Abstract
Objects
Optic nerve sheath diameter has been linked with intracranial pressure in previous studies. Measurement of sheath diameter using transorbital ultrasound is proposed as a clinical assessment indicator of developing hydrocephalus in the paediatric population.
Methods
A retrospective review of optic nerve sheath ultrasound examinations performed in a clinical setting between 2000 and 2006 for assessment of hydrocephalus in a single institution.
Results
A total of 331 examinations were performed in 160 patients over the study period. A satisfactory image was possible in all cases. Sheath diameters were correlated with clinical case data from concurrent case records.
Conclusion
Transorbital ultrasound is a reproducible, non-invasive technique for the assessment of optic nerve sheath diameter and is well tolerated in children. Our series revealed asymptomatic baseline value higher than in previous reports. Variation from individual case asymptomatic baseline was the most sensitive variable in the series in determining development of hydrocephalus. This technique is felt to be a useful adjunct in the assessment of hydrocephalus in the paediatric neurosurgical population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The observation that optic nerve sheath diameter changes with intracranial cerebrospinal fluid (CSF) dynamics was made by Hansen and Helmke [1]. They also described a sonographic technique which allowed measurement of the diameter non-invasively and how this diameter was dynamic and linked to changes in CSF pressure [2, 3]. A clinical study by Newman et al. using this technique observed a significant correlation in a group of shunted hydrocephalic patients with shunt malfunction compared with a control population. They suggest normal values for optic nerve sheath diameter taken 3 mm behind the globe to be < 4 mm in infants and < 4.5 mm in older children [4]. The observation in our unit that baseline ‘normal’ values in the asymptomatic shunted hydrocephalus population were significantly higher than those reported by the Glasgow group prompted this study of the clinical relevance of the information gained from optic nerve sheath measurement in the assessment of the shunted hydrocephalic population.
Materials and methods
A retrospective review of optic nerve sheath ultrasound examinations performed in a clinical setting between February 2000 and October 2006 in the Royal Belfast Hospital for Sick Children. Patients were identified from the radiology department’s computerised database, and a clinical case review was performed from hospital records correlating axial brain imaging, sonographic diameters, clinical presentation and surgical outcome of shunt intervention.
The sonography was performed using either the Sequoia Ultrasound System or Acuson 128XP Computed Sonography System (Acuson Corporation, Mountain View, CA, USA)
An 8–13 MHz linear array probe was used, set power “low” and space peak time average sound energy < 100 mWcm−2.
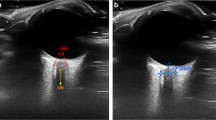
Patients were placed supine on the examination couch with eyes closed in a neutral position. The ultrasound probe was applied to the closed eyelid using a coupling gel and axial images taken of each globe. The transverse diameter of the optic nerve sheath (ONSD) at 3 mm behind the optic nerve head was taken using the digital cursor of the ultrasound machine (Fig. 1a,b). The average diameter of three separate measurements was taken as the value for that eye. The examination was performed by paediatric radiographers experienced in the technique and reported by consultant paediatric radiologists.
Results
During the study period, 331 examinations (658) orbits were performed in 160 shunted hydrocephalic patients. Seventy-four patients had shunts associated with myelomeningocoele. Complete optic nerve sheath diameter (ONSD) data was available for 303 (92%). Ninety-two patients had a single examination with 68 (42.5%) having multiple, sequential examinations (Fig. 2).
Optic nerve sheath diameters are displayed in Table 1.
Evaluating individual patients who had ONSD measured whilst asymptomatic and symptomatic yielded the following results using mean values of multiple examinations (Table 2).
Using a paired samples t test, the difference in mean ONSD in patients when symptomatic of shunt malfunction was significant when compared with their own asymptomatic baseline values (Table 3).
Sixty-eight patients had multiple examinations for which complete clinical and ONSD data was available in 51 (75%). The ONSD change was deemed to be clinically relevant to the final diagnosis in 29 of those 51 (56.8%). If one assumes that it was irrelevant in the remaining cases for which there was incomplete data, this still leaves 42.6% (29/68) in which the findings were felt to be correlative.
Twenty-four of 29 (82.8%) had an ONSD that correlated positively with shunt block. Of these, 19 (79.2%) were associated with no change in CT or MR ventricular configuration. Five (20.8%) were associated with a diagnostic change on CT/MR axial imaging.
Nineteen of 29 patients had a surgical shunt exploration on the basis of symptoms suggestive of shunt malfunction with no change in ventricular configuration on axial CT/MR imaging but were noted to have ONSD increased from baseline. Of these, one patient was found to have a patent shunt system at operation.
Two patients had ONSD diameter which did not correlate to shunt malfunction and three patients who initially appeared to correlate, subsequent to shunt revision had an ONSD which failed to return to baseline.
A number of miscellaneous observations were also made. One patient with symptoms of raised intracranial pressure and increased ONSD, resolved spontaneously without intervention. The ONSD returned to baseline with resolution of symptoms. One patient had an ONSD decreased from baseline associated with symptoms of overdrainage. Again this resolved after shunt intervention. Two patients were noted to have higher asymptomatic baseline ONSD values after revision of their shunt valves to gravity-assisted valve devices. Ventricular size was similarly increased on axial imaging.
Of the 45 asymptomatic patients in our series with complete clinical data, 26 demonstrated ONSD > 4.5 mm (57.8%), again significantly higher than previous reports [4, 5]. Whilst this paper presents a higher baseline asymptomatic population mean from the Newman paper, it must be recognised that the control group is different. The Glasgow group utilised non-hydrocephalus patients attending for renal ultrasound as their control population. Our series studies the asymptomatic hydrocephalic group as their own control. The justification for this comes from previous work from our radiology department [6, 7] where a retrospective study of 63 asymptomatic myelomeningocoele-associated shunted hydrocephalic patients was performed over a 6-year period (1997–2003). The age range in this group was 2–19 years and ONSD was measured from 2.1–7.1 mm with an inter-eye variance of 0.1 mm. In that series, again 44/63 (70%) had asymptomatic values > 4.5 mm. Eight patients in the same group were rescanned when symptomatic, and all demonstrated increased ONSD with a mean of 6.0 mm compared with 4.8 mm when well (P = 0.008; Wilcoxon Signed Ranks Test).
In our current series, inter-eye variance overall was –0.076 mm which is well within the tolerance of the sonographic system (Table 1).
Conclusion
Transorbital optic nerve sheath ultrasound is a reproducible, non-invasive technique and is well tolerated in children. This series reports asymptomatic values in the shunted hydrocephalic population significantly higher than in previous studies. ONSD is increased in symptomatic patients from their own baseline values. This may have a predictive role in the assessment of hydrocephalus or shunt malfunction when brain imaging reveals static ventricular configuration. Multiple examinations are necessary to evaluate the ONSD pattern for each patient to determine clinical relevance in that individual.
References
Hansen HC, Helmke K (1996) The subarachnoid space surrounding the optic nerves. An ultrasound study of the optic nerve sheath. Surg Radiol Anat 18(4):323–328
Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol 26(10):701–705
Helmke K, Hansen HC (1996) Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol 26(10):706–710
Newman WD, Hollman AS, Dutton GN, Carachi R (2002) Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol 86(10):1109–1113
Ballantyne J, Hollman AS, Hamilton R, Bradnam MS, Carachi R, Young DG et al (1999) Transorbital optic nerve sheath ultrasonography in normal children. Clin Radiol 54(11):740–742
Bamford L et al (2004) presented at the European Congress of Radiology, Vienna
Bamford L et al (2005) presented at the British Medical Ultrasound Society Meeting. Manchester, UK
Acknowledgements
Thanks to Dr Chris Patterson, Medical Statistician, Queen’s University, Belfast for his assistance with data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McAuley, D., Paterson, A. & Sweeney, L. Optic nerve sheath ultrasound in the assessment of paediatric hydrocephalus. Childs Nerv Syst 25, 87–90 (2009). https://doi.org/10.1007/s00381-008-0713-6
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0713-6