (1969) Tumors of the skull and meninges. In: Matson DD (ed) Neurosurgery of infancy and childhood, 2nd edn. Thomas, Springfield, pp 697–631
Germano IM, Edwards MSB, Davis R, Schiffer D (1994) Intracranial meningiomas of the first two decades of life. J Neurosurg 80:447–453
Tufana K, Dogulua F, Kurta G, Emmeza H, Cevikera N, Baykanerb MK (2005) Intracranial meningiomas of childhood and adolescence. Pediatr Neurosurg 41:1–7
Im S-H, Wang K-C, Kim S-K, Oh C-W, Kim DG, Cho B-K (2001) Childhood meningioma: unusual location, atypical radiological findings, and favorable treatment outcome. Child's Nerv Syst 17:656–662
Deen HG Jr, Scheithauer BW, Ebersold M (1982) Clinical and pathological study of meningiomas of the first two decades of life. J Neurosurg 56:317–322
Choux M, Lena G, Genitori L (1991) Meningioma in children. In: Schmideck HH (ed) Meningiomas and their surgical management. Saunders, Philadelphia, pp 93–102
McDermott MW, Wilson CB (1996) Meningiomas. In: Youmans JR (ed) Youman's neurological surgery, 4th edn. Saunders, Philadelphia, pp 2794–2795
Sano K, Wakai S, Ochiai C, Takakura K (1981) Characteristics of intracranial meningiomas in childhood. Child's Brain 8:98–106
Sheikh BY, Siqueira E, Dayel F (1996) Meningioma in children: a report of nine cases and review of literature. Surg Neurol 45:328–335
Mallucci CL, Parkes SE, Barber P et al (1996) Paediatric meningeal tumors. Child’s Nerv Syst 12:582–589
Artico M, Ferrante L, Cervoni L, Fortuna A (1995) Pediatric cystic meningioma: report of three cases. Child’s Nerv Syst 11:137–140
Darling CF, Byrd SE, Reyes-Mugica M et al (1994) MR of paediatric intracranial meningiomas. AJNR Am J Neuroradiol 15:435–444
Caroli E, Russillo M, Ferrante L (2006) Intracranial meningiomas in children: report of 27 new cases and critical analysis of 440 cases reported in the literature. J Child Neurol 21:31–36
Davidson GS, Hope JK (1989) Meningeal tumors in childhood. Cancer 63:1205–1210
Siqueira EB, Kannan I, Ali MA (1989) Large meningioma of foramen magnum in a 4 year old child. Surg Neurol 31:409–411
Alp H, Cevikler N, Baykaner K, Orbay T (1985) Giant meningioma in fourteen month old infant. Surg Neurol 24:77–79
Lopez MJ, Olivares JL, Ramos F, Redondo JA, Ramon Y, Cajal S, Banzo J, Legido A (1988) Giant meningioma in a 5 month old infant. Child's Nerv Syst 4:112–115
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, X., Zhao, J. Intracranial meningiomas of childhood and adolescence: report of 34 cases with follow-up. Childs Nerv Syst 25, 1411–1417 (2009). https://doi.org/10.1007/s00381-009-0949-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-009-0949-9