Abstract
Objectives
Even in the days of modern microsurgery, the removal of a brain stem lesion remains a surgical challenge. Especially when operating on children, the prognosis is directly related to the radicality of the resection; however, a radical resection is often associated with surgical morbidity. Intraoperative neuromonitoring could help to minimise the surgical morbidity, but few studies have been performed to clarify the value of this monitoring. We investigated a prospective series of 21 patients with lesions involving the brain stem for the prognostic value and benefits of neuromonitoring.
Methods
We performed intraoperative neuromonitoring of cranial nerve function by electromyography (EMG) and motor evoked potential (MEP). The results were correlated with postoperative neurological deficits.
Conclusions
There is a good correlation between intraoperative neurophysiological events and postoperative neurological deficits in patients with lesions of the brain stem. In general, transient, prolonged, spontaneous activity in EMG is associated with a transient paresis of the respective muscle, whereas a permanent spontaneous activity is associated with a permanent deficit. Intraoperative neuromonitoring reliably predicts postoperative neurological function in patients with tumours of the lower brain stem and fourth ventricle. This neuromonitoring guides the neurosurgeon in the operation and may decrease surgical morbidity. We recommend using monitoring of MEP and EMG of the lower cranial nerves in surgery on all patients with lesions involving the lower brain stem and fourth ventricle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Even in the days of modern microsurgery, the removal of a brain stem lesion remains a surgical challenge. Especially when operating on children, the prognosis is directly related to the radicality of the resection [1]. However, a radical tumour resection is particularly difficult in tumours of the fourth ventricle because anatomical landmarks are inconstant [2] and anatomy is often displaced by the lesion [3]. Also, the subependymal location of the caudal cranial nerve nuclei makes surgery difficult. This uncertain situation and the tight connection of many lesions with the brain stem tissue creates a significant risk for injury to the nuclei of the caudal cranial nerves. This often has deleterious effects for the patient and can result in severe disability, often tracheotomy, and may have a lethal course.
Intraoperative neuromonitoring has proven its benefits for many indications. In surgery of cerebellopontine angle tumours, the outcome regarding hearing loss and facial nerve palsy could be significantly improved by the use of intraoperative monitoring of brain stem auditory evoked potentials (BAEP) and electromyography (EMG) of the facial nerve [4–6]. Neurophysiological monitoring has become an integral part in neurovascular, cardiovascular and spinal surgery, as well as in surgery of the central region. For this reason, the use of intraoperative neuromonitoring has become a standard procedure in most neurosurgical centres (see [7–9] for a review).
Intraoperative monitoring using BAEP and somatosensory evoked potentials [10–13] have been described as tools of the surveillance of brain stem function. Cranial nerve EMG has been used for intraoperative identification of cranial nerve nuclei [14–17]. However, only two studies performing continuous intraoperative cranial nerve EMG monitoring have been published [18, 19], and one of those studies included only the sixth and seventh cranial nerve [18].
Thus, the reliability of intraoperative cranial nerve EMG monitoring is not yet well defined, especially for the lower cranial nerves. The prognostic value of intraoperative EMG events in brain stem surgery and what produces these events is not sufficiently understood, and the effectiveness of the technique in preventing postoperative neurological deficit has yet to be clarified. In the present study, we report our experience with systematical intraoperative neurophysiological monitoring in a series of 21 patients with lesions of the brain stem.
Materials and methods
Patients
All patients with lesions invading the brain stem who were operated on in our neurosurgical centre between 2000 and 2002 were included in the study. Clinical data of the patients were collected prospectively. The neurological statuses of the patients were evaluated and documented preoperatively, postoperatively and at follow-up to assess the surgical morbidity. A member of the staff who was not involved in the monitoring procedure performed these examinations. Data of the postoperative course of the patients that were related to surgical morbidity were also collected (e.g. aspiration pneumonia or tracheotomy).
Recording protocol
Different nervous structures were monitored, depending on the location of the lesion and the decision of the surgeon. Motor evoked potentials (MEPs) were obtained by high-frequency repetitive electrical stimulation, which was applied transcranially through subdermal needle electrodes placed at C3 and C4 [20]. EMG responses were recorded using pairs of subdermal needle electrodes, which were placed at the thenar and hypothenar in a belly-tendon fashion.
For EMG recordings, needle electrodes were placed in the respective muscles in a bipolar fashion. Free running and triggered EMG recordings were obtained from the masseter (CN V), lateral rectus oculi (CN VI), orbicularis oculi and orbicularis oris (CN VII), velum palatinum (CN IX), pharyngeal constrictor (CN IX and X) and the tongue (CN XII) in a bipolar technique. Stimulation for triggered EMG records was applied through concentric bipolar stimulation electrodes (Inomed GmbH, Teningen, Germany).
Intraoperative monitoring of EMG and evoked potentials was provided using the Inomed Neuroexplorer (Inomed GmbH). With this system, up to eight channels of EMG recordings could be displayed in sequential periods of 500 ms. The sampling rate was 10 kHz.
Intraoperative monitoring
All surgeries were performed in general anaesthesia, which was maintained by fentanyl, midazolam and sevoflurane. Induction of anaesthesia was performed by propofol and alfentanil. Short-lasting muscle relaxants were used for induction of anaesthesia, intubation and positioning of the patient. No muscle relaxant was used thereafter.
Burst, train and pulse patterns of EMG activity were considered significant according to established criteria [5, 6]. Short bursts were not considered pathological if they occurred at the onset or end of manipulation, and were interpreted as contact activity [6]. The same exception was made for short trains at the onset or end of manipulation [5]. Short EMG activity during direct manipulation on cranial nerves, which stopped immediately after cessation of manipulation, was also not considered as significant. Spontaneous pathological EMG activity before the beginning of the surgical procedure was registered as “primary pathological EMG activity”. In all cases of potential changes, a check was made after informing the surgeon regarding the electrode impedances, changes in the anaesthesia regimen and changes in the blood pressure and oxygenation.
Spontaneous activity in EMG was made audible to the surgeon and additionally reported. Neurophysiological changes and the reaction of the surgeon were documented. A constant exchange of information with the surgeon, regarding changes in potentials and impacts on the operation, took place and was documented. It was noted whether the information provided by neuromonitoring led to significant changes in the operative strategy.
All intraoperative neurophysiological data were stored on CD-ROM for repeated analysis postoperatively. In some cases, correlating short video sequences of the surgical process could be sampled and stored.
Statistical analyses
We used the chi-square test to investigate the statistical significance of our findings.
Results
Patient characteristics
Twenty-one patients (13 males and 8 females, age from 1 to 66, mean 37.4) who underwent microsurgical removal of a brain stem-invading lesion at our institution between 2000 and 2002 were examined. Their diagnoses, as well as neurological statuses preoperatively, postoperatively and at follow-up, are indicated in Table 1.
Surgery
In 12 patients (57%), the use of intraoperative neuromonitoring led to a change in the operative strategy. In most patients, this was reversion of retraction, irrigation and continuing surgery at a different site until the neurophysiological recordings returned to normal. Under the guidance of neuromonitoring, macroscopically complete resections were possible in 18 patients (86%). In the other patients, the use of neuromonitoring led to the decision of performing a subtotal tumour removal to preserve neurological function.
Prognostic value of neuromonitoring
The results of neuromonitoring are summarised in Table 1. In general, there was a high correlation between monitored intraoperative events and postoperative neurological function. Altogether, a transient or permanent pathological activity associated with an attributable postoperative deficit (i.e. true positive event) was observed 17 times. A transient pathological activity without an attributable deficit (i.e. false positive event) was observed eight times. A new postoperative deficit without an intraoperative change in the corresponding potential (i.e. false negative event) was observed only once. Forty true negative events were observed. Table 2 lists the correlation between intraoperative neurophysiological events and postoperative neurological deficits. The correlation of intraoperative neurophysiological events with postoperative deficits was statistically significant (p<0.05).
The postoperative clinical course was complicated by aspiration pneumonia, tracheotomy or both in five patients. In all patients, there was an intraoperative activity of at least one of the EMGs of the nerves IX, X or XII.
Discussion
Interpretation of changes in potentials during intraoperative neuromonitoring is only possible on the basis of data on experience. However, this experience is very limited in surgery of lesions of the brain stem [10–12, 14], especially for EMG. In the present study we report our findings in a series of 21 patients with brain stem lesions.
Surgery
The most critical point during surgery was, in most patients, the dissection of the tumour from the floor of the fourth ventricle. In small, circumscribed infiltrations of the floor of the fourth ventricle, direct stimulation was helpful in the identification of motor nuclei. Our impression was that for the stimulation of an intact motor nucleus in the rhomboid fossa, a current of 0.1 to 0.2 mA should be enough to result in full response. With higher currents, the determination of the location of a nucleus becomes inaccurate. These observations are in agreement with the observations of Strauss et al., who have identified the motor nuclei of cranial nerves by direct stimulation in ten patients [14]. We found that intraoperative direct stimulation of the rhomboid fossa was important, and one should not wait for spontaneous EMG activity when dissecting in proximity to a motor nucleus.
In larger lesions, however, with more extensive brain stem involvement by direct infiltration or even adhesion, spontaneous EMG activity can occur by indirect manipulation, even further away from the nucleus.
The adequate reaction to a significant change in monitored potentials is not defined for brain stem surgery. It has been shown that intermittent retraction causes less damage to brain structures than continuous retraction [21]. Therefore, the surgeon usually reacted by release of retraction. Additionally, the potentially injured structure was irrigated with ringer solution at 37°C and the dissection was continued at a different site of the lesion. This was usually enough to make the potentials return to normal.
Other groups have reported observing interfering effects of anaesthesia [22, 23]. However, with the methods described here, we have not had major problems with this. It has to be made sure that muscle relaxants are only administered for induction of anaesthesia and that the blood pressure stays at a constant level. One should, however, always keep in mind that changes in electrophysiological activity could be a result of changes in anaesthesia, and thus, good communication with the anaesthesiologist is crucial.
Prognostic value of neuromonitoring
The correlation of intraoperative neurophysiological changes with postoperative neurological deficits is a major concern of research on neuromonitoring. When discussing sensitivity, specificity and predictive values of neuromonitoring, it should be realised that, in intraoperative neuromonitoring, a false negative result is much worse than a false positive result. A surgically caused neurological deficit without previous warning by neuromonitoring is much more deleterious than an observed activity without a correlating postoperative deficit. However, if false positive results occur too often, it could result in decreased credibility of the method. In general, the meaning of a false positive result is a matter of debate in neuromonitoring. There is a difference between expecting neuromonitoring to inform us about the intraoperative manipulation of a nervous structure and expecting neuromonitoring to inform us about an imminent postoperative deficit. In this study we have correlated intraoperative prolonged spontaneous activity with postoperative deficits, whereas short intraoperative activity was interpreted as a warning for imminent injury. The results are summarised in Table 2.
MEP showed a good correlation between intraoperative neurophysiological events and postoperative deficits. However, we only observed one positive event with the use of MEP in the present study, which was correlated with a postoperative hemiparesis. The rare occurrence of MEP events certainly is due to the fact that, in the present series, the motor tracts were not directly related to the lesion. On the other hand, we did not observe false positive results in the 12 monitored patients, indicating that the use of MEP is reliable in brain stem surgery. Considering this, we conclude that MEP can be useful in cases where motor tracts are in proximity to the lesion.
EMG events showed, in general, a good correlation with postoperative neurological status. The EMG of the caudal cranial nerves (IX, X and XII) especially resulted in a good reliability. A positive intraoperative EMG event in one of the nerves resulted in a postoperative deficit in 73% of the patients, and temporary spontaneous activity of all three nerves was always associated with a postoperative deficit. Postoperative aspiration pneumonia or tracheotomy was always associated with intraoperative spontaneous activity in one of these nerves. Thus, although some false positive results occurred, the EMG of these nerves can give us important information about the postoperative neurological status. In case of a positive event, the extubation should be handled with great care, and special attention should be paid to the pharyngeal reflexes (Fig. 1). Regarding the fact that EMG activity of these nerves was often associated with aspiration pneumonia and tracheotomy in the postoperative course, a delayed extubation should be considered in patients with positive intraoperative results, i.e. prolonged spontaneous activity. An uneventful monitoring of all caudal cranial nerves, however, guaranteed good pharyngeal reflexes in the present study.
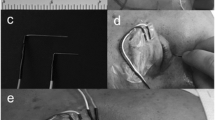
Illustrative case: This 20-year-old man (patient 3, Table 1) presented with vertigo and headache. Contrast-enhanced MRI (a) revealed a cystic, contrast-enhancing lesion at the craniocervical junction, suggestive for a pilocytic astrocytoma involving the floor of the fourth ventricle and occlusive hydrocephalus. Intraoperatively, the tumour was well delineated and imbedded in the vermis, but demonstrated to be strongly adherent and even infiltrating the floor of the fourth ventricle. An early, postoperative, contrast-enhanced MRI exhibited complete tumour resection (b). Intraoperative neuromonitoring was performed and revealed recurrent transitory prolonged spontaneous EMG activity in cranial nerves 10 and 12 (c). After pausing and irrigating with 37°C ringer solution, the spontaneous activity decreased (d). Postoperatively, the patient exhibited transitory gait ataxia, singultus and a slight tongue deviation. These deficits completely disappeared after 2 months
Altogether, the absence of pathological activity in all monitored structures was a reliable indicator of a stable neurological status. We observed only one false negative event in the whole series. In patient 9, a postoperative abducens paresis was observed without intraoperative electrophysiological warning. The reason why neuromonitoring failed to detect the injury in this case remains unclear. Possibly, the injury was internuclear and, thus, undetectable.
Certainly, more important than predicting the postoperative neurological status is avoiding a neurological deterioration. By correlating the intraoperative neurophysiological changes with the surgical morbidity, we have shown that monitoring is a reliable indicator for postoperative deficits. But we can hereby certainly not prove that the use of neuromonitoring has helped prevent surgical morbidity in brain stem surgery. However, we believe that our observations of (1) temporary spontaneous activity, being usually associated with temporary postoperative deterioration, and (2) that reaction to changes by reversion of retraction, irrigation and continuing surgery at a different site usually made potentials return to normal are highly suggestive that, in many patients, permanent neurological damage was avoided by the use of intraoperative neuromonitoring. A study in which the surgeon would not react to the intraoperative changes in half of the patients would result in ethical problems. This type of double-blinded study is not found in the literature of neuromonitoring, because surgeons who have experienced the increased feeling of security provided by neuromonitoring are reluctant to deprive their patients of the benefits from an aid to the operation that surgeons believe can improve the operation’s outcome [24].
Benefits and limitations
In the present study we have shown that intraoperative neuromonitoring is a reliable indicator of neurological function in brain stem surgery. In case no pathological activity is observed, a new postoperative neurological deficit is very unlikely, as our results show. There can be potential benefits of neuromonitoring for the patient by (1) giving the surgeon a secure feeling and (2) encouraging the surgeon to perform a more radical resection. In cases where the surgeon experiences pathological activity, there can also be a learning effect by demonstrating to the surgeon which steps of the manipulation lead to a neurological deficit. Thus, the use of neuromonitoring is beneficial for the patient and for the surgeon. Direct stimulation of motor structures helps the surgeon to understand the anatomy, which is difficult, especially in the floor of the fourth ventricle [3].
We have observed that the use of intraoperative neuromonitoring in brain stem surgery, if well prepared and coordinated, is easily available and does not cause significant delay. As observed by others [14], we agree that the method is not associated with side effects by needle placement and stimulation.
Also, in brain stem surgery, neuromonitoring certainly has its limitations and dangers. First, it has to be noted that not all structures or functions of the brain stem can be monitored. We have observed irritation of the breathing centre in patient 1 and cerebellar signs in patient 14. No monitoring for these functions is known so far. We have furthermore experienced that, in patients with primary pathological EMG activity, a further intraoperative injury can possibly be unrecognised. Although it sounds trivial, it has to be considered that irritations can only be detected in structures that are actually monitored. Thus, a proper selection of the monitoring setup has to be performed preoperatively to get an optimal result. When dissecting on the floor of the fourth ventricle, we recommend using intermittent direct stimulation when possible rather than relying on spontaneous EMG activity because the EMG warning can occur just at the moment when the respective structure is injured. In the setting of the operating room, communication between the neurophysiologist and the neurosurgeon could also be a possible limitation of neuromonitoring. Only good communication can tap the full potential of neuromonitoring.
The use of intraoperative neuromonitoring in brain stem surgery, if applied and interpreted correctly, might contribute to increased safety and lower surgical morbidity. Furthermore, the technique could lead to more radical removals of lesions of the brain stem. This is especially true when operating on children because the prognosis is directly related to the radicality of the resection [1]. We have also shown that the method has a significant prognostic value, which can also have consequences for treatment. We suggest that the use of intraoperative neuromonitoring should become a standard in brain stem surgery. Correct and experienced interpretation of the data and a surgeon willing to alter his or her procedure according to the neurophysiological observations are necessary presuppositions for effective use of intraoperative neuromonitoring. However, further studies have to be performed to gain more experience with the interpretation of the intraoperative neurophysiological data in the surgery of brain stem lesions.
References
Pollack IF, Gerszten PC, Martinez AJ, Lo KH, Shultz B, Albright AL, Janosky J, Deutsch M (1995) Intracranial ependymomas of childhood: long-term outcome and prognostic factors. Neurosurgery 37:655–666 (discussion 666–667)
Lang J Jr, Ohmachi N, Lang J Sr (1991) Anatomical landmarks of the rhomboid fossa (floor of the 4th ventricle), its length and its width. Acta Neurochir (Wien) 113:84–90
Fahlbusch R, Strauss C (1991) Zur chirurgischen Bedeutung von cavernösen Hämangiomen des Hirnstammes. Zentralbl Neurochir 52:25–32
Radtke RA, Erwin CW, Wilkins RH (1989) Intraoperative brainstem auditory evoked potentials: significant decrease in postoperative morbidity. Neurology 39:187–191
Prass RL, Luders H (1986) Acoustic (loudspeaker) facial electromyographic monitoring: part 1. Evoked electromyographic activity during acoustic neuroma resection. Neurosurgery 19:392–400
Prass RL, Kinney SE, Hardy RW Jr, Hahn JF, Luders H (1987) Acoustic (loudspeaker) facial EMG monitoring: II. Use of evoked EMG activity during acoustic neuroma resection. Otolaryngol Head Neck Surg 97:541–551
Sala F, Krzan MJ, Deletis V (2002) Intraoperative neurophysiological monitoring in pediatric neurosurgery: why, when, how? Childs Nerv Syst 18:264–287
Moeller A (1995) Intraoperative neurophysiologic monitoring. Harwood, Luxembourg
Deletis V, Shils J (2002) Neurophysiology in neurosurgery — a modern intraoperative approach. Academic, Amsterdam
Legatt AD (2002) Mechanisms of intraoperative brainstem auditory evoked potential changes. J Clin Neurophysiol 19:396–408
Shchekut’ev GA, Lubnin A, Barkalaia DE, Sogomonian SA (1994) Monitoring of short latent evoked potentials during brain stem surgery. Anesteziol Reanimatol (5):48–52
Fahlbusch R, Strauss C, Huk W, Rockelein G, Kompf D, Ruprecht KW (1990) Surgical removal of pontomesencephalic cavernous hemangiomas. Neurosurgery 26:449–456 (discussion 456–457)
Wiedemayer H, Fauser B, Sandalcioglu IE, Schafer H, Stolke D (2002) The impact of neurophysiological intraoperative monitoring on surgical decisions: a critical analysis of 423 cases. J Neurosurg 96:255–262
Strauss C, Romstock J, Nimsky C, Fahlbusch R (1993) Intraoperative identification of motor areas of the rhomboid fossa using direct stimulation. J Neurosurg 79:393–399 (comment)
Morota N, Deletis V, Lee M, Epstein FJ (1996) Functional anatomic relationship between brain-stem tumors and cranial motor nuclei. Neurosurgery 39:787–793 (discussion 793–794)
Morota N, Deletis V, Epstein FJ, Kofler M, Abbott R, Lee M, Ruskin K (1995) Brain stem mapping: neurophysiological localization of motor nuclei on the floor of the fourth ventricle. Neurosurgery 37:922–929 (discussion 929–930)
Katsuta T, Morioka T, Fujii K, Fukui M (1993) Physiological localization of the facial colliculus during direct surgery on an intrinsic brain stem lesion. Neurosurgery 32:861–863 (comment 863)
Grabb PA, Albright AL, Sclabassi RJ, Pollack IF (1997) Continuous intraoperative electromyographic monitoring of cranial nerves during resection of fourth ventricular tumors in children. J Neurosurg 86:1–4
Eisner W, Schmid UD, Reulen HJ, Oeckler R, Olteanu-Nerbe V, Gall C, Kothbauer K (1995) The mapping and continuous monitoring of the intrinsic motor nuclei during brain stem surgery. Neurosurgery 37:255–265
Pechstein U, Cedzich C, Nadstawek J, Schramm J (1996) Transcranial high-frequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 39:335–343 (discussion 343–344)
Yokoh A, Sugita K, Kobayashi S (1983) Intermittent versus continuous brain retraction. An experimental study. J Neurosurg 58:918–923
May DM, Jones SJ, Crockard HA (1996) Somatosensory evoked potential monitoring in cervical surgery: identification of pre- and intraoperative risk factors associated with neurological deterioration. J Neurosurg 85:566–573
Szalay EA, Carollo JJ, Roach JW (1986) Sensitivity of spinal cord monitoring to intraoperative events. J Pediatr Orthop 6:437–441
Moller AR (1995) Evaluating the benefits of intraoperative neurophysiological monitoring. Harwood, Luxembourg
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gläsker, S., Pechstein, U., Vougioukas, V.I. et al. Monitoring motor function during resection of tumours in the lower brain stem and fourth ventricle. Childs Nerv Syst 22, 1288–1295 (2006). https://doi.org/10.1007/s00381-006-0101-z
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-006-0101-z