Abstract
Introduction
In a small subset of patients, a Chiari malformation can present with signs of raised intracranial pressure due to obstruction of cerebrospinal fluid flow or with the raised intracranial pressure as the primary pathological driving force resulting in tonsillar herniation.
Case report
The authors report a unique case in a 14-year-old boy with a Chiari malformation type 1–syringomyelia complex with slit-like ventricles. We have successfully managed the acute presentation of raised intracranial pressure, mimicking idiopathic intracranial hypertension, utilizing a frameless stereotactic image-navigated endoscopic third ventriculostomy alone. We present the preoperative and postoperative radiological and ophthalmological findings and discuss the possible mechanisms related to the pathophysiology and treatment in this case. The patient’s symptoms resolved immediately postoperatively with resolution of papilledema. At 18-month follow-up, the patient remains entirely asymptomatic and the need for craniovertebral decompression appears to have been obviated.
Conclusion
We advocate that in the Chiari malformation type 1–syringomyelia complex with normal or small ventricles, patients presenting with isolated signs and symptoms of raised intracranial pressure alone can be safely and effectively managed with an electromagnetic-guided stereotactic endoscopic third ventriculostomy as a primary treatment option.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chiari 1 malformations are characterized by downward displacement of the cerebellar tonsils through the foramen magnum into the cervical spinal canal. Chiari 1 malformations (CM1) are most commonly either asymptomatic or present subacutely with the most common presenting symptom being headache or neck pain [2, 15]. The presenting signs are usually related to brainstem or cranial nerve dysfunction, spinal cord dysfunction, or cerebellar dysfunction [2, 15]. A spinal syrinx may occur in association with Chiari 1 malformations in up to 40% of all cases [15, 16]. The cervical cord is the most common site. Associated hydrocephalus occurs in 7–10% of cases [12, 17]. Acute presentations of Chiari 1 malformations without hydrocephalus but with isolated papilledema and visual obscurations is uncommon and is especially rare in children [16]. Papilledema has occasionally been associated with Chiari 1 malformation in the published literature. Milhorat et al. reported that nine (2%) of 364 patients symptomatic from Chiari had papilledema. Seven of the nine patients (80%) had normal-sized ventricles on cranial magnetic resonance imaging (MRI).
We report a case where the initial diagnosis of idiopathic intracranial hypertension–pseudotumor cerebri (PTC) was considered based on papilledema and headaches being the only presenting features associated with a normal computed tomography (CT) head report. The diagnosis was revised after a MRI of the brain was performed revealing a Chiari 1 malformation with a concomitant syrinx. The standard treatment for symptomatic Chiari 1 malformations without ventriculomegaly is posterior craniovertebral decompression [6, 16]. We have successfully managed the acute presentation in this patient with a frameless stereotactic image-guided endoscopic third ventriculostomy alone.
Case report
History
A previously well 14-year-old boy presented with a 4-day history of visual disturbances in his right temporal field of vision described as “round blobs,” morning temporal headaches, and bilateral pulsatile tinnitus. There was no past medical history of note.
Examination and investigation
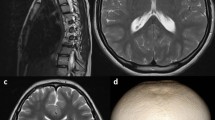
Fundoscopy revealed eye findings as shown (Fig. 1). Peripheral, central nervous system, and general examination was otherwise normal. A CT head scan was performed and reported as normal. Based on the clinical presentation and CT report, the diagnosis of benign or idiopathic intracranial hypertension was suspected and the patient underwent a lumbar puncture (LP). The opening pressure was 47-cm water. Cerebrospinal fluid analysis was normal. The patient was referred for a neurosurgical opinion and a MRI of the brain and spine was performed. MRI demonstrated (Fig. 2) a Chiari 1 malformation extending 5.9 mm below the foramen magnum and a syrinx extending from T4–T5 to T6 with a maximum diameter of 7 mm. With evidence of obstruction to outflow of cerebrospinal fluid (CSF) at the foramen magnum (Fig. 2) and clinical signs of raised intracranial pressure without cerebellar or brainstem dysfunction, a decision was made to perform a CSF diversion procedure—ETV—as the first line of management.
Operation
Due to the small ventricular size, a stereotactic electromagnetic (EM) frameless image-guided endoscopic third ventriculostomy was performed using a 2-mm pediatric endoscope and a light touch balloon. A standard right frontal coronal burr hole was employed to gain first pass access into the right frontal horn of the lateral ventricle. There were no intraoperative or postoperative complications.
Postoperative course
At 1 month postoperatively, there was resolution of papilledema, macular signs, and headaches. MRI of the brain has shown an excellent CSF flow jet through the third ventricle (Fig. 3). The Chiari malformation was still present and measures 9 mm and to date there has been no change to the syrinx morphology. At 18-month follow-up, the patient remains entirely asymptomatic with resolution of papilledema (Fig. 4).
Discussion
Most patients with Chiari 1 malformations are asymptomatic or present either with subacute or chronic symptoms linked to posterior fossa–brainstem compression [2, 6, 15, 16,]. Our nonobese male pediatric patients’ clinical presentation is rare. The pathophysiology of congenital–idiopathic Chiari 1 malformation remains controversial and incompletely understood [16]. Idiopathic intracranial hypertension in prepubertal children is rare and has different characteristics than that in adults [7, 12, 14]. Childhood idiopathic intracranial hypertension has no sex predilection, and obesity is uncommon when patients approaching puberty are excluded [7, 14]. Prepubertal children usually present with stiff neck, diplopia, and strabismus [7, 14]. Papilledema may resolve rapidly with medical therapy; however, despite treatment, children can sustain loss of visual field and acuity—in one series visual acuity or visual field loss occurred in six (60%) of ten patients [14].
The association or causal relationship between idiopathic intracranial hypertension (IIH) or PTC and Chiari 1 malformation remains poorly defined. Suggestions have been made in the literature as to the possible coexistence of IIH–PTC with CM1 [4, 5, 9]. It is a possibility that IIH–PTC may cause or exacerbate CM1 or vice versa but this remains unclear. The decision to proceed to an LP in our patient without obtaining an MRI emphasizes the critical need to be aware of this relationship and the potential danger of exacerbating the underlying CM1 [8, 13]. A presumed diagnosis of benign intracranial hypertension should not be made prior to MRI.
We proceeded to surgical treatment in our patient without a trial of medication alone due to the rapid onset of visual symptoms and threatened permanent visual impairment. Urgent surgical treatment of CM1 patients is uncommon [18] and as patients usually present with acute signs and symptoms related to brainstem dysfunction and/or cerebellar compression, the procedure of choice is likely to be a posterior craniovertebral decompression [2, 7, 18]. CSF diversion has been well described as a management option for IIH–PTC [10, 19]. Lumbar peritoneal shunting is not an option for those with concomitant CM as the hindbrain herniation may be worsened. However, ventriculoperitoneal CSF shunting with a stereotactically placed ventricular catheter has been favorably reported as a management option for patients with medically refractory IIH–PTC [3, 10, 19]. Nevertheless, the complications and morbidity of ventriculoperitoneal shunts are well documented and should be avoided if possible.
Endoscopic CSF diversion—ETV—was considered a viable option as our patient only demonstrated signs and symptoms of raised intracranial pressure and if successful would preclude the need for a permanent ventriculoperitoneal shunt or craniovertebral decompression. When one is faced with a symptomatic Chiari 1 malformation without any evidence of raised intracranial pressure and normal–small ventricles, then the standard surgical treatment would be to proceed directly to hindbrain decompression. However, it is increasingly apparent that a subgroup of patients with CM1 and small ventricles may have raised intracranial pressure as a primary pathological driving force. This may be evidenced by obvious signs and symptoms of raised intracranial pressure such as in our case—the patient was initially suspected of having IIH with associated papilledema. In the more common scenario where there is patent hydrocephalus, it is conventional to manage this first before proceeding to a craniovertebral decompression. Indeed, in many instances, a craniovertebral decompression may be avoided entirely by performing a CSF diversion procedure either through an endoscopic third ventriculostomy or a ventriculoperitoneal shunt.
Arguably, if one can manage the overall condition with a single operative procedure, then the least invasive procedure, e.g., ETV should be performed. Secondly, in CM1, there may be additional risk in performing a primary craniovertebral decompression in the presence of raised intracranial pressure with or without hydrocephalus. We have noted an increase risk of CSF leaks and indeed hydrocephalus requiring shunting in patients managed initially with craniovertebral decompression when raised intracranial pressure has been missed. We therefore always screen for raised intracranial pressure in CM1 patients particularly if they have headaches which are more suggestive of raised intracranial pressure than the stereotypical occipital–neck ache of hindbrain hernia or CM1. Our patient presented only with global headache and eye signs and therefore it was deemed more appropriate to primarily manage the raised intracranial pressure utilizing a minimally invasive approach—EM-navigated ETV. A recent study from our unit has demonstrated that ETV for Chiari malformation type 1 with hydrocephalus can provide a definitive primary treatment option and avoid unnecessary craniovertebral decompression in over 50% of cases [12].
As the size of the patients ventricles was small (Fig. 2b), the patient underwent a frameless EM neuronavigation-guided ETV without any complications. No head fixation is required and the EM probe allows real-time tracking and there is no line of sight issue. The EM probe passes down the working channel of the endoscope and can also double up as the instrument for fenestration. This procedure obviated the need for a shunt or craniovertebral decompression and its inherent potential complications.
Conclusion
The successful outcome in our case highlights the technique of EM neuronavigation ETV as a safe management option in this category of patient with small ventricles and intracranial hypertension associated with tonsillar herniation and foramen magnum outflow obstruction. We believe this to be the first such reported case in either the adult or pediatric populations whereby an ETV has been successfully employed as the first-line management in an acutely presenting patient with CM1. Nevertheless, it is important to maintain regular long-term follow-up in this patient with further interval imaging to monitor the Chiari 1 malformation and the spinal syrinx.
References
Alberti O, Riegel T, Hellwig D, Bertalanffy H (2001) Frameless navigation and endoscopy. J Neurosurg 95(3):541–543
Alden TD, Ojemann JG, Park TS (2001) Surgical treatment of Chiari I malformation: indications and approaches. Neurosurg Focus 11(1):E2 Review
Azeem SS, Origitano TC (2001) Ventricular catheter placement with a frameless neuronavigational system: a 1-year experience. Neurosurgery 60(4 Suppl 2):243–247 discussion 247–8
Banik R, Lin D, Miller NR (2006) Prevalence of Chiari I malformation and cerebellar ectopia in patients with pseudotumor cerebri. J Neurol Sci 247(1):71–75
Bejjani GK (2003) Association of the adult Chiari malformation and idiopathic intracranial hypertension: more than a coincidence. Med Hypotheses 60(6):859–863
Caldarelli M, Novegno F, Vassimi L, Romani R, Tamburrini G, Di Rocco C (2007) The role of limited posterior fossa craniectomy in the surgical treatment of Chiari malformation type I: experience with a pediatric series. J Neurosurg 106(3 Suppl):187–195
Cinciripini GS, Donahue S, Borchert MS (1999) Idiopathic intracranial hypertension in prepubertal pediatric patients: characteristics, treatment, and outcome. Am J Ophthalmol 127(2):178–182
Erbay SH, O’Callaghan MG, Bhadelia R (2005) Is lumbar puncture contraindicated in patients with Chiari I malformation? AJNR Am J Neuroradiol 26(4):985
Fagan LH, Ferguson S, Yassari R, Frim DM (2006) The Chiari pseudotumor cerebri syndrome: symptom recurrence after decompressive surgery for Chiari malformation type I. Pediatr Neurosurg 42(1):14–19
Gil Z, Siomin V, Beni-Adani L, Sira B, Constantini S (2002) Ventricular catheter placement in children with hydrocephalus and small ventricles: the use of a frameless neuronavigation system. Childs Nerv Syst 18(1–2):26–29
Gumprecht H, Trost HA, Lumenta CB (2000) Neuroendoscopy combined with frameless neuronavigation. Br J Neurosurg 14(2):129–131
Hayhurst C, Osman-Farah J, Das K, Mallucci C (2008) Initial management of hydrocephalus associated with Chiari malformation Type 1–syringomyelia complex via endoscopic third ventriculostomy: an outcome analysis. J Neurosurg 108:1211–1214 (June 2008)
Johnston I, Hawke SH, Halmagyi GM, Teo C (1991) The pseudotumour syndrome: disorders of cerebrospinal fluid circulation causing intracranial hypertension without ventriculomegaly. Arch Neurol 48:740–747
Kamel MH, Mansour N, Kelleher MO, Aquilina K, Young S (2007) Association of intracranial hypertension without ventriculomegaly and Chiari malformation: a dangerous combination. Br J Neurosurg 13:1–3
Kesler A, Fattal-Valevski A (2002) Idiopathic intracranial hypertension in the pediatric population. J Child Neurol 17(10):745–748
Meadows J, Kraut M, Guarnieri M, Haroun RI, Carson BS (2000) Asymptomatic Chiari type I malformations identified on magnetic resonance imaging. J Neurosurg 92:920–926
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 44:1005–1017
Schroeder HW, Wagner W, Tschiltschke W, Gaab MR (2001) Frameless neuronavigation in intracranial endoscopic neurosurgery. J Neurosurg 94(1):72–79
Wellons JC 3rd, Tubbs RS, Bui CJ, Grabb PA, Oakes WJ (2007) Urgent surgical intervention in pediatric patients with Chiari malformation type I. Report of two cases. J Neurosurg 107(1 Suppl):49–52
Woodworth GF, McGirt MJ, Elfert P, Sciubba DM, Rigamonti D (2005) Frameless stereotactic ventricular shunt placement for idiopathic intracranial hypertension. Stereotact Funct Neurosurg 83(1):12–16
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kandasamy, J., Kneen, R., Gladstone, M. et al. Chiari I malformation without hydrocephalus: acute intracranial hypertension managed with endoscopic third ventriculostomy (ETV). Childs Nerv Syst 24, 1493–1497 (2008). https://doi.org/10.1007/s00381-008-0672-y
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0672-y